We are immersed these days in the erroneous idea that only randomized placebo-controlled studies (RCTs) constitute scientific data. We will discuss the origins of the over-reliance on RCTs in a future column. For now, we shall simply assume that many of our readers understand that a well-documented case study can provide information relevant to many.
And so, we would like to tell you about a Calgary-based child who we refer to as ‘Andrew’ (not his real name). Andrew is the middle child of three boys in an intact family, with two parents with professional careers. His two brothers seemed to have a normal developmental course, but Andrew did not. He displayed various learning and developmental problems from an early age, and because it was so atypical in his family, he was evaluated in the local genetics clinic (which found no evidence of any known syndrome). By age 8, after a diagnosis of pervasive developmental disorder was ruled out, he was diagnosed with an anxiety disorder. When he was 10, his anxiety symptoms became quite significant, associated with insomnia, difficulties with activities of daily living, inattention, distractibility, and self-injurious behaviour. He subsequently developed auditory and visual hallucinations, with voices telling him to harm himself. These hallucinations were followed by delusions in which he believed someone was poisoning his food, and that he had committed both murder and adultery. He engaged in obsessive prayer out of guilt for his acts.
Andrew became so ill that he was admitted to a tertiary inpatient pediatric hospital (Alberta Children’s Hospital) where he was evaluated for everything from neurological problems (CT, MRI) to PANDAS (Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal infections). Everything was ruled out, but he continued to be the sickest case of childhood psychosis ever seen on this inpatient unit even after many trials of psychiatric medication alone and in combination, including quetiapine, risperidone, fluoxetine, fluvoxamine and clonazepam. Andrew was discharged after six months on a regimen of risperidone and fluvoxamine. He returned home, and his care was transferred to the outpatient Mood and Anxiety Disorders Clinic.
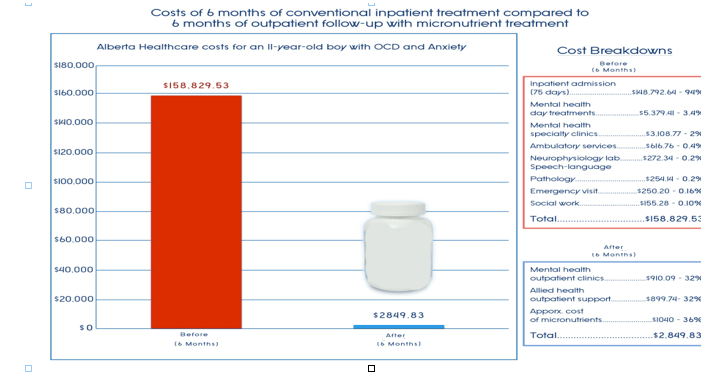
Two important notes: 1) At the time of his hospital admission, his Children’s Global Assessment Scale score was 35 out of 100 (indicating very low function); at discharge his CGAS score was still exactly 35. 2) A health economist extracted provincial health care costs of much of his 6 months of hospital care, which conservatively was $158,829.53.
What happened next was remarkable. His parents approached his outpatient psychiatrist Dr. Megan Rodway and asked for her opinion about trying Andrew on a broad spectrum nutrient formula which at that time was called EMPowerplus (EMP), since he had not responded to any medications. Dr. Rodway reports that her response was “It is snake oil, but I don’t have anything better to offer.” And so beginning in September 2008, Andrew transitioned onto EMP while gradually reducing his two medications to zero. Here is the parent report data on his symptoms of anxiety (if you are interested in seeing the graphs of OCD and psychosis, as well as Andrew’s self-report of auditory and visual hallucinations, the reference is provided below):
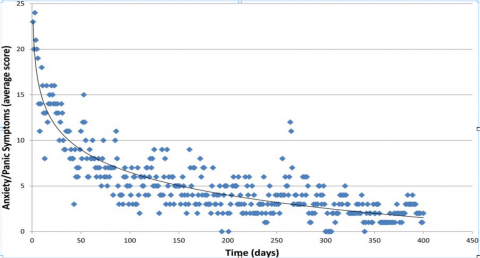
The long-term result was impressive: all symptoms of psychosis and OCD had remitted in a few months. By the next summer, Andrew was able to attend sleep-away camp.
