A. The Chronicity Problem Becomes Apparent (1960s-1979s)
It seems paradoxical that drugs that ameliorate acute psychotic symptoms over the short term will increase the likelihood that a person diagnosed with schizophrenia will become chronically ill. But that disturbing fact showed up in the very first outcome studies, and has continued to show up in outcome studies ever since.
1. NIMH’s first follow-up study
a) One Year After Discharge. Schooler, N. American Journal of Psychiatry, 123 (1967):986-995.
This NIMH study looked at one-year outcomes for 299 patients who had been treated either with neuroleptics or placebo upon their admission to a hospital. This was the first long-term study conducted by the NIMH, and the researchers found that patients who received placebo “were less likely to be rehospitalized than those who received any of the three active phenothiazines.” However, in spite of this finding, which the researchers wrote “was so unexpected,” the NIMH investigators stated that they “were unprepared to recommend placebo as treatment of choice.” (See page 991).
2. NIMH’s first two relapse studies
a) Relapse in Chronic Schizophrenics following Abrupt Withdrawal of Tranquilizing Medication. Prien, R. British Journal of Psychiatry, 115 (1968), 679-86.
The critical finding of this NIMH study was that relapse rates rose in direct relation to dosage–the higher the dosage that patients were on before the drugs were withdrawn, the greater the relapse rates. At the start of the study, 18 patients were on placebo, and only one got worse over the next six months (6%). Sixty-five patients were on 300 mg. of chlorpromazine at the start of the study, and 54% of these patients worsened after the drug was withdrawn. One hundred thirteen patients were on more than 300 mg. of chlorpromazine at the start of the study, and 66% of these patients got worse after drug withdrawal. (See table 3, page 684.)
b) Discontinuation of Chemotherapy for Chronic Schizophrenics. Prien, R. Hospital and Community Psychiatry, 22 (1971), 20-23.
In this NIMH study, the earlier finding that relapse rates rose in correlation with neuroleptic dosage was confirmed. Only 2 of 30 patients who were on placebo at the start of the study relapsed during the next 24 weeks (7%). Twenty-three percent of the 99 patients who were on under 300 mg. of chlorpromazine at the start of the study relapsed following drug withdrawal. Fifty-two percent of the 91 patients who were on 300 to 500 mg. of chlorpromazine at the start of the study relapsed following drug withdrawal, and sixty-five percent of the 81 patients who were on more than 500 mg. of chlorpromazine at the start of the study relapsed following drug withdrawal. The researchers concluded: “Relapse was found to be significantly related to the dose of the tranquilizing medication the patient was receiving before he was put on placebo–the higher the dose, the greater the probability of relapse.” (See page 22, 23.)
3. A study comparing five-year outcomes in the pre-Thorazine era and the post-Thorazine era.
a) Comparison of Two Five-Year Follow-up Studies.Bockoven, J. American Journal of Psychiatry, 132 (1975), 796-801.
In this study, Boston psychiatrists Sanbourne Bockoven and Harry Solomon compared relapse rates in the pre-drug era to those in the drug era, and found that patients in the pre-drug era had done better. Forty-five percent of the patients treated at Boston Psychopathic Hospital in 1947 had not relapsed in the five years following discharge, and 76% were successfully living in the community at the end of that follow-up period. In contrast, only 31% of patients treated in 1967 with drugs at a Boston community health center remained relapse-free for the next five years, and as a group they were much more “socially dependent”–on welfare, etc.–than those in the 1947 cohort.
Other researchers who reviewed relapse rates for New York psychiatric hospitals in the 1940s and early 1950s reported similar findings: roughly 50% of discharged schizophrenia patients had remained continuously well through lengthy follow-up periods, which was markedly superior to outcomes with neuroleptics. See Nathaniel Lehrman, “A state hospital population five years after admission: a yardstick for evaluative comparison of follow-up studies,” Psychiatric Quarterly, 34 (1960), 658-681; and H.L. Rachlin, “Follow-up study of 317 patients discharged from Hillside Hospital in 1950,” J. Hillside Hospital, 5 (1956), 17-40.
