Pictures are worth a thousand words. They can distill mountains of detail into essential understandings. So I’ve chosen pictures to distill the mountain of mental health research I’ve examined over the last eight years. Three infographics summarize research on psychiatric drugs, and one asserts why I think Integrative Mental Health is the best path available for mental health recovery.
First, antidepressants.
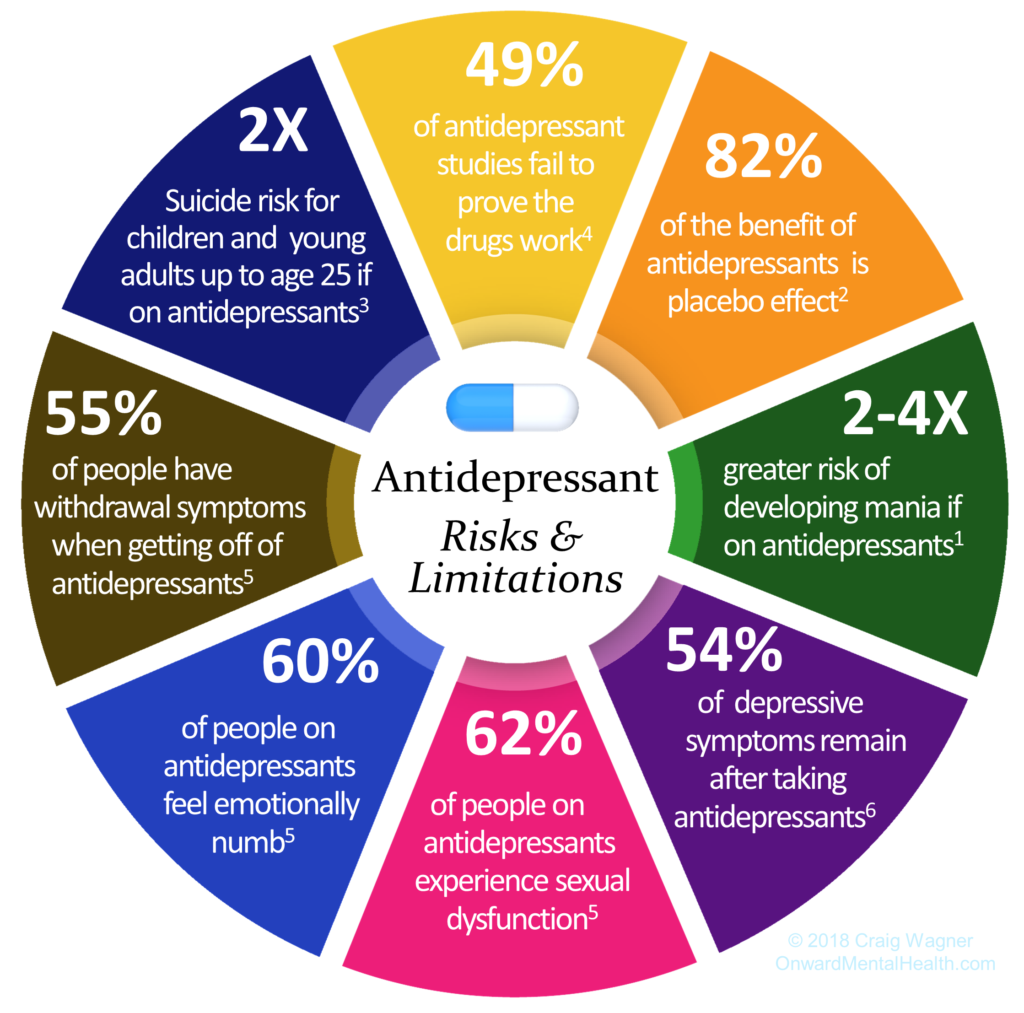
The FDA1 and meta-analyses2 tell us that the advantage of antidepressants over placebo for treating depression is razor thin; so small, in fact, that most people can’t tell the difference. To gain this small advantage people must accept antidepressants’ side effects, risks, and limitations which can be significant. Even more startling, at milder symptom levels — representing about 85% of people taking these drugs for depression — antidepressants have no advantage over placebo.3
Second, antipsychotics.