Here are some important questions to ask:
- Has he remained well? The Calgary people have kept in touch with the family for over 4 years now, and Andrew has remained well. At one point after about 3 years, Andrew became tired of taking the capsules and began to fight them. His parents let him cut back, and then were terribly frightened when some of his symptoms returned. They quickly put him back on the full dose (12-15 capsules/day for him), and insisted that no further reversals be tried. There are no data from this reversal; only parent report.
- What is in the formula? It is a broad spectrum formula consisting of mostly vitamins and minerals. In keeping with one of our previous blogs on ‘magic bullets,’ we would like to mention that it seems highly unlikely that a single nutrient could have resulted in Andrew’s recovery.
- Are vitamins and minerals safe? He had repeated blood tests for about two years, and all results were normal. These results are consistent with others that we have published on the safety of this complex formula (see Simpson et al. reference below).
- Could Andrew’s improvement be attributed to a placebo/expectancy effect? Psychosis is a challenge to treat and complete remission is difficult to achieve. Without a placebo-controlled trial, one can never be sure, but there are several factors which argue against this interpretation: a) there is 4 ½ years of follow-up information indicating sustained improvement (unlikely for an expectancy effect), b) the parent report of an informal reversal suggests on-off control of symptoms with the nutrient formula, c) Andrew was given the best state of the art care with the inpatient admission and medications, and still there was no observed benefit, indicating that it is unlikely that expectancy effects could remove psychosis.
- What about the cost? The health economist compared the first 6 months of inpatient care to the next 6 months of outpatient care. As mentioned above, inpatient costs exceeded$158,000. Outpatient costs to the health care system were <$2,000. The roughly $1000 that the nutrients cost could not be recovered from health care; the family must pay for them.
- What is Andrew like now? Andrew is a boy with a tendency toward anxiety, who has some significant learning disabilities requiring special education. He continues to take a therapeutic dose of the micronutrient formula, sometimes with a broad spectrum amino acid formula (whey protein).
- What is the significance of this case? There does not appear to be anything unique about Andrew, which suggests to us that broad spectrum nutrient treatment should be considered for virtually all first-episode psychoses. In fact, this case illustrates what might be called a new world view: for some people, nutrients can be the primary treatment, and medication might be a supplement. (It is for this reason that we tend to avoid the word ‘supplement’ when referring to nutrient treatments.)
This is our 6th post on nutrition and mental health, and we are attempting to write about many aspects of the broad emerging field of Nutritional Psychiatry. Some of this field includes data on successful nutrient treatments (like Andrew), but other aspects include correlational data from epidemiological surveys, understanding mechanisms by which nutrients affect brain function, diet and fetal development, elimination diets, improved resistance to environmental toxicants and stress with nutrition, etc! Future posts will continue to talk about some of these more ‘academic’ topics, with occasional treatment stories like Andrew interspersed to keep us reminded about the enormous potential of this field.
To read more
- Rodway M, Vance A, Watters A, Lee H, Bos E, Kaplan BJ (2012 Nov 9), Efficacy and cost of micronutrient treatment of childhood psychosis. BMJ Case Reports. doi: 10.1136/bcr-2012-007213
- Simpson, JSA, Crawford, SG, Goldstein, ET, Field, C, Burgess, E, Kaplan, BJ (18 April 2011). Systematic review of safety and tolerability of a complex micronutrient formula used in mental health. BMC Psychiatry, 11:62. doi: 10.1186/1471-244X-11-62.












I find that interesting that they refer to him as developmentally behind. Coeliacs is something anyone can contract, and it is known for delayed intellectual development, because it creates a mind body disconnect, and inability to contact gut instincts essentially, relying on different types of intelligences, but plenty of people with degenerative disease are in intellectual professions, or president with severe spine difficulties. Food hasn’t cured my “psychosis”, though it will cure immunity, and allergy care greatly helps, if prison is sensory deprivation? I find it was more something depressives envy, as my intellectual potential greatly increased from the experience, and what lsd, was suppose to promise instead of many suicides. I like esoteric stuff from the 19th century, so I would be curious to know, if he could be qualified as a medium.