4. Two NIMH studies in the 1970s investigating longer-term outcomes in non-medicated patients
a. The Treatment of Acute Schizophrenia Without Drugs. Carpenter, W. American Journal of Psychiatry, 134 (1977), 14-20.
In this 1977 NIMH study, 49 schizophrenia patients placed into an experimental hospital program that provided them with psychosocial support were randomized into drug and non-drug cohorts. Only 35% of the non-medicated patients relapsed within a year after discharge, compared to 45% of those treated with medication. The medicated patients also suffered more from depression, blunted emotions, and retarded movements.
b. Are There Schizophrenics for Whom Drugs May be Unnecessary or Contraindicated?Rappaport, M. International Pharmacopsychiatry, 13 (1978), 100-111.
In this 1978 study, Maurice Rappaport and his colleagues at the University of California, San Francisco randomized 80 young male schizophrenics admitted to Agnews State Hospital to drug and non-drug groups. Only 27% of the drug-free patients relapsed in the three years following discharge, compared to 62% of the medicated group. Most notably, only two of 24 patients (8 percent) who weren’t medicated in the hospital and continued to forgo such treatment after discharge subsequently relapsed. At the end of the study, this group of 24 drug-free patients was functioning at a dramatically higher level than drug-treated patients.
5. The Soteria Project.
During the 1970s, the head of schizophrenia studies at the NIMH, Loren Mosher, conducted an experiment that compared treatment in a homelike environment (called Soteria), where antipsychotics were minimally used, to conventional treatment in a hospital setting. At the end of two years, the Soteria patients had “lower psychopathology scores, fewer (hospital) readmissions, and better global adjustment” than those treated conventionally with drugs in a hospital setting. Only 31% of the patients treated without drugs in in the Soteria House who remained off neuroleptics after leaving the program relapsed over the next two years.
a) A Non-Neuroleptic Treatment for Schizophrenia. Mathews, S. Schizophrenia Bulletin, 5 (1979), 322-332.
b) Community Residential Treatment for Schizophrenia. Mosher, L. Hospital and Community Psychiatry, 29 (1978), 715-723
c) The Treatment of Acute Psychosis Without Neuroleptics. Mosher, L. International Journal of Social Psychiatry, 41 (1995), 157-173.
d) Treatment of Acute Psychosis Without Neuroleptics. Bola, J. The Journal of Nervous and Mental Disease, 191 (2003):219-229.
6. The cure may be worse than the disease
a) Maintenance Antipsychotic Therapy. Cole, J. American Journal of Psychiatry, 132 (1977): 32-6.
In 1977, Jonathan Cole, the former head of the NIMH Psychopharmacology Service Center, concluded that given the myriad of problems caused by antipsychotic medications, “every chronic schizophrenic outpatient maintained on an antipsychotic medication should have the benefit of an adequate trial without drugs.” He titled his article “Is the Cure Worse than the Disease?”
B. A Biological Explanation for Drug-Induced Chronicity
7. Drug-induced supersensitivity psychosis
In the late 1970s, Canadian investigators identified the biological changes caused by antipsychotics that lead to the high relapse rates. Because the drugs dampen dopamine activity, the brain tries to compensate by becoming “supersensitive” to dopamine. In particular, the drugs trigger an increase in the density of dopamine receptors. This perturbation in dopamine function, over the long term, makes the patients more biologically prone to psychosis and to worse relapses upon drug withdrawal. The researchers concluded: “Neuroleptics can produce a dopamine supersensitivity that leads to both dyskinetic and psychotic symptoms. An implication is that the tendency toward psychotic relapse in a patient who has developed such a supersensitivity is determined by more than just the normal course of the illness.”
a) Dopaminergic Supersensitivity After Neuroleptics. Muller, P. Psychopharmacology 60 (1978):1-11.
b) Neuroleptic-Induced Supersensitivity Psychosis. Chouinard, G. American Journal of Psychiatry, 135 (1978):1409-1410.
c) Neuroleptic-Induced Supersensitivity Psychosis. Chouinard, G. American Journal of Psychiatry, 137 (1980):16-20.
