By Sophie Faught
MindFreedom International Communications Coordinator
As part of its I GOT BETTER campaign to challenge hopelessness in mental health care, MindFreedom International conducted a two-part Hope in Mental Health Care Survey from June to October of this year. The survey was designed to gather answers to these three questions:
1. How prevalent are messages of hopelessness in mental health care?
2. What are the sources and contents of these messages?
3. What is the veracity of these messages? In other words, do hopeless prognoses and statements about recovery, medication use, etc. generally prove true or false?
Well over 1000 individuals participated in the survey, contributing their experience, wisdom, and opinions to a growing body of knowledge about recovery from mental and emotional distress. In this and forthcoming blogs, we’ll be sharing the major findings that emerged from our analysis of the survey data.
(You can download the final survey report that outlines survey methods, characteristics of the survey sample, and all findings here.)
The mental health system itself is the most common source of messages of hopelessness.
Respondents to part two of the survey who had received a psychiatric diagnosis (n=390) overwhelmingly pointed towards the mental health system as the source of messages of hopelessness:
Furthermore,
- 64% were never told by a mental health provider during their mental health care that recovery from their mental/emotional problem was possible, and 41% were actually told by a mental health provider that recovery was impossible.
- 76% were told by a mental health provider provider that they would have to take medications for the rest of their life.
- 49% were specifically told by a mental health provider that they could not reach a personal goal (for example, education, career, independent housing, relationship, children, etc.) because of a psychiatric diagnosis.
The frequency of hopeless messages was even greater for individuals with diagnoses of schizophrenia and bipolar disorder.
Were these messages of hopelessness true?
Looking again at respondents with diagnoses of schizophrenia and bipolar disorder (described by the American Psychiatric Association as “serious mental illnesses”* and frequently assigned an extremely negative prognosis in the medical literature), we see that often these messages of hopelessness were unwarranted.
Almost 2/3 of respondents with these diagnoses who were once told recovery is impossible described themselves as “recovered.”
- Diagnosis of Schizophrenia (n=94): 59% were told by a mental health provider that recovery was impossible. But of these individuals receiving such a negative prognosis, 90% said that they had “experienced at least some recovery from a mental or emotional problem,” and 66% ranked themselves as “recovered” or “fully recovered” (equivalent to a ranking of 8, 9, or 10 on a 10-point recovery scale).
- Diagnosis of Bipolar Disorder (n=196): 51% were told by a mental health provider that recovery was impossible. Of these individuals, 91% said that they had “experienced at least some recovery from a mental or emotional problem,” and 60% ranked themselves as “recovered” or “fully recovered.”
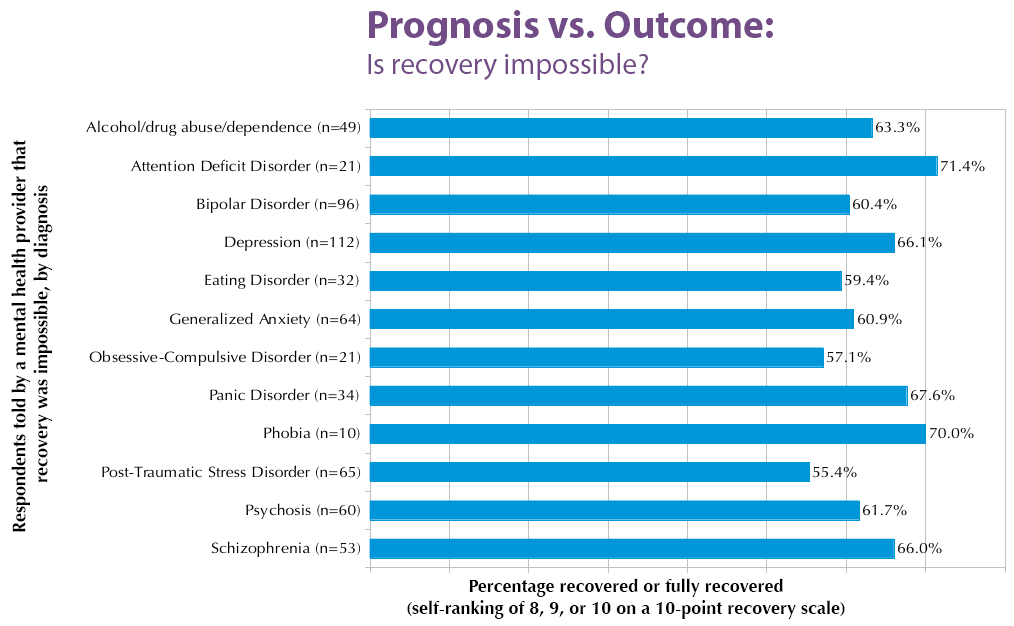
The same trend continues across the board, for every diagnosis. A significant percentage of individuals once told by mental health providers that recovery is impossible describe themselves as “recovered” or “fully recovered”:
This vast disconnect between prognosis (as predicted by mental health providers) and actual outcome (as reported by psychiatric survivors) forces us to ask the question: Why send messages of hopelessness when they are so often untrue?
A different message
MindFreedom International’s I GOT BETTER campaign is about sending a different kind of message, one of hope and human possibility.
You can see some of those possibilities in our collection of videoed stories of triumph over psychiatric adversity (see these written stories, also). And if you have a story to share, we encourage you to do so. We want to compile a body of knowledge to counter the narrative of hopelessness, to show that there are diverse ways to achieve balance after mental or emotional distress.
There are many ways to mental and emotional wellness. What’s yours?
* American Psychiatric Association (2012). Schizophrenia. Retrieved from http://www.apa.org/topics/schiz/index.aspx; American Psychiatric Association (2012). Bipolar Disorder. Retrieved from http://www.apa.org/topics/bipolar/index.aspx.
















Regarding “There are many ways to mental and emotional wellness. What’s yours?”