Report comment
It’s my understanding that at least in some cases psychosis reflects brain inflammation. JR Hibbeln has shown that omega-3s can reduce inflammation and ameliorate many mental health symptoms. Charles Serhan has examined how omega-3s are acted on by COX2 enzymes. They are converted to resolvins which down-regulate inflammation. All makes sense. I wonder why the psychiatrists can’t find these references.
Report comment
Maybe because Encephalitis is usually caused by viral or bacterial infection
Report comment
Hi Joanne,
In one of his Youtube videos, Robert Whitaker described psychosis as having flu-like characteristics of coming and going on its own.
This makes sense when you consider psychosis caused by encephalopathy can be caused by a virus/bacteria/toxin or a combination of such and stressful/emotional situations can weaken our immune system.
I suffered psychotic and manic symptoms from toxic causes but symptoms also exacerbated from an abscessed tooth that I delayed treatment for and after a bout of ocular shingles.
Below is a link to a narrative I wrote that was published in the Journal of Participatory Medicine explaining my experiences.
Bob is correct that psychosis can have flu-like characteristics but it is important to test for and treat the underlying cause. Although the symptoms are alike, the treatments may vary considerably.
http://www.jopm.org/perspective/narratives/2011/03/28/psychosis-possibly-linked-to-an-occupational-disease-an-e-patient%E2%80%99s-participatory-approach-to-consideration-of-etiologic-factors/
Report comment
I’m not entirely convinced, don’t rule it out, but the only way to demonstrate this would be with EEG, CT, MRI, full blood count etc, as nutritional deficiency does not explain mental distress for everyone.
Report comment
for everyone? probably for a minority of cases if that. By the way, over on his blog Behaviorism and Mental Health, Dr. Phil Hickey mentions this blog post but contrasts it with a story “of a man “with schizophrenia” who also transitioned from “anti-psychotic medication” to the same nutrient formula as Andrew used. (It’s marketed as EMPowerplus). This young man, Jordan Ramsey, shortly afterwards killed his father and gravely injured his mother.” He concludes: “Vitamins and micronutrients in proper quantities probably won’t do much harm. But they can be over-hyped. Dr. Grohol states that “…after more than a decade on the market, the manufacturers of this product haven’t done a single placebo-controlled trial.”
In my view, a double-blind randomized controlled trial is overdue for a product for which such strong claims are being made.” http://www.behaviorismandmentalhealth.com/2013/06/11/nutrition-and-psychosis/
Report comment
I haven’t very thoroughly examined it, but I find many of these inflammation theories interesting. There’s one study which found out that aspirin can reduce the effectiveness of SSRI and SSRIs can influence the cytokines through some mechanism. It also makes sense that the brain or behavior is modified by inflammation, for example in the sense that it’s good for a human or animal and the tribe if a sick person rests in relative seclusion until the inflammation goes away. Etc.
Report comment
I’m interested by the finding that psychological stress causes inflammation.
“Researchers from Ohio University found that levels of a protein that rise in response to inflammation, called C-reactive proteins, increase when a person is asked to think about a negative and stressful event.” – http://www.huffingtonpost.com/2013/03/17/stress-inflammation-dwelling-ruminating_n_2876394.html
“A research team led by Carnegie Mellon University’s Sheldon Cohen has found that chronic psychological stress is associated with the body losing its ability to regulate the inflammatory response.” – http://www.sciencedaily.com/releases/2012/04/120402162546.htm
Report comment
omega-3s are a great idea, and may help something, somehow, somewhere, but the whole inflammation-as-a-driver requires a lot more clarification. omega-3s in large doses can suppress natural killer cells so approach with caution.
Report comment
Re: Inflammation
There is a theory among some holistic doctors (ie, Mark Hyman, M.D, functional medicine practitioner) that brain inflammation is behind a great deal of “mental illness.”
My thought is that he and others may be on to something. When you consider the lack of nutrients, exposure to chemicals and toxins in our food, etc, it begins to make sense.
