Note: This is the ninth piece or final third of the final triptych in the Lasagna trilogy of triptychs that started with Not So Bad Pharma and runs through to Marilyn’s Curse.
Marilyn died of an overdose of barbiturate sleeping pills (Tragedy). A bystander, Lou Lasagna, noted she had been denied access to a sleeping pill that was safe in overdose, the first pill of any sort that had been proven to work and be safe in an RCT before it was marketed. She was denied by doctors who put more weight on uncontrolled clinical observations than RCT data. As she died, she uttered a curse. Life went on. At first Lou noticed nothing but over the years his horror grew (Empire 1, Empire 2).
On April 10, in the midst of the Lasagna series, an article appeared in the New York Times that attracted a huge amount of interest – mostly outrage. It covered a story about research on premature infants who were being treated with Oxygen to prevent blindess. The key detail was just what had the parents been told about the study – what had they consented to?
Johanna Ryan who contributes regularly to this blog posted the following:
It looks like Informed Consent is something that needs constant defending – kind of like Free Speech. Just yesterday I read about a study testing various levels of oxygen on 1,316 premature babies. According to the New York Times, HHS officials concluded that “the study did have an effect on which infants died and which developed blindness, and that those risks were not properly communicated to the parents, depriving them of information needed to decide whether to participate.” The consent forms mentioned only one risk: possible skin abrasions from an oxygen monitoring device.
The study was centered at the University of Alabama, with participation from Yale, Stanford and Duke, among others. One hundred and thirty of 654 babies in the low-oxygen group died, while 91 of 509 babies in the high-oxygen group developed an eye disease that can lead to blindness. University officials scrambled to minimize the death rate by comparing it to that of preemies who were not in the study. However, this was not a control group at all; it consisted of infants excluded either by the researchers or by their parents, because they were extremely fragile.
The Times brought forth Dr. Arthur Caplan, the dean of American bioethics, to muse sagely that complete informed consent was overrated anyway. Most consent forms, he said, consisted of a “truth dump” listing every conceivable risk, and were aimed more at protecting the institution than the subjects. He felt most parents would rely on what the doctors told them instead of reading all that fine print. The pity of it is, he may be right – although I think I’d rather wade through the Truth Dump than trust Dr. Caplan to tell me what was an acceptable risk for my baby.
And this is research at the finest academic medical centers, on an old familiar molecule, O2, that nobody owns! Just imagine how things are going in the for-profit centers where the blockbuster drugs of tomorrow are tested. Who looks out for the (unemployed and/or uninsured) subjects there?
The rise of informed consent was influenced by the rising tide of new-drug research in the 1950’s, I’m sure … but it also owed a lot to the civil rights movement. Working at the University of Illinois’ Hospital in the early 1990’s, I found elderly black patients always called the place by its old name – “Illinois Research.” The assumed deal, not too long ago, was that if the care was free, the doctors were free as well, to experiment on you as they saw fit. If you were black, or otherwise not a first-class citizen, you didn’t count on any protection. The fight to overturn that grim state of affairs lasted well into the 1960’s, from the notorious Tuskegee study to New York’s Willowbrook Hospital and Pennsylvania’s Holmesburg Prison. And like other fights won at that time, it might not stay won, if no one’s watching. This time around, we’ll need to look out not just for the research subjects, but also for the rest of us who get the treatments vouched for by that research.
The idea of Informed Consent took shape in the 1950s centered on breast cancer and ECT legal cases. Histories of bioethics, like Rothman’ s Strangers at the Bedside suggest it really took off in 1965 when Harvard’s Henry Beecher published an article outlining a series of cases from the best institutions in the United States where patients were being exposed to experimental treatments or other forms of research without being aware of what was happening.
Lou Lasagna looked on at Beecher pushing this boat out. As with almost all these things he thought Beecher took the nub of a good idea and pushed it that bit further than was warranted. Lasagna had established the beachhead – to mix metaphors – but rather than bunker down and see what happened next, Beecher was keen to get up and at-em and storm the enemy lines.