If you don’t complain, they can’t “help” you. If there is no problem, then there is no need for a solution.
Report comment
There is definitely a problem. When “they” try to “help” you, they will write you a prescription. They are not willing to look at other options which may be a lot better.
Sadly I had to do a lot of research on the internet to find the solution to my problem, which the psychiatrist should have had.
Report comment
I am a person who has been abused by Mental Health System esp. in Georgia. I have been told there was no hope for me to ever become any better much less be functional in a job or ever be able to function as a human in relationships. and I have been told I had so many diseases bipolar, schizo-affective, schizophrenia and so many others. I have none of those diseases I was abused in every way for most of my life and was given medications to shut me up. If I talk I tell the hidden secretes-they gave me enough medications I drooled all over my clothes never knowing I was in this world. and I went to a trauma center in another state which helped me understand my feelings and shows me hope that I can become whole again and function as someone who could work and function better than I ever had. I was a survivor. I like all humans struggle with daily life issues and have gotten off 2.5 legal sized pages of medication and now taking 1 mental health medication. The program I was in tried to get me to sign papers to give them all my money I had while I was drugged up. Stealing isn’t what they were trying to do were they?
Report comment
Congratulations for finding that trauma center and for finding your way back to health and well-being! Yes, you are a survivor and that’s a tremendous accomplishment on your part. You survived because of your own abilities and talents and gifts.
Report comment
My son was not only told that he was mentally ill, that there was no cure, that he will be on drugs for life and that he will get worse if he stops taking the meds, he was literally taken aside by the medical staff and brainwashed into believing it behind my back, because the doctors and nursing staff knew that I disagreed with them.I had to painstakingly undo their “good” work every time he came home from an appointement.
Report comment
There is no cure, meds for the rest of your life, you will get worse if you stop…the exact same things I was told. When I started looking at diet as a cause of the problem I was told, “that is a symptom not a cause”. That made no sense to me, so I did a lot of research. Took me almost three years but I finally found that what I needed was less processed food and more whole fruits and vegetables. I made a few simple changes in my diet and the last ten months have been the best of my life.
I hope this little suggestion might help with your son.
Report comment
“Why send messages of hopelessness when they are so often untrue?”
Why indeed. Cui bono? Who benefits from these messages of hopelessness? The person hearing the message? Seems unlikely in most cases. The person delivering the message? Intentionally or not, we have to acknowledge the “job security” of telling someone they will require our services…for the rest of their life! Does the pharmaceutical industry, APA and other groups benefit? I think we know the answer. How about the broader culture? Does the broader culture somehow benefit from knowing that those who act “differently” can be identified/labeled and “treated” for life?
I think the results of the survey also speak to the incredible resiliency of survivors. In the face of multiple messages designed to influence them, they don’t buy it. People recover in spite of the help they receive. What would happen if we actually gave them what they wanted?! Shock. Horror.
Report comment
This is just great. Anyone who hasn’t, reading Paris Williams’ Rethinking Madness puts across the same message: lots of people do “recover” from “psychosis,” and if you just ASK such a person what went on, what helped and hindered, you get lots of good information. Williams extensively interviewed six people who had fully “recovered” from long term “psychosis.” They said what helped them was accepting, supportive relationships, regaining a sense of hope, of meaning, and of their own being alive with important feelings, thoughts and ambitions. And – no big surprise – they saw just about all of psychiatry as opposing the things that helped them, with the same messages discussed in this blog and responses.
Thank you to MindFreedom for this project – it is tremendously important. We need a lot more like it. Someday the public and the “mental health” industry will get the idea that if you want to know about mental problems, you really ought to ASK people with lived experience what it is like, what helps and what doesn’t.
Report comment
I find this article frustrating. As the director of a mental health program, we work hard to push recovery. We use all kinds of methods to help people see their movement toward recovery. It frustrates me that the article paints mental health providers as culprits, when I would guess, in increasing numbers, we are using a recovery focus.
It is also frustrating that it happens. Because I do believe it does.
But I fear this article oversimplifies the issues. And I think for those who don’t know what is happening on the good side of the equation, this article is misleading.
I have suffered with anxiety since childhood. I have learned to deal with it using CBT tools. I always tell my clients, things can get better. And a lot of what I tell them is that it is my job to help them develop the tools so they can do it themselves, so they are not so dependent on a counselor or medications.
At any rate
a downer article in many respects
but one that should be a wake up call to counselors and programs who are not working out of a recovery mode.
Report comment
Hmm, maybe if recipients of mental illness services were told the truth, i.e. that there is no brain disease that can be fixed by chemicals, they are not sick, and the only thing mental illness workers can do is listen, maybe they could move away from the learned helplessness that the oppressive medical model instills in them.
Kinda krazy to teach recovery skills for fictitious diseases. No wonder you are frustrated. Maybe you could teach skills for coping with systemic oppression, say upfront that it’s about learning to live with impossible, unfair crap, not about managing disease symptoms.
Report comment
love this reply.
Report comment
Me too, I think dragonfly’s is an excellent reply.
The question is what is meant by “recovery”. Danish “Capital Region Psychiatry”, i.e. the psych system in the Copenhagen area, recently came up with an interesting concept that everybody is totally mesmerized by: Illness Management Recovery. Uh, wait a minute, WHAT?! you may ask. Yup, you got that right: Illness Management Recovery. In one breath. Finally, psychiatry officially acknowledges that recovery is possible, and Capital region Psychiatry now even pushes for recovery, hooray! Or does it?? Let’s be honest, “illness management” on the one hand, and “recovery” on the other are mutually exclusive. It can only be either or. Not both and. But any such criticism is immediately, and often successfully, stifled by the argument that recovery is “deeply personal” (cf. Anthony), so nobody has a right to define what it actually is except for the person experiencing it. While the mh system of course sees to that all the deeply personal definitions of recovery it quotes are those of “insightful patients”, i.e. people who’ve internalized the mh system’s definition of recovery — so much for “deeply personal”… — as meaning “living a satisfying, hopeful, and contributing life even with limitations caused by the illness.” (cf. Anthony). If that’s recovery then what to call it when people actually end up “living a satisfying, hopeful, and contributing life” without any “limitations caused by” any “illness”, as it clearly falls beyond Anthony’s/the mh system’s definition of recovery? Well, I never really liked the term “recovery” anyways, since I don’t quite see how it fits in where there was no illness to begin with.