Omega-3s can help. So can other nutrients, used in combination, as discussed by the blog authors in a a previous post.
Best,
Duane Sherry, M.S.
discoverandrecover.wordpress.com/nutrition
Report comment
I don’t doubt that decent nutrition and supplements help, but I question brain inflammation [unless we do the physical tests on everyone presenting with ‘psychosis’]
Report comment
IMO, we would find numerous reasons for “psychosis” if we did physical tests – from sleep deprivation, to adverse reactions to prescription and illegal drugs, to a *bunch* of underlying physical conditions, from A-Z. –
http://psychoticdisorders.wordpress.com/
IMO, trauma is *not* always the cause of “psychosis.” It may be the *primary* cause, but it is not the *only* cause.
Duane
Report comment
While I agree, various research has found that psychological distress causes increases in inflammation, so before everyone jumps on the inflammation-as-purely-physical-cause bandwagon…:
“Researchers from Ohio University found that levels of a protein that rise in response to inflammation, called C-reactive proteins, increase when a person is asked to think about a negative and stressful event.” – http://www.huffingtonpost.com/2013/03/17/stress-inflammation-dwelling-ruminating_n_2876394.html
“A research team led by Carnegie Mellon University’s Sheldon Cohen has found that chronic psychological stress is associated with the body losing its ability to regulate the inflammatory response.” – http://www.sciencedaily.com/releases/2012/04/120402162546.htm
So in these cases the inflammation and the distress can both be seen as results of the same thing rather than one causing the other. Right?
Report comment
Seems to be right. A two way street. I have an autoimmune disease, have had another so I’m skeptical to any purely somatic explanation for anything. People don’t like murky issues with a lot of loose ends, but that’s where things are now. They just found this, which makes me wonder just what they think that they’ve been looking st.
http://neurosciencenews.com/lymphatic-system-brain-neurobiology-2080/
Report comment
precisely Duane..
I’ve said elsewhere trauma must not be seen as The Only Cause of ‘psychosis’!! [got shot down for it..]
Report comment
does anyone really believe that trauma is the only cause of psychosis? That’s just stupid, because it is eminently disprovable with any fairly strict definition of trauma (it is documented that many people undergo psychotic process who have not had what would traditionally be called trauma, e.g., assault or specific, discreet instances of abuse or terror), and fairly meaningless with any fairly expanded one (life itself and innumerable aspects of it could be seen as traumatic, like living under capitalism for example, which encompasses every moment of life and therefore doesn’t involve *discrete* instances of abuse or terror)…
The fact that anyone who stays awake long enough will become psychotic demonstrates that this is a normal part of ALL human beings; whether a person undergoes psychosis in their lifetime or not, all humans are capable of it, whether they have been “traumatized” (in the traditional sense) or not. This says to me that looking for *a* cause or even multi-factor causation of psychosis is missing the point– psychosis can be caused by literally anything that for a particular person who, in the absence of support within consensus reality, finds it necessary to forge a creative solution. We need to stop trying to “prevent” psychosis by stamping it out, like we would smallpox or cancer, and accept that what we need to do is support human beings at all levels– socially, economically/materially, spiritually, artistically, physically and with regard to sleep and nutrition, too, of course. The trauma discourse I find extremely limiting in this connection.
Report comment
Yes meremortal, I keep speaking of this enforced positivity because I’m seeing this within psych services through their perverted versions of ‘recovery’ but also within NGO’s and some survivors/groups within their versions too. It’s as though it’s become shameful to say anything less than ‘I am recovering’, or ‘I am recovered’, or ‘I’m a recovered XYZ’.
Most of the ‘user involvement’ work within services, and conferences/workshops only want ‘recovery stories’, it’s like we’re just not allowed to speak of ongoing or enduring difficulties, or it’s framed as our sordid personal failure. It’s become a culture of denial as you say, and that’s rippling out. It’s even wider than that Barbara’s ‘Smile or Die’ is such a great little film.
I also do not believe that trauma is the only cause of ‘psychosis’ and I question what we mean by trauma because for a while it did appear to me as though it meant childhood sexual abuse and little else because that was the main example cited. The term has been broadened now, I believe partly in response to those of us saying this doesn’t mean one thing.