C. Twenty-Five Years of Confirming Evidence
Since 1980, there have been a number of long-term outcome studies that confirm the fact that antipsychotics increase the likelihood a person will become chronically ill.
8. The World Health Organization Studies.
a). The International Pilot Study of Schizophrenia.Leff, J.Psychological Medicine, 22 (1992):131-145.
The first World Health Organization study that compared schizophrenia outcomes in “developed” and “developing” countries was called The International Pilot Study of Schizophrenia. It began in 1968 and involved 1202 patients in nine countries. At both two-year and five-year follow-ups, the patients in the poor countries were doing much better. The researchers concluded that schizophrenia patients in the poor countries “had a considerably better course and outcome than (patients) in developed countries. This remained true whether clinical outcomes, social outcomes, or a combination of the two was considered.” Two-thirds of the patients in India and Nigeria were asymptomatic at the end of five years. The WHO investigators, however, were unable to identify a variable that explained this notable difference in outcomes. See pages 132, 142, 143.
b) Schizophrenia: Manifestations, Incidence and Course in Different Cultures.Jablensky, A. Psychological Medicine, supplement 20 (1992):1-95.
The second WHO study was called the Determinants of Outcome of Severe Mental Disorders. It involved 1379 patients from 10 countries, and was designed as a follow-up study to the International Pilot Study of Schizophrenia. The patients in this study were first-episode patients, and 86% had been ill fewer than 12 months. This study confirmed the findings of the first: two-year outcomes were much better for the patients in the poor countries. In broad terms, 37 percent of the patients in the poor countries (India, Nigeria and Colombia) had a single psychotic episode and then fully recovered; another 26.7% of the patients in the poor countries had two or more psychotic episodes but still were in “complete remission” at the end of the two years. In other words, 63.7% of the patients in the poor countries were doing fairly well at the end of two years. In contrast, only 36.9% of the patients in the U.S. and six other developed countries were doing fairly well at the end of two years. The researchers concluded that “being in a developed country was a strong predictor of not attaining a complete remission.”
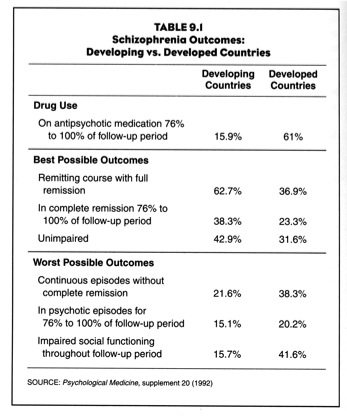
Although the WHO researchers didn’t identify a variable that would explain this difference in outcomes, they did note that in the developing countries, only 15.9% of patients were continuously maintained on neuroleptics, compared to 61% of patients in the U.S. and other developed countries.
Who Data Summarized
9. The Vermont Longitudinal study
In a long-term study of schizophrenia patients released during the late 1950s and early 1960s from the back wards of Vermont State Hospital, Courtenay Harding reported that twenty years later 25% to 50% of the patients were completely off their medications, suffered no further signs and symptoms of schizophrenia, and were functioning well. She concluded that it was a “myth” that schizophrenia patients must be on the drugs all their lives, and the reality was that “it may be a small percentage who need medication indefinitely.”
a) The Vermont Longitudinal Study of Persons With Severe Mental Illness, II. Harding, C. American Journal of Psychiatry 144 (1987):727-734.
b) Empirical Correction of Seven Myths About Schizophrenia With Implications for Treatment.Harding, C. ACTA Psychiatrica Scandinavica 90, suppl. 384 (1990):140-146.
10. A meta-analysis of the outcomes literature.
a) One Hundred Years of Schizophrenia. Hegerty, J. American Journal of Psychiatry 151 (1994):1409-1416.
In 1994, Harvard Medical School researchers reported that outcomes for schizophrenia patients in the U.S. had declined since the 1970s, to the point they were no better than they had been in 1900. Although the researchers did not blame antipsychotics for the poor outcomes, it is notable that this decline occurred during a period when American psychiatrists began telling the public that people diagnosed with schizophrenia had to stay on the drugs for life. In other words, the decline coincided with the adoption of a paradigm of care that emphasized lifelong drug therapy.