Report comment
Me too! Kudos! Much better than mine!
Report comment
Brilliant reply, wish I could word things this good!!!
I love those so called recovery services, all they did was to tell me that I needed to recover from forced medication side effects. They were going to teach me to cook and clean, because they noticed I wasn’t!! When you are sleeping 22 hours a day and can barely move the other two hours, is it any wonder you don’t do anything!!?? But it was my fictional brain disease that caused me to do these things, the medications were just treating it!!! Amazing how I have recovered ALL functional abilities now that I am off medication!!! Yet even suggest lowering the dose of medication and so called recovery services tell you how dangerous that is, that you don’t understand the seriousness of your condition that you will die without them, etc. These were services who believed in my ability to live outside the hospital, not to do anything else. I certainly was not able to recovery to the point of a cure, no that was just wishful thinking. And of course can’t forget about there need to teach me how to “think properly”. Because I didn’t think like them I was defective with thinking and needed CBT classes to teach me how to think!!!
The only people who need to recover, to think properly or the like is the mental health system itself!! I do worry sometimes (not!!) about how they are going to cope when they discover how wrong they were. Who is going to be there to help them. Maybe they can take some coctails of drugs to help them with it. That would be a very good use for them!!!!!!!!!!!!!!!!!!!!!!!!!!!!
Report comment
spkliewer,
It is great what you are doing, and we need much more of it. Unfortunately, there are a lot more programs and professionals out there who absolutely do NOT work as you do, and they dominate the field. I think this is particularly true for people labelled with “serious mental illness” – it seems professionals are so desperate to promote
“medication compliance” that they lay it on thick about chronic brain-based disease, medication for life, etc. The medical model’s message is much rosier for other labels like “depression,” “adhd” or anxiety. TV ads don’t stress the broken brain or drugs for life themes for these labels – they show scenes of people having a lovely time. This could be seen as much more encouraging, but it is also insidious, inducing people to take drugs that can be medically dangerous, can cause anxiety, agitation, aggression, psychosis, addiction and suicide.
In my 15 years experience, there are a lot more professionals who think, once they’ve labelled someone with a diagnosis or two, that they’ve described the person; his/her history, relationships, aspirations, strengths, dreams and resources are largely ignored. So many professionals do this unconsciously, not aware of how they have discounted the person. At some level, people know when they are truly respected – and being in the presence of a professional who does not respect you is an excellent way to be drained of hope.
Report comment
spkliewer, do you have any statistics regarding how many mental health programs are operating on a recovery model? How many mental health providers?
Such numbers would be very helpful to assess how widely the recovery model is used.
Report comment
One has to be able to define what recovery means first, and it usually means being medication complaint and understanding the limitations of your illness. Once you have done those things you are allowed to have some semblance of a life.
When I discussed lowering, not withdrawing just lowering dosages of medication the immediate response from EVERYONE was “you do want to be able to keep recovering don’t you”. One cannot recover without being on medication for life. One cannot recover without acknowledging that they have a life long brain disease. Sorry but saying I have some fictional life long brain disease and will need to take mind numbing drugs for life is not and never has been recovery.
Report comment
Key words. Wake up call to counselors and programs who are not working out of a recovery mode.
The approach is what matters so people can listen into their own wisdom & develop ways that support their self-efficacy, and connect to a community with unique contribution & courage.
Report comment
Many programs and institutions may use the word “recovery” but do not promote it in any way, shape, or form. For instance, at the institution where I work the word “recovery” is the predominant word in the mission statement. However, the only treatment forced upon the people labeled as “mentally ill” is the toxic drugs. If you don’t take your drugs the psychiatrists take you to court and get you committed for another 45, or 180 days. If you signed yourself in voluntarily and try to leave, almost every time you are told you cannot leave and a psychiatrist on call will state that you’re a danger to yourself,and or, others; consequently you can’t leave! Your wish to leave is a sure sign that you’re ill! I love their way of thinking. Recovery is paid lip service to but is not encouraged at all and is defined by what the psychiatrist on the units decide will be considered recovery. There are no choices of treatment, there is no discussion of how one gets one’s life back, there is only the toxic drugs and people telling you that the only way you’ll get better is by taking the right combination of drugs, for all the rest of your life! It is the biggest bunch of hypocrisy I’ve ever witnessed in my entire life. It’s extremely easy to talk the talk for words are cheap. It’s another matter entirely to walk the walk and actually support people in their own individual understanding of what recovery is for them. Recovery is as individual and unique as each and every person pursuing it. The only expert on a person’s life is that person herself or himself, not any pseudo professional who knows little about forming enriching and caring human relationships which help people find the beginnings of their recovery.
Personally, as a person with lived experience of the so-called “mental health system” and as a peer worker in a large psychiatric institution, I stand behind what this article states. I told the psychiatrist assigned to me when I was locked in the very institution I now work in that I was not “sick” and that I would only listen to him if he made sense to me. He called me impertinent and I laughed and told him to get used to it! This article speaks the truth and reality of what the system is doing to people, plain and simple.
Report comment
Where I live “Recovery,” seems to be written what all workers have to say to and about clients but the “treatment,” offered hasn’t changed. It’s still drugs and a patronising chat with a worker once a fortnight if you are, “Critical,” and drugs and no one to talk to if you are relatively stable.
If you’re having a crisis they’ll send a worker round everyday, or even more than once a day, to make sure you’ve taken the pills because it is cheaper than taking someone into hospital – you don’t get a choice about that even if the people you’re living with are driving mad.