Living under capitalism and sleep deprivation are good examples. Completely support your analysis on the trauma discourse.
Report comment
meremortal, why the need to limit ‘trauma’ to such a strict, narrow definition though (as has been done traditionally)? You may find the discourse limiting because you are working with a very limited concept of the term. What human beings (and other animals) have the capacity to tolerate also depends a great deal on their resources and circumstances. So what may not be too big of a deal for one may be overwhelming for another who is low on coping resources. Hence why you can’t limit the definition of trauma to just a few discrete events as has been done “traditionally,” as you say. Joanna mentions that the term has been broadened now but if you have a problem with that, you could substitute “psychological/mental/emotional distress” and would be referring to approximately the same thing.
Which is not to say that trauma/psychological distress is the one and only ’cause,’ don’t know that and am not saying it, but I do believe it’s a gigantic and maybe the primary one which is nevertheless greatly neglected/overlooked/misunderstood in the mainstream. Most mainstream efforts and dollars are put towards researching the brain in an attempt to find the causes of distress while adverse life conditions and events are routinely ignored or simply not understood. This may be why some of us harp so much on it – because it doesn’t get nearly the attention it deserves, on the contrary, it’s brushed under the rug, hidden, or simply not seen much of the time.
Report comment
I do agree with a lot of your comment though, about supporting human beings at all levels, etc. I just find that trauma (broadly defined) and dysfunctional families, relationships, social conditions and other ‘environmental’ problems get so little attention for how important they really are, and are often not well understood. There is so much money and science and technology being thrown at problems which are often simple matters of the heart and taking the time to listen, care, and connect, that some of us feel the need to harp on this point because it’s obviously not getting through.
Report comment
Everyone would have a better diet with enough money to eat, here people are being cruelly sanctioned and left with no income for months, some people are facing the prospect of starvation, I can’t even believe I’m typing this but it’s true [if anyone doesn’t believe me I can offer enough links I’m just tired right this moment.
Brain inflammation is very interesting but I think we need to concentrate on basic income/housing first, let’s get that right! Then we can look at brain scans and formulas.
Report comment
Yeah, lets actually ensure peoples basic needs are met, both physical and otherwise, before we go picking through their brains looking for the sources of their troubles, novel idea.
Report comment
In response to “Can Psychosis be Treated With Nutrition?”
That would depend on what is causing the psychosis.
If the psychotic state is being caused by something like an Ovarian Teratoma, then the answer is no.
The woman featured in the story below spent two months suffering from psychosis and labeled with schizophrenia, the second woman in the story spent two years suffering psychotic symptoms and labeled schizophrenic before two Teratomas were discovered. Her psychotic symptoms abated one day after the tumors were removed.
There are many underlying causes of psychosis and mania. There is no one-size-fits-all treatment. Nutrition is the answer for some, but not all.
Functional Medicine, Integrative Psychiatry and Orthomolecular Psychiatry certainly are the best options if a patient is interesting in detecting and treating the underlying cause, as well as hopefully preventing future episodes.
http://psychoticdisorders.wordpress.com/2013/05/29/ovarian-teratoma-causing-psychosis-monster-inside-me/
Report comment
Thank you, Maria.
You have a great deal to add in these areas!
Duane
Report comment
Duane,
Honestly, it’s to the point where I can not help but believe that the psychotic symptoms some individuals suffer from are nothing more than job opportunities for a multitude of professionals, including authors.
When it comes to symptoms of psychosis,
we don’t need to reinvent the wheel,
we don’t need any more research that involves just talking to “schizophrenic people”,
https://www.madinamerica.com/2012/10/new-research-project-funded-by-the-foundation-for-excellence-in-mental-health-care-is-in-process/
we don’t need any more books,
we don’t need any more lectures,
there are enough case studies and research out there already,
we do need caring medical and mental health professionals who want to help others and will follow best practice standards of assessment,
psychosis shouldn’t be a such a mystery when there is such a long list of underlying causes,
http://psychoticdisorders.wordpress.com/bmj-best-practice-assessment-of-psychosis/
we do need funding to help people suffering from the symptoms get the testing and treatment they need for the underlying condition (which as Bob has already stated, in many cases is probably substance abuse)
we do need creative individuals like the founders of the Delancey Street Foundation to help those in recovery obtain job skills
http://www.delanceystreetfoundation.org/
we can no longer blame the pharmaceutical companies for hindering the paradigm shift,
at this point, those who claim to be mental health advocates, need to evaluate how they are impacting the health, safety and welfare of others if they are not supporting best practice standards.