11. MRI studies
During the 1990s, researchers using MRI technology discovered that antipsychotics shrink the frontal lobes and cause an enlargement of the basal ganglia. In the “Follow-up Magnetic Resonance Imaging” study, researchers reported that the enlargement of the basal ganglia was associated with a worsening of both the positive and negative symptoms of schizophrenia. This was powerful evidence of how the drugs cause chronic illness over time.
a) Increase in Caudate Nuclei Volumes of First-Episode Schizophrenia Patients Taking Antipsychotic Drugs.Chakos, M. American Journal of Psychiatry 151 (1994):1430-1436.
b) Neuroleptics in Progressive Structural Brain Abnormalities in Psychiatric Illness. Madsen, A. The Lancet 32 (1998):784-785.
c) Subcortical Volumes in Neuroleptic Naive and Treated Patients With Schizophrenia.Gur, R. American Journal of Psychiatry 155 (1998):1711-1717.
d) A Followup Magnetic Resonance Imaging Study of Schizophrenia.Gur, R. Archives of General Psychiatry 55 (1998):145-152.
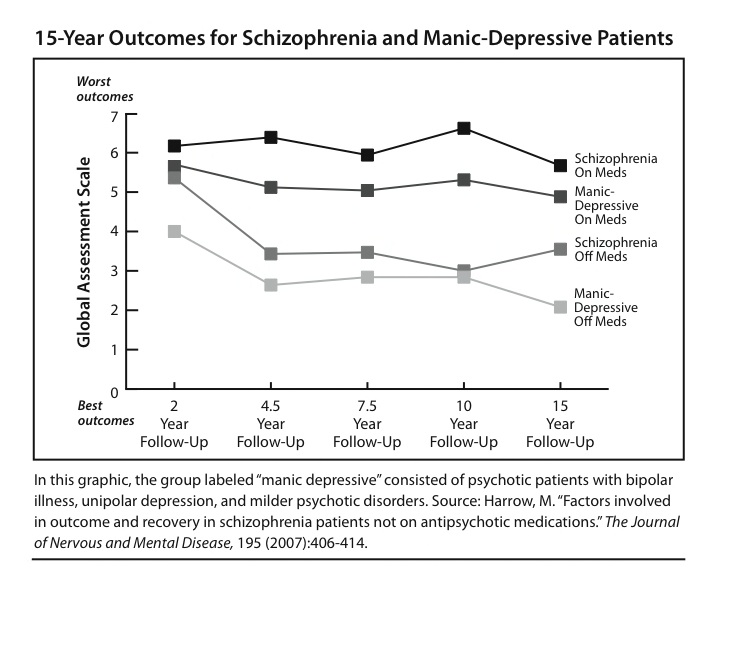
12. Martin Harrow’s 15-year outcomes study
a) Factors Involved in Outcome and Recovery in Schizophrenia Patients Not on Antipsychotic Medications. Harrow, M. Journal of Nervous and Mental Disease, 195 (2007): 407-414.
NIMH-funded researchers followed the long-term outcomes of schizophrenia patients diagnosed at two Chicago-area hospitals in the late 1980s, and they found that at the end of 15 years, 40% of the schizophrenia patients who had stopped taking antipsychotics were recovered, versus 5% of those who had stayed on the drugs. Long-term outcomes for patients with “other psychotic disorders” were also much better for those off the drugs than for those who stayed on the medications.
Mad in America Documents
The evidence for antipsychotics
Antipsychotics and chronic illness
Antipsychotics and progressive brain dysfunction
Early death associated with antipsychotic drugs
Outcomes in the era of atypical antipsychotics
Modern experimental programs producing better outcomes












[…] can find links to these studies and the other information about them, here: http://www.madinamerica.com/2011/11/antipsychotic-drugs-and-chronic-illness/ Many of the contributors to that site, which is a wonderful resource for cutting edge science and […]
Report comment