If your fairly stable but having a bit of relapse they’ll send the crisis team round to ask you to go for an assessment at the hospital and if you don’t turn up they send the police round.
Report comment
I think I can see where you’re coming from…in the treatment you received and provided there was a message of hope. I think that we all agree that’s a positive thing.
The survey was needed to highlight that some other people’s experiences are different. In the “treatment” I received, I basically didn’t get to speak to people…they were not interested in any form of therapy, and the only message was literally verbatim from the survey findings above.
I think the article is designed not to be a “happy” one, it’s not a “happy” situation I and many others, found themselves in and it’s important that such experiences are acknowledged, even if they make people uncomfortable.
I find the silver lining in the “I got better” side of this story, these are the real life experiences of people who didn’t take a message of hopelessness at face value, and fought back – does it get more uplifting than that??
Report comment
Recovery mode? My board-certified psychiatrist told me almost from day 1 that my depression was “genetic,” and that I would always have it. He said I needed medication for life, that there was no cure, and that I would have to visit him monthly, which I did for many years, believing there were no other avenues to wellness.
He refused to consider a referral for therapy, telling me that I was “not a good candidate for therapy” and that all I really needed was medication.
He kept me on SSRIs and Xanax for over a decade, telling me that my brain needed them like a diabetic needed insulin.
Even my pharmacist was alarmed that I was on a benzo for so many years when the PDR and other texts don’t recommend it for long term use.
When I became more agitated, depressed, obsessed with suicide and tormented by insomnia he blamed the “disease” and increased my dosages until I ended up in an ER.
He would not help me discontinue these meds and said I simply needed a different pill or a different dose.
I fired him and then put myself into recovery mode, weaning myself off of those pills using a taper method found on the web.
No more meds and no more psychiatrists. I don’t trust them. And I’m doing pretty well.
Report comment
I am glad you are out there, doing good recovery work. But I am afraid you are more in the minority than you may believe. I have been a mental health practitioner and advocate in the field for over 25 years. It did not surprise me one bit to read that three quarters of the time, a mental health professional is responsible for telling their client that recovery is unlikely or impossible. That may be changing a bit today, but if it is, that movement is in its infancy and it remains to be seen if it becomes “mainstream.” I just know that when I talk real recovery talk in mental health planning meetings, the room often becomes quiet and the subject is quickly changed in most settings. Client empowerment makes most clinicians very uncomfortable.
I have also heard the message repeatedly that “recovery is possible IF you follow your medication regime.” I do not consider that a recovery message at all. It is an implied message of hopelessness – you can only recover if you accept that your brain is broken and that your distress is a meaningless expression of genetic inadequacy.
Recovery, in my view, has to be defined by the client. Medication may or may not play a part in it, at the client’s discretion. Defining the issue as a “mental illness” or a normal response to life’s difficult circumstances should also be at the client’s discretion.
Most mental health clinicians I have known do not subscribe to these principles, even when they talk about “recovery” and sincerely mean it. The majority seem to believe the client’s brain is broken, and they convey that to the client, directly or through their behavior.
I believe the statistics are an accurate reflection of most people’s experience with the mental health system. It is not an overly negative spin – it is the truth.
—- Steve
Report comment
All. You should read the work of Paul Levy:
http://www.awakeninthedream.com/wetiko/
After reading a bit of his work I have come to realize that we are a small part of all things going on right now (not just in mental health care). The only way forward as I see it is if we become a compassion-movement. Not only compassion for ourselves but also for the very people we are pretending to fight against.
I fact, the Wetiko theory can explain the theory of why there is a growing number of people with mental health problems.
Report comment
One of the reasons why people remain hopeless is because people who believe recovery exists (because they are recovered) are fighting an uphill battle trying to advocate services & the change in the way delivery of services are offered in an effort to increase the value of the person in recovery. Some services are business run, and even though they state that consumer driven services are pivotal to their core values, funding criteria still needs to be met. And this is the business model, which – interferes with the way in which management tend to think when they come to talk with their coal-face workers. I got better, but management don’t want me too better, otherwise how will they cope with the change that brings about?
Report comment
David Ross makes a good point. Considering the effort made by the mental health system
to keep people down, it requires extraordinary resilience to recover. The recovery rate would be much higher if they were not emotionally assaulted by the mental health system. And then imagine if clients were actually helped! My first book and my recent book describes the stories of people who recovered FROM the mental death system. They get out of the system and off psychiatric drugs.
Spkliewer is angry that people are critical of the system. He acknowledges that maybe sometimes it does discourage people, but that does not bother him as much.
Do you think Spkliewer, the patients lied? They’re paranoid? As a renegade psychologist I can tell you they are right. The study understates the problem! Hopelessness as Dragonfly point out is intrinsic to the system, to the psychiatric model that is used all over. The DSM is based on an epistemology of degradation, an ontology of deficiency. In other words, from its perspective, to understand the Other I must subsume her under a rhetoric of deficiency, I must regard nher with disdain and pity. Does the DSM encourage awe and wonder and marvel at the mystery of the Other? Is there one word in the DSM Spkliewer that even suggests the Other might be worthy of awe of reverence—even as a soul that has not realized her potential.
And look at the ontology of flaw. Her existence is blighted. Is there any suggestion that there may be light, radiance, beauty, dignity at the heart of her existence—that she is created in the image of God? Even unrealized potential— obstacles to be overcome on the hero’s journey.
The survey is brilliant but it needs to be supplemented by philosophical analysis—as I just sketched out. Then we see the problem. Hopelessness is INTRINSIC to the ideology of mental health/illness. But please see my recent book. Because the Mad Pride movement at its best shows the way out. We need to look at madness as a gift. Thus my book is The Spiritual Gift of Madness: The Failure of Psychiatry and the Rise of the Mad Pride Movement.
http://www.amazon.com/Spiritual-Gift-Madness-Psychiatry-Movement/dp/159477448X/ref=sr_1_1?s=books&ie=UTF8&qid=1356867151&sr=1-1&keywords=farber+gift
David Oaks BTW is in both books.( Sascha DuBrul is in last one as is Paul Levy, mentioned below).