Report comment
Maria,
Thanks for your contributions in getting the word out.
Duane
Report comment
Thanks Duane.
My new contributions involve filing complaints and gathering evidence/legal reasoning for lawsuits.
Report comment
Maria,
Sounds like an exciting and worthwhile venture.
Duane
Report comment
EMpower Plus cannot be as effective or cost-effective as an orthomolecular program based on tissue mineral analysis with retesting and program adjustments every 90 days. Is EMpower Plus more effective and cost-effective than psychiatric drugs or ECT? Definitely!
A wealth of information and experience here.
http://www.arltma.com
Report comment
Subvet,
Thank you for the link, and all the comments you’ve left on MIA on the subject of orthomolecular medicine.
Glad you’re here!
My best,
Duane
Report comment
Duane,
I am only here because in 1982 I learned about orthomolecular therapy and a reliable source at reasonable cost, Analytical Research Labs. At that time, ARL was doing tissue mineral analysis for security clearances at the national labs like Sandia, Lawrence Livermore, Oak Ridge, etc. ARL could put out a very accurate personality profile which the labs found valuable in their hiring and security clearance evaluations.
Later I learned that Veterans Affairs was also a client. The VA was looking for evidence of self-medication (substance abuse)in veterans seeking hospitalization for psychiatric problems.
Neither of these two applications came near to employing the full capabilities of ARL to identify underlying chemical imbalances and toxicity and design personalized diet and supplement programs to restore health.
Had I not been involved in the nuke weapons industry, I never would have learned about ARL.
Report comment
Well, appreciate your spreading the word to others. It’s sure good to have you here!
Duane
Report comment
I found this study very interesting. I do not take EMpower Plus but take a range of supplements that includes a majority of the ingredients listed for this product. When I was taking the dreaded SSRI I developed many symptoms of auto immune disease–including large patches of red and inflamed skin on my back and legs, extreme fatigue and aching in my joints. I was also tested positive for thyroid disease. I have always been a very physically healthy and active person and had never exhibited any of these symptoms prior to taking the drug.
I had my blood analyzed and it was shown to have very high markers for inflammation. I did my own research and found a number of studies indicating that Zoloft significantly reduces the absorption of various types of Vitamin D–which can cause skin disease, joint and bone problems (osteopenia) and fatigue. I slowly started weaning myself off of the “medication” and started a supplementation program designed to combat inflammation. Every three months I repeated my blood work. The lower I went on the Zoloft the lower the markers for inflammation. Now off of the medication, I no longer test positive for inflammation and have no physical symptoms of autoimmune disease which I am convinced was caused by the medication.
If mental distress is caused by or exacerbated by inflammation then prescribing SSRIs seems to be the absolutely worst treatment protocol to offer based upon my experience. How can a drug effectively restore mental equilibrium if the very mechanisms by which it “works” creates a state in the body that contributes to mental distress? For me, that answer was/is it can’t.
Report comment
How would it be if the range of nutrients came from whole, healthy foods — maybe in addition to the supplement? When trauma is generally defined as “a situation that causes great distress and disruption,” it can also refer to any condition that disrupts the healthy, harmonious flow of ones biorhythms — like heart rhythms, brainwaves, or oscillations from the biological functioning of any organ(s). Or any situations that disrupts the harmony of one’s lifestyle or practices. It can be shown that symptoms result from disruption to healthy functioning.