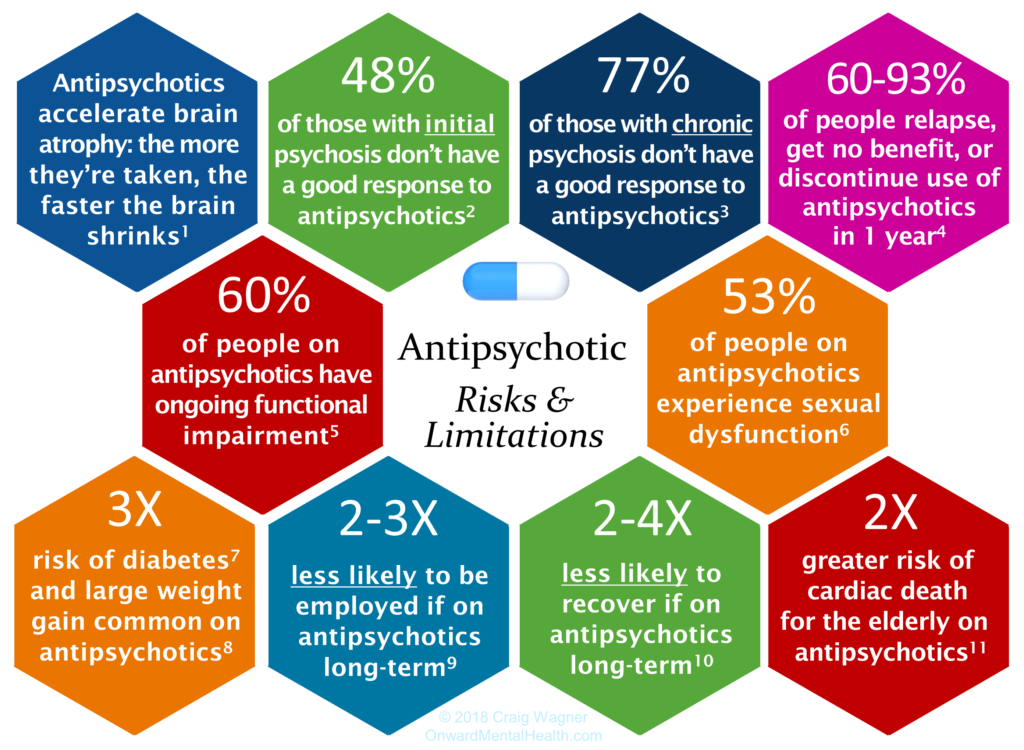
For many people, antipsychotics reduce psychosis. But less than a quarter of those with chronic psychosis see even a 50% reduction in symptoms when using them.4 And this partial symptom relief often comes with life-altering side effects. Additionally, evidence suggests that antipsychotics may do more harm than good in the long term.5
Finally, benzodiazepines.

Benzodiazepines can reduce anxiety, often quickly. But prescribing guidelines say their use should be restricted to very short durations. There is good reason: significant cognitive decline and potentially life-threatening withdrawal make them a questionable solution beyond episodic anxiety.
Psychiatric drugs, the big picture
These infographics paint a troubling reality of psychiatric drugs. It isn’t surprising that most carry the strictest FDA warning, a black box. But there is another reality: some people find meds indispensable.
This hit home with me last fall at the Massachusetts Psychiatric Rehabilitation Association summit. After I presented these infographics I received nods of recognition as people saw their own experience in the numbers. But at the break, a peer support specialist spoke with me. “I’ve been on Clozapine for years,” she said. “It’s the only thing that works for me. It’s what allows me to do my job.”
So these infographics don’t suggest a mass exodus from drugs. Rather, they suggest exercising informed caution if you choose to use them. The risk/reward profiles of these drugs are much more questionable than their ubiquitous prescribing might indicate.
The infographics contain another message: look beyond drugs to other approaches that give more avenues for recovery. Thankfully, many such options exist.
Integrative Mental Health and the web of causation
Integrative Mental Health is an emerging paradigm that provides a diverse set of evidence-based options that include, but go well beyond, medication.
Unlike conventional psychiatry which focuses on symptoms and prescribes drugs to reduce them, integrative practitioners seek to understand and treat the causes that lie beneath the symptoms. They probe for markers of biological, social, environmental, and habitual factors unique to the individual.