It’s admirable Spkliewer that you convey positive expectations to clients. But like an ostrich you’re hiding and instead of facing the facts you berate the messenger! How can you be so oblivious? Are you in Shangrai-la? Have you not read the DSM—the Bible of Psychiatry? If you get paid for your work you use it—so I’m wondering what’s going on. The survey is not misleading. I got my PhD in the mid-80s and the system has gotten far worse. It’s revealing that to prove your point Spkliewer you refer to anxiety! But who is marked “anxiety disorder.” ? That’s a tiny caste at the top. The majority in the system are relegated to the lower castes– those labeled “mentally ill. ”
You are on the MIA blog now. You have no idea what is in Bob’s books You blame Mind Freedom and claim they are misleading and simplistic, but YOU are being irresponsible.. 2 million children and youth are on psychiatric drugs. Most of them will never get off. They will be warned to stay on the “meds.” Their lives will be ruined. And you say Mind Freedom oversimplifies. You don’t say your name or where you work. What are you hiding? ? You are either being disingenous or you are deceiving yourself. And you are being irresponsible. Read Anatomy of an Epidemic by Robert Whitaker.
As Dragonfly puts it. Telling people they can recover is not necessarily helpful. Recover from what? For example if I met someone and I were to say to him while conversing, “You know I think you can recover
from your mental illness,” he would not be likely to respond, “Thanks for your faith in me” People have problems but that does not mean they have “mental illnesses.” Szasz called them “problems in living”
Spkliewer says his job is to help people recover. That’s nonsense. Back in 1988 I lost the last job I had for helping people to recover. I had finished post-doc training with Jay Haley,Salvador Minuuchin etc. I had a job in a clinic in NJ for one year. The year before I had read Peter Breggin and decided the drugs were poison. Many of my clients made extraordinary recoveries—and they got off psychiatric drugs. The director told me he was firing me because I had enraged the psychiatrist.
I know that back in 1990 virtually every professional I met believed that “schizophrenia” was a chronic incurable mental illness. The same was true of “bipolar disorder”, although they were rare in those days. I do not believe that professionals have improved.
There would be a simple way to ascertain this—ask mental health workers. Then you would see the survey is valid, the respondents were not paranoid. One could not pose the question directly because the shrinks would want to appear encouraging. No you have to get to the deep structure of psychiatric ideology. Ask 390 professionals, “ Do you think schizophrenics or bipolars can recover and wean themselves off anti-psychotics.” I’m sure there would be less than 1% of psychiatrists and less than 5% of other mental health workers who would answer in the affirmative. No, they will say, “They’ll always need to take medication. Their illness is like diabetes” Some might add, “Oh sure they can recover but they need to take their mediction.” If persons need to take “anti-psychotics” that means they still have psychosis, and they have ipso facto not recovered.
Your job Spkliewer is to create and maintain clients for the drug companies. Back in 1978 the APA made a deal with the drug companies. The drug companies will provide them with revenue and in return the psychiatric system will not only provide them with clients but they will legitimize the manufacture and marketing of toxic psychiatric drugs. This marriage required some changes—look at the extraordinary increase in the % of US population on drugs. In the earlier days those patients who were not suffering from “psychosis” were not put on drugs for life.Now everyone is Also once the deal was made with the drug companies all problem were defined as biological in nature.. The goal of the military industrial complex is not to protect national security, not to preserve peace. Its goal is to create wars and conflicts because that is how the system creates profits.
To assert Spkliewer that your job is to help patients recover is naïve.Its admirable that you want to do that, but how much freedom do you have? How many clients did you encourage last months to wean themselves off psychiatric drugs? The goal of the psychiatric pharmaceutical complex is not to help patients get well. It is to create and market diseases
In order to create permanent clients for the psychiatric pharmaceutical complex. My alternative to that
is spelled out in my recent book, or more briefly in my article on this website. See Szasz and Beyond; The Future of the Mad Pride Movement.
Thanks,
Seth
Seth Farber, Ph.D.
http://www.sethHfarber.com
Report comment
“ Do you think schizophrenics or bipolars can recover and wean themselves off anti-psychotics.”
This question you pose is very important. I can confirm that when I ask it of professionals, I most often get the answer you describe, which has lead me, and the folks I work with to do more. After asking this question of so-called professionals, so-called consumers, teachers/educators, members of the general public, other social serving organizations and the faith community we then need to follow up with more accurate information. We know this is going to take some time in our small community but we feel like it has to be done. So many people are laboring under a false/untrue conceptualization of problems of living/emotional-behavioral distress. Thanks for your thoughts Seth.
D
Report comment
And on top of what everyone has posted here you can mention all of the other studies besides this one that clearly show that people recover quite well from this so-called “illness” which is only a construct of biopsychiatry and the drug companies. Look at the two studies done by the World Health Organization, and Dr. Harrow’s twenty year study, and of Courtney Harding’s studies. It’s all out there but you never once hear the so-called mental health professionals talking about any of these studies. When I mention them to the staff and so-called professionals that I work with they have absolutely no idea what I’m talking about, which I find of great interest since these studies are old information now and have been around for a while. Why are they not better informed? They don’t want to be “informed” in any way, shape, or form because it goes against everything that they stand for and what they do to people under their power. A very few do become informed, like most of the psychiatrists who post on MIA. But they seem to be far and few between. None of the psychiatrists where I work have any idea who Courtney Harding is, have never heard that the World Health Organization did not one but two studies because they thought their stats were faulty on the first study because they showed some glaring contrasts to the present so-called “mental health system” prevalent in the developed countries of the world. THEY CHOOSE NOT TO BE INFORMED! To be informed would cause a problem for their egos and their lifestyles and they’re not willing to hazard those things at all. I say bah humbug to them.