Report comment
symptoms of real disease, I mean
Report comment
I think of how the brain and intestines are interrelated, as there’s an extensive nervous system in the gut. Two Awardees at a Peace Conference, including a Chief of Infectious Diseases from Kaiser, were interviewed by public radio. I’m quoting from minutes 10-18 of the African Peace Conference show: “There is almost zero programming about your health on television, in terms of the food that you eat… most of it is laden with chemicals that you can’t digest… The body sees it as toxic, so it wraps these chemicals in fat. And moves it away from your organs to your extremities… you cannot pursue life, liberty or the pursuit of happiness, if you don’t have health… with the fast food and processed food industry… we are largely dependent on the crops of wheat and corn… both have a protein… [that] needs to be soaked for 12 to 18 hours before the human body can digest it. But because we’re processing the food so fast, we don’t have time to do it. So we grind it to dust … that flour is indigestible in the human system. And it actually attacks the intestinal walls after you eat it, which is why we’re having this huge increase in something that’s called leaky gut syndrome, where the gut actually becomes permeable, and undigested food goes into the bloodstream. And the body reacts to that as a toxin. So you have this incredible increase in food allergies… much of what allows us to export this food, around the world and around the country is that it has chemicals in it that are not food. And those chemicals attack our bodies…”
http://www.capradio.org/news/insight/2013/04/25/insight-042513
Michael Pollan talked about feeding healthy microbes in the gut with a range of nutritious plants:
“There’s a great many other species occupying us, sharing our bodies, and we need them, and we need to look out for them. And one of the hallmarks of the Western diet, as you alluded to in your intro, is that it’s been designed to very effectively feed us, the 10 percent, with these – you know, we process food to make it much more readily absorbable, you know, lots of refined sugars, lots of refined carbohydrates, lots of easily absorbed fats, but very little is left for the large intestine, where the real action is going on, where you have this interior fermentation, if you will, that we’re not feeding very well. And because those guys like different food than you do in some ways. They really like fiber, for example. They love plants. They love a variety of fiber, too. That’s a real mistake of I think what we’re doing now. We’re kind of supplementing everything with fiber, but we’re only putting in one or two different kinds of fiber. And every different microbe probably likes to chomp on a different kind.”
http://www.npr.org/2013/05/03/180824408/michael-pollan-you-are-what-you-cook
Report comment
Great points, Irene.
Thank you!
Duane
Report comment
The heart too, has its own nervous system, and from a nervous system perspective, which includes the brain, heart, lungs and stomach, one could speculate that psychosis is a response to an internal threat?
Unresolved trauma certainly fits this concept of an internalized sense of threat, which the nervous system tries to contain, by degrees of respiratory, muscular and vascular constriction. Could we not speculate about internalized threats, like viral infections and tumors, invoking unconscious reactions which cannot be verbalized?
Allan N Schore, has long called for a multidisciplinary approach to mental health, disciplines like an emerging;
“Science of the Heart”
“How do stress and different emotional states affect the autonomic nervous system, the hormonal and immune systems, the heart and brain? Over the years we have experimented with different psychological and physiological measures, but it was consistently heart rate variability, or heart rhythms, that stood out as the most dynamic and reflective of inner emotional states and stress. It became clear that negative emotions lead to increased disorder in the heart’s rhythms and in the autonomic nervous system, thereby adversely affecting the rest of the body.
In contrast, positive emotions create increased harmony and coherence in heart rhythms and improve balance in the nervous system. The health implications are easy to understand: Disharmony in the nervous system leads to inefficiency and increased stress on the heart and other organs while harmonious rhythms are more efficient and less stressful to the body’s systems.
More intriguing are the dramatic positive changes that occur when techniques are applied that increase coherence in rhythmic patterns of heart rate variability. These include shifts in perception and the ability to reduce stress and deal more effectively with difficult situations. We observed that the heart was acting as though it had a mind of its own and was profoundly
influencing the way we perceive and respond to the world. In essence, it appeared that the heart was affecting intelligence and awareness.
The answers to many of our original questions now provide a scientific basis to explain how and why the heart affects mental clarity, creativity, emotional balance and personal effectiveness. Our research and that of others indicate that the heart is far more than a simple pump. The heart is, in fact, a highly complex, self-organized information processing center with its own functional “brain” that communicates with and influences the cranial brain via the nervous system, hormonal system and other pathways. These influences profoundly affect brain function and most of the body’s major organs, and ultimately determine the quality of life.” (McCraty, Atkinson, Tomasino, 2001).