They see these factors interacting in a dynamic web of causation. Some people have one factor that strongly predominates. Others strain under the accumulated weight of many smaller issues. And sometimes a minor incremental stressor can be the straw that breaks the camel’s back and ushers in a crisis of mental distress.
Here is a conceptual view of the web of causation, highlighting factors shown in research to be associated with mental distress.

Integrative practitioners perform biomedical testing, psychosocial evaluation, and probe personal history to understand this web. They address suspected causative factors, selecting from a menu of 27 evidence-based non-drug options. These include diet, exercise, digestive care, calming practices, nutrient supplements, herbs, psychological therapies, and much more. Nearly all these options have very low or no side effects and can be used with drugs. This is good news since drugs can be a part of the equation as well.
In thousands of cases, these customized interventions have significantly decreased symptoms, allowing drug dosages and associated side effects to be greatly decreased. In some cases, symptoms are completely eliminated without drugs.
Although Integrative Mental Health is showing great promise, it isn’t a silver bullet. We don’t know all the factors that influence mental distress and we can’t fully address all those we know. They also can take weeks or months to show full benefit and practitioners are hard to find.
But there is good reason to be hopeful. People who live in recovery overwhelmingly report that a combination of approaches was needed,6 and the growing number of integrative practitioners can help provide them.
Changing Awareness
There is significant work ahead if we are to reap the benefits of Integrative Mental Health. It starts with communication.
We must communicate the risk/reward profile of psychiatric drugs, so people know to look beyond them. But we must also communicate that some people find drugs necessary.
We must communicate the full menu of available recovery options, so people and their practitioners can craft the best path forward. We must communicate the remarkable stories of recovery to give hope to those in distress. And we must communicate that recovery is not only possible but should be expected.
That’s a lot of communication.
To make it easier, let’s use pictures. They’re worth a thousand words.
*****
Infographic footnotes:
Antidepressants [link]
Antipsychotics [link]
Benzodiazepines [link]












What is the number one cause of “mental distress” in the world today? Although the matter is certainly not beyond dispute, I would say that the number one cause of “mental distress” in the world today is the fact of being born into the physical universe, that is, corporal existence. Many peoples’ experience of life on this planet began with a slap on the rump.
I like the graphs, and I think they must be very instructive, however I do have a little problem with how they were conceived. This is especially true with the one on what you call anti-psychotics, and I would call neuroleptics, drugs that I have heard referred to, with no small sense of irony, as psychotic drugs. The problem, as I see it, is this matter of envisioning “mental distress” as a form of “impairment” that would be corrected through the impairment of drug use. The reality is that what you really get are psychological, that is, psycho-somatic conditions supplanted by chemically induced physical injury.
“Chronic psychosis” seems to me a much more mythological creature than say “chronic drug impairment” coupled, of course, with financial “impairment”/dependency. This web of causation starts with seeing a problem where no problem necessarily exists. The web of deception is further complicated by the x = unknown factor. Here, a cause is like the winning number in the lottery, all you have to do to get “mental distressed” is to reverse the odds.
Curiously we don’t see “mental distress” as a winning position, mostly.
Report comment
Hi Frank, Thanks for your thoughts. You make an interesting point about trying to fix one form of impairment (i.e. mental distress) with another (drug use). Indeed, the impairment created by antipsychotics is well documented, especially in the long-term studies. Many of the non-drug approaches for psychosis (including CBT for psychosis, Open Dialogue, and Hearing Voices Network) don’t try to medicalize psychosis, but seek to meet the experience, understand it, and find ways to work through the issues it may present.
Report comment
Thank you for your honesty, Craig.
Report comment
It’s easy to feel discouraged, and in a lot of ways it is a natural response. A couple of things to consider. Thousands of people have recovered, and when I get down (as a care provider), I like to talk to peer support specialists. Not to get anything specific, but I find that their courage seems to rub off on me as I see that they have come back from dark places and have made the noble commitment to help others. We all need those kind of people in our life. Second, there are 5 broad stages of recovery… 1) Distress, 2) Awareness, 3) Preparation, 4) Rebuilding, and 5) Maintenance. A tipping point (and a potential stalling point), a fundamentally human challenge, comes at the beginning of stage #2. It is where we look ourselves in the eye and viscerally feel: a) I want to get better, b) I can get better (others have), c) I’m going to push ahead (and stumble along the way) until I do get better… It is finding some way to set the discouragement aside for periods. Just like anything, it is a developed skill. Mindfulness can help with that.