Report comment
Very brilliantly written. The real problem is that the term recovery has been highjacked by the system. It has come to mean being medication complaint and understanding hte limitations caused by your fictional brain disease. Ask ANY professional about lowering dosages of medication – not going off, just lowering the dose and the immediate response is: “you do want to recover don’t you, you won’t be able to do that if you do not stay on this medication for life. You need to understand that you have a life long biological chemical imbalance in the brain and will need to take medication for life, just like someone with diabetes takes insulin”. Recovery to them means being allowed to live supervised outside of a hosptial. It means having some control over the food you eat. It means being allowed to work in sheltered workshops, etc. Problem is 99% of the consumer movement does not argue against it. When I say that is not recover, I am told that recover needs to be possible and while I might be able to live without medication, 99.9% of people will never be able to do so and we need to allow those people to believe that they can have some level of recover as well. And they would believe what they are saying to me, they are hand picked to work in the system, because they support the status quo, all the while shoving in the word recover in every sentence they speak and all over all the materials they produce.
Report comment
You’ve got that right. Even a lot of peer workers take up the mantra of “you need to take your meds to get well!” They do this to curry favor with the psychiatrists on the units since the psychiatrists are the gods and godesses who call all the shots. I’ve called people aside and taken them to task in private about this but it hasn’t stopped them. Too many peer workers have jumped on the “recovery bandwagon” and that’s why I’ve quit talking about recovery and talk about healing and well-being.
Report comment
The Moloch that is the mental health system constitutes a manufactory of the very problems it professes to be in the business of ameliorating or curing.
For example, they claim that their patients have problems with their brains, assertions that rest entirely on the ipse dixits of psychiatrists, no independent verification being needed, because psychiatrists have undergone an education at the university of Mount Olympus that imparts to the recipient of this education special insight. The very “treatment” leads to the problems it is meant to be curing. I could furnish you with many more examples but for the sake of brevity, I’ll leave the rest to the imagination of the reader.
I am not surprised Spkliewer hasn’t responded. Out of the materials of ignorance and dogma, those who believe in and profit from psychiatric ideology have constructed an impregnable fortress, impenetrable to the facts, within which “facts” are generated in support of the ideology; where beliefs are continually reinforced within the community of believers; where sacred mantras (such as “the drugs are safe and effective”) are chanted in perpetuity; and against this backdrop more and more sacrifices are made.
People in Spkliewer’s inenviable situation just tell themselves that they are there to help their victims to gain their conscience as an ally and to escape the guilt feelings inextricably intertwined with an honest appraisal and articulation of what psychiatrists and their subordinates do. Language can mystify, but it does not have alchemical powers; it cannot transmute the base materials of coercion, fraud and violence into therapeutic gold.
Stephen Gilbert is right. The mental-health workers in this cancerous system don’t know about the damage they are doing because they do not want to know. Their careers must come first, which depend for their existence on the espousal of the official doctrine. Some people say they are victims of a misinformation campaign. I say that in an age of unprecedented access to information, ignorance is a choice. In our age, ignorance subsists upon the will and desire of those who profit from it. In claiming that they are victims, they are merely trying to exonerate themselves of responsibility for their beliefs.
Report comment
Thanks for this post; it makes important points. It skirts close to being an ad hominem attack, though; The general point is valid one, and can be made without disparaging an individual. I would think some of the personal references could put the person mentioned on the defensive. I hope we can focus on the ideas here, and not the individuals who put themselves forth, at some risk, in the interest of building a productive discussion.
Report comment
Books on philosophy are often too abstract for me to read without a guided tour from which I can at least draft up a flow chart. I usually look around and ask what and where are the tools for change. There’s more to it than that, but I don’t usually post a lot online. I once got into trouble with the system for saying “If I believed that [I and others were no more than their DSM dx and prognosis], I would be in trouble.” That about sums up what I have to say today and have felt and believed for a long time.
Report comment
Whatever anyone wants to call it at any given time, anything can heal, change, shift, grow, evolve, etc. For anyone to suggest hopelessness about anything is to create limitations that are illusory, although they can become real through chronic programming. When we call our own plight or the plight of others hopeless, we are doing a grave injustice to humanity. Each individual needs to know their own path in order not to be vulnerable to anyone else’s opinion or “assessment.” We own our hearts, minds and spirits.
What allowed me to heal from the issues and beliefs that were keeping me feeling limited and impaired was *precisely* getting away from the mental health field (not just the system, but any part of the field which has absorbed the divisive DSM paradigm). I got these same messages of ‘poor chance of recovery,” as written on my hospital discharge papers a decade ago. I’m totally fine now—healthy, clear, grounded, detoxified from all those meds years ago, moving along with the flow of the world, creating, living, loving, even good with the family. Not a trace of how I used to feel or experience life with such incredible fear and anxiety.
What I now feel is a passionate desire to see this whole mental health mess shift into light the sake of our collective well being. There’s a great big world full of answers to questions, solutions to problems, and enlightened perspectives outside of the mental health industry.
Mostly, I was grateful to find the space to create my own path of healing and growth, having specifically with who I am as a spirit. For me, it happened to be doing theater, spiritual work, and then becoming a teacher and filmmaker, but there are infinite paths from which to choose, based on each individuals calling and desires. What I learned in graduate school about ‘personality types’ and ‘psychopathology’ served only for me to see how we create toxic social hierarchies. From my experience, that’s where the trouble started–the education of counseling psychology is sorely misguided. At least, this is what I encountered in the classroom, and then, in abudance, by experience.
Report comment
Pardon, in last paragraph, meant to write, “having specifically TO DO with who I am as spirit.”
Report comment
Sophie,
Thanks for doing the research to locate the source of messages of hopelessness. A hopeless person is a powerless person. I think personal power is an essential tool in recovery. We need more hope, more power and more recovery.