In understanding my own experience of “mania” for example, I’ve learned to sense the rather magical “affect” of spontaneous breathing and its affect on my heart, with its innate reflect responses. The sudden release of my life-long constriction defense, against an internalized sense of threat, in 1980, triggered my ascent into mania. Of course, back then, I was completely ignorant of my “internal” functioning, believing my thoughts to be the major avenue of self-awareness.
As for “treating” myself with good nutrition, I do, yet have come to sense within, the unconscious functioning of my vagus nerve, and its sometimes primitive affect on my metabolism and moods. From previously taken for granted views of treatment, from a rather “external” perspective, the things I should do to myself? I’ve come to know myself within, with an increasing ability to self-regulate.
Best wishes to all,
David Bates.
Report comment
David,
I find it interesting that we have neurons throughout our bodies – particularly, in our brains, hearts and intestines.
Because when it comes to making decisions, we often think things through logically with our brain, double-check with our heart, and go with our gut.
The heart and gut can over-ride the brain sometimes.
It sounds ‘New Age’ I suppose, unless we consider how we all started as a single cell, which duplicated to form what we call our brain, intestine and heart.
Separate organs, with specific functions.
But also connected.
Duane
Report comment
And, I particularly liked what you had to say about coming to “know yourself from within” and learning to “self-regulate.”
I believe these are the things that can help any of us learn to live happier, more meaningful lives. Thank you for the words of wisdom, David.
You always have good things to say and share!
My best,
Duane
Report comment
Hi Duane, there does seem to be a new paradigm of psychotherapy emerging, which involves a shift from notions of conscious self-control, towards an awareness of the “unconscious” aspects of self-regulation.
An unconscious self-regulation which most people take for granted, like the way we learn to walk, a skill which quickly becomes an unconscious expectation of coherent movement.
Through the emerging new discipline of psychophysiology we seem to be discovering a more holistic and coherent sense of self, involving both the “voluntary” and “involuntary” nature of being human.
I do believe we can rise to the challenge of answering a mutual friend’s clarion call, “if mental illness is not what psychiatry says it is, then what is it?”
There is plenty of emerging science which supports the person centered view we all encourage. A science perspective that psychiatrists are desperately in need of, to dissolve the illusion of a brain disease, perspective.
Sadly most psychiatrists are only aware of what they are taught, and remain stuck in a “pathology” perspective, which seems to reflect a consensus fear of altered states of mind.
Best wishes,
David.
Report comment
There are many links I could post but here’s one:
http://www.thefedonline.org.uk/disability-in-the-news/disabled-people-are-being-forced-to-scavenge-for-food-from-supermarket-skips
A good diet is just not achievable for everyone because they can’t afford it [nor the supplements], they can’t get to a market to search for fresh fruit/veg, they don’t have a garden to grow any in a high rise block. Over 2 million people in and out of work have been subject to welfare ‘sanctions’ [for which there are denied targets]. Sanctions, delays in commencement, and the low paid are having use Food Banks which only offer tinned processed foods, nothing fresh. The cheapest foods are often the worst with 3 for 2 deals, and for depressed people with less cooking ability the McDonalds £1 menu is where it’s at.
Report comment
Some food banks are now turning away those who have been sanctioned and those deemed to have “chaotic lifestyles”
There is currently one person on hunger strike because of issues such as these.Whilst optimum nutrition with preventative/healing qualities are a nice discussion for many people who cannot consistently afford good food it’s just not relevant, they’ll take any food to stave off hunger. The fact that this happens in a relatively rich western economy is shocking to me.
Report comment
Here’s the problem I have right from the beginning with this. The title, the question is skewed right from the beginning and is not the one people should be asking.
The correct question is “Can poor nutrition cause/be a factor in psychosis/acute emotional distress ?”
Report comment
Can psychosis be treated with nutrition? Reverse the question.
Can malnutrition cause mental, emotional and behavioral signs and symptoms?
Fasting effectively activates the Spirit (aka “psyche”).
Report comment
How can we find out more to try this with our child?
Report comment