Report comment
I would like to support that neuropetics are the better word.
“In the 1950s, when the drugs we now call ‘antipsychotics’ first came along, psychiatrists recognised that they were toxic substances that happened to have the ability to suppress thoughts and emotions without simply putting people to sleep in the way the old sedatives did” (Joanna Moncrieff, MD 13. August 2013; Deniker P. Compr Psychiatry 1960 Apr;1:92-102.). Mainstream psychiatry was uncomfortable with the notion that its principle treatment worked by being a neurological toxin and transformed it into a sophisticated, treatment. At last the misleading expression “antipsychotics” was chosen.
Breggin clls this medication neurotoxin.
“Antipsychotics” do not cure psychisis as the word suggests but reduce symptoms for a small minority.
Report comment
I love the camel cartoon with the multiple factors weighing down!
Report comment
Thanks Mark! I wanted to use that comparison since crisis is often preceded by some stressful event in life that really seems like the “last straw”. A huge collapse can occur that is way out of proportion to the size of the incremental stressor – a lot like “breaking the camel’s back”…
Report comment
craig…good work…I don’t see the word psychological…
Report comment
I did find the word psychological…sorry
Report comment
TinyTortoise, good catch. Taking a psychological view of distress is so often overlooked – especially in situations of the many forms of anxiety. We are such tightly integrated mind-body-spirit beings that the distinction between causes and effects becomes blurry. That’s why I think it more helpful to think of a dynamic web of causation where factors can be both causes and effects. Ron Unger in his CBT-for psychosis class (https://www.udemy.com/cbt-for-psychosis/?couponCode=ISPS-US%20Regular%20price) points out that social isolation can cause psychosis to worsen – AND – Psychosis can cause us to become more socially isolated. The problem gets big when that feedback loop starts to spiral out of control…
Report comment
good work CW…
Report comment
Hi Craig,
my wife has d.i.d. I have shepherded her healing using attachment theory among other things. I get frustrated by her ignorance of how lucky we got as she never used any drugs nor got caught in the mental health system. I have struggled to show her how detrimental these drugs are while she defends all the women she knows who uses them. So I sent her your 4 charts and hope, maybe, a picture will be worth a 1000 words to her.
Sam
Report comment
Sam, I admire your foresight in looking for more holistic solutions with your wife. It is difficult to swim upstream against the fast rushing flow of psychiatric drugs, but it seems like you did it. Integrative Mental Health offers a much more sensible answer in my mind. Their approach: 1) Start with wellness fundamentals (diet, exercise, mindfulness, safe home, etc.) since we know those dramatically impact mental health, 2) Do testing/evaluation to find all the factors that are out of whack and address those found (there are a number of biomedical factors that are easy to check for but rarely are – see the Resources page at http://www.OnwardMentalHealth.com for a list of those tests), 3) Doing the first two should reduce symptoms, so if they are still not manageable, drugs can be considered for RESIDUAL symptoms. Conventional psychiatry does it in the opposite order: start with drugs (and often end with drugs). I too am a caregiver, and I hear you on the frustration angle. I have to remind myself that when I get frustrated, that is something I can and should control. Mindfulness and present-momentness is what works for me to be able to cast aside frustration. I especially like to read Eckhart Tolle when I get wound up.
Report comment
Thank you for this excellent summary.
Report comment
Glad to see a note from our brethren to the north. You have the good fortune of having many more Orthomolecular practitioners in Canada than we have in the U.S. Abram Hoffer did the great ground work that formed the basis of today’s nutrient therapy. He handed his work to Carl Pfeiffer who in turn put it in the capable hands of William Walsh. From the Michigan area, I and others have gone to Toronto for assistance. The good news is that we are seeing practitioners trained in nutrient therapy sprouting up in the U.S. The Walsh Institute (www.WalshInstitute.org) also has a directory of telemedicine providers.
Report comment
I knew Abram Hoffer – not as a patient – and I am responsible for the very