I agree that it is essential to get the word out about hope. We have to get it out to treatment providers and family members as well as people both inside and outside the current treatment systems.
All the best.
Alice Keys MD
Report comment
This is a fascinating and important discussion, and I have enjoyed following it. As a clinical psychologist and cognitive-behavioral therapist who specializes in working with clients experiencing anxiety problems, I have spent my entire career operating from a recovery model. I empathize with spkliewer’s frustration that the article portrays mental health professionals in a negative light. I don’t believe in the disease model and explicitly refute it to my clients. I emphasize the likelihood that their problems can be fully and permanently overcome with the right combination of skills and experiences. I don’t recommend the use of psychotropic drugs unless clients have full informed consent and choose to take them. Many of my psychologist friends and colleagues share my beliefs and practices in this regard.
That said, it is undeniable that we are the exception to the rule within a mental health system that overwhelmingly emphasizes hopelessness, defectiveness, and aversive treatments with questionable benefits. It is also undeniable that even those of us who operate from a recovery model have not done enough to change the mental health system, and sometimes we even reinforce (at times unintentionally) the chronic disease model through our language and actions.
Mental health professionals need to listen carefully and understand the experiences of those who have been harmed by the mental health system. Anatomy of an Epidemic should be required reading for all mental health professionals. All of my students read it. MindFreedom’s survey results are eye-opening and highlight rampant, serious problems in the mental health system.
The flip side is that are many conscientious, capable mental health professionals who provide safe and effective therapies to their clients from a recovery model. We look beyond labels to understand our clients and their circumstances, and we provide therapies that are demonstrably and specifically effective (like cognitive-behavioral therapies for anxiety problems). I’ve noticed a tendency on this site, at times, for all mental health professionals to be lumped in together as harmful charlatans. I clearly understand why awareness of the serious problems in the mental health system (especially if it is the result of personal experience) might lead one to paint all who work within the system with the same brush. But the reality is that there are large and meaningful differences between mental health professionals, and even among the mental health professions on important issues relevant to this discussion. The great bloggers on this site demonstrate as much every day.
Report comment
Hi Brett,
Thank goodness there are professionals out there like you! It is certainly refreshing to hear about your approach — particularly your avoidance of the disease model and your insistence on full informed consent for psychotropic medications.
Have you considered being listed in the MindFreedom directory of alternatives? (http://www.mindfreedom.org/directory) It’s made up entirely of professionals like yourself who agree with MindFreedom principles and try to offer an alternative to the dominant, biopsychiatric paradigm. There are folks like you out there; if only there were more!
Report comment
Some of us have been more abused by CBT than by medications. You seem to think that CBT is a perfectly harmless treatment, and you clearly show very little awareness of your own theraputic limitations by stating what you do. Anyone that is so obsessed with one thing, ie CBT to believe that it can cure everything and that nothing else is needed is no better than anyone else. In my world CBT would be outlawed long before medication. Open your eyes to the dangers and limitations of your own pet therapy and then you might truly be able to help people.
Report comment
I disagree. I don’t think that we lump all mental health professionals together as harmful charlatans. I have great respect for most of the “professionals” who post here and would allow any one of them to walk with me during times of personal distress. We don’t paint all of you with the same brush. But I will say again as I’ve said many times here before, we have no reason to trust you just because you have a title and claim that you care about people. All of us have heard that many times before. You have to prove yourself here, not by talking the talk, but by walking the walk. Words are cheap and mean little; it’s actions and attitudes that I look to in forming my decision as to whether you would be one of those very few professionals that I’d allow to walk with me in my times of distress and anguish. I can only speak for myself. Yes, I’m prickly when it comes to professionals. But I am willing to listen, and over time will make my decision about your sincerity. Come and spend some time with us; I have the feeling that you’re one of the “keepers” but you have to give us a chance to see that.
Report comment
This is a response to Brett Deacon’s response to Belinda’s response. I don’t know how it got where it’s at but of course it’s midnight so go figure. I got mixed up! It’s what happens when you get old!
Report comment
I guess it’s in the right place after all! Never mind!
Report comment
I don’t lump all mental health professionals together as harmful charlatans, I lump all institutional psychiatrists together as harmful charlatans!
Report comment
Belinda: the content and tone of your post is a perfect example of the problem I described in my post and is not conducive to a productive dialogue. If you are able to engage me in a discussion free from vitriol and unfounded personal attacks, I would be interested in understanding why you believe CBT is dangerous and should be “outlawed long before medication.”
Report comment
From the (temporary moderator):
I don’t see Belinda’s comment as an example of vitriol or personal attack, at least not to the degree that we would see it as a violation of our posting policy. I do think she mischaracterizes your reference to CBT as “obsessed,” when it seems more like a passing reference to something that you have seen as effective.
I think one of the problems is the imprecision of what is referenced when people refer to “CBT.” I think it’s referenced as if it’s an homogenous, unified practice. While there may be such a thing as a manualized, operationalized, and codified “CBT” practice, I think that in reality it is the catch-all term for what is in fact an eclectic assortment of therapies.
I see this imprecision play out in many ways, principally in the form of people saying about a person they have concern about “if only he would do CBT,” as if they know what that actually is or might be. I think that in the real world of practice today, that is rarely something anyone is in a position to say about what any one practitioner might be doing. It really means; “if only he would do something, preferably what I think he should do.” I can understand peoples’ frustration at mistaking the hoped-for end product for the means.
So while Belinda is certain to be justified in her complaints of what she has experienced, I’m confident Brett has had experiences with which to justify believing that something that was being called CBT has been helpful for people in his experience.
The helpful conversation would be about what CBT is thought to be, or has been experienced as, by all involved. Getting into a back-and-forth about whether it is good or not (or whether the individuals involved in the discussion are therefore good people or at least justified in their belief) seems less helpful.
I hope this conversation can continue in an exploration of the ideas and the ideals involved, rather than about any assumptions about anyone’s personal characteristics or inclinations.