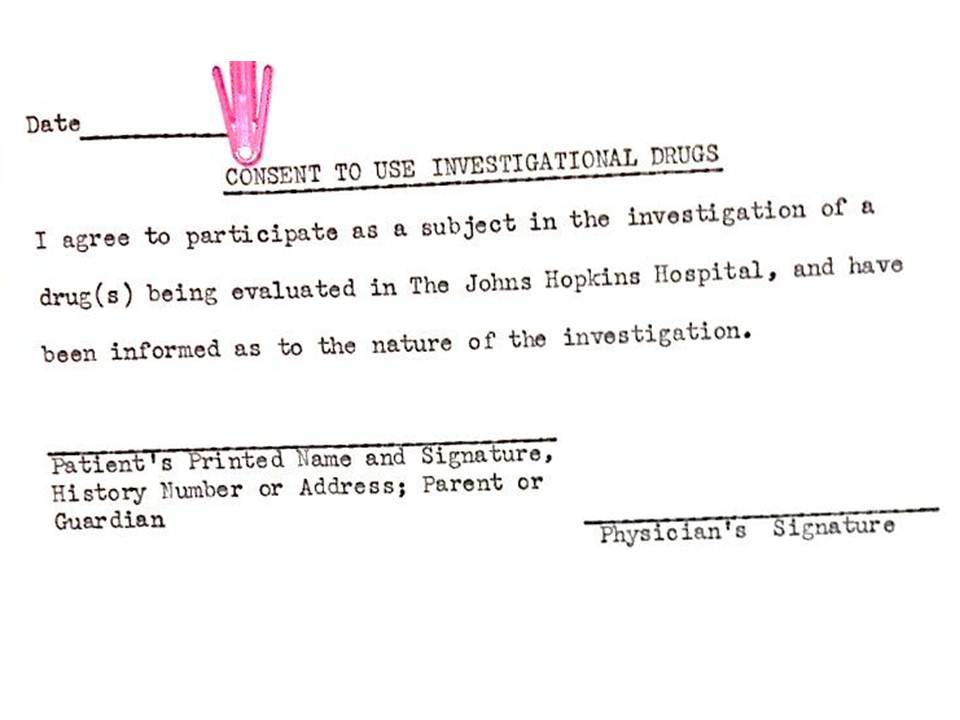
Lasagna’s beachhead had been established in 1962. He had campaigned the ensure that all patients taking an investigational new drug produced by a pharmaceutical company were aware that the drug was novel and not yet approved. He produced the first consent forms for this purpose. He put it on the agenda for Kefauver’s 1959 hearings only to see these hearings sink out of sight in a political quagmire. And then thalidomide struck.
The politicians had to be seen to do something fast. They rushed through a Bill that required companies to prove their drugs are effective and to do so using controlled trials. They maintained the prescription-only status for new drugs that Kefauver found problematic on so many fronts. They also left product patents in place – the single thing he was most keen to change.
To top it off, for good measure they made consent forms for investigational new drugs mandatory.
A good idea? Well it meant that FDA had to be involved from the very start of the very first investigation of a new drug. Partly because of that the length of time a drug spent with FDA increased from a little over a year in the 1950s to over ten years in the 1970s. Companies were handed a stick to beat FDA with.
They were also handed a blank piece of paper. Once they have had a chance to think about it, companies appear to have felt increasingly strongly that they have to do more to protect the rights of patients. The consent form evolved to include clauses telling study participants that their data would be shown to no-one other than the regulator. Translated into English this meant your data and our privacy will be hidden for ever.
Informed consent which was designed to safeguard patients has become a key vehicle safeguarding companies.












I’ve always wondered about this. Living in the States, I know that electroshock therapy requires informed consent. The problem is that one of most common reasons for its use is that the patient is in crisis and unresponsive to medication, right? How on earth can you be in crisis and unresponsive to other treatments to the point where electroshock is your best option, and yet, informed enough to give consent?
Report comment