We are dealing with difficult, subtle, highly charged subjects that have great and significant import for all involved, and in fact for everyone everywhere. Let’s try to carry that as a privilege and a responsibility, and be aware of the tenderness of the sensibilities of all involved in it.
Report comment
Being accused of advocating 4 positions I did not take and do not support, and having my motives and competence questioned, sure feels like a personal attack. I have thick skin and am not arguing that Belinda’s comments violate this site’s posting policy. Rather, I suggest that this kind of dialogue is more likely to stifle than facilitate an important exchange of ideas.
I have no doubt Belinda has valid reasons for disliking CBT based on personal experience. It would be illuminating to have a discussion about them. I have encountered numerous clients that have had negative reactions to CBT provided by former therapists. I am genuinely interested in understanding the ways in which CBT can be counter-therapeutic. As both a therapist and trainer of student therapists, greater awareness of these issues would be valuable.
As Kermit mentioned, CBT is an umbrella term that describes many kinds of therapies. Some of these are better than others, and some are provided by therapists with more competence than others. The differences between variations of CBT can be huge, at least as large as average differences between CBT and other types of therapy. I recently discussed this issue in a journal article describing a study we conducted with Wyoming therapists:
“Our findings suggest that most community practitioners claim to provide “CBT” but do so in a manner that differs substantially from versions of CBT recognized as evidence-based among clinical scientists. As such, the term “CBT” may be sufficiently ambiguous as to render it largely devoid of meaning. Rather than asking potential therapists whether or not they use CBT, informed treatment-seeking mental health consumers might be encouraged to ask, “What kind of CBT do you provide?”
http://www.uw-anxietylab.com/uploads/7/6/0/4/7604142/wyoming_therapist_survey.pdf
Report comment
Well, technically, CBT isn’t an umbrella term. It denotes (as you say) a specific body of theory and research. But in popular parlance it connotes any form of talk therapy, and may have little or nothing to do with the theory or research denoted (as you also say).
Where it gets interesting is that the theory and/or research denoted may also have little or nothing to do with what has been experienced as successful in real-world situations, “success” being a term that can go through many shades and permutations in its travels from clinical and research contexts to the real world. But it’s referenced as if it means a specific thing, because that seems to lend validity to whatever argument is being made; the specifics of the theory and more importantly the people involved get lost.
I agree, of course, that an interesting conversation is available and essential, and that assumptions, insinuations or extrapolations about motives, etc., make that impossible.
I am sorry for the degree to which that has happened, happens, or will happen to anyone on this website. It has, does, and will happen again; we deal with essential and eternal dilemmas. We can only hope to find our way back from fixed views, our own and others’, and find our way forward to an ongoing, evolving, living, and fecund conversation.
Report comment
I have also read that the therapist’s relationship with the client may have as much or more to do with success than the particular modality of therapy used. As I recall, it appeared that creating a safe space for sharing experiences in a non-judgmental and empowering way was the core of what made any therapy more effective. If the clients felt safe and respected, they tended to get better, whatever you called the therapy.
Bottom line, I agree with Milton Erickson’s sentiment that good therapy has to be re-invented for every client. I think we do what helps the client move forward toward the kind of life they are seeking, whatever that is. I don’t think there will ever be a “modality” that can account for all the wonderful variations and nuances in human behavior and experience.
And I agree, we should not attack anyone who is genuinely trying to help, even if our own experiences differ. I’m not in a position to say if Belinda is or is not attacking you (I haven’t read her posts, to be honest), but I value anyone who is really trying to make a difference and believe there are many paths to that particular goal.
—- Steve
Report comment
Hi Steve. Great comments! Your “bottom line” is very well-stated. Regarding the therapeutic relationship, no doubt it is a critical part of the benefits underlying most any therapy. Where therapeutic schools seem to differ is the extent to which the relationship is considered not only necessary but sufficient for an optimal outcome. I think the evidence is clear that for certain psychological problems, a strong therapeutic relationship relationship is not enough and problem-specific therapies are more effective than relationship-oriented therapies. This seems to be the case for anxiety problems like OCD that are most effectively treated with exposure-based cognitive-behavioral therapy. That said, your points are important. For my part, I feel a bit uncomfortable dealing in generalities about what therapy approaches work, and why, when the answer differs depending on the problem being addressed.
Report comment
This is a response to Stephen’s response about 8 posts up. I figured it might be more easily accessible here…
****************
Hi Stephen. I appreciate your insightful comments and value this exchange with you! It is difficult to have discussions of this nature in this impersonal electronic context because minor disagreements can so easily become needlessly magnified. Quickly: from my perspective, I have noticed a tendency for *some commentators, at times* to paint all people involved in the mental health system with the same brush, but this is the exception rather than the rule to the typically welcoming, challenging, and stimulating nature of this awesome community. Also, I can easily understand how those that have been harmed by the system would initially regard any of its members with skepticism – I’m sure I would. I’m delighted to be here, benefitting from the perspective of professionals, family members, advocates, survivors, and everyone else. We have much to learn from each other.
Regarding walking the walk, I note that I have published a few journal articles critiquing the biomedical/disease model (see here: http://www.uw-anxietylab.com/uploads/7/6/0/4/7604142/brain_disease_tbt_article.pdf, and here: http://www.uw-anxietylab.com/uploads/7/6/0/4/7604142/chemical_imbalance_study.pdf). I have a lengthy and vigorous critique of the biomedical model coming out before long in the most high-impact journal in my field of clinical psychology. I’ve had a longstanding professional interest in in the areas of focus of Mad in America that began in college when I spent a summer working in an addiction treatment center where every patient was labeled as having a lifelong, progressive brain disease over which they had no control. Didn’t buy it then, don’t buy it now, and my presence here, professional work in this area, and this dialogue with you stems from a passionate sense of injustice that I can hopefully play some productive role in correcting.
Many thanks for this collegial exchange and I look forward to learning from you and this site in the future.
Best,
Brett
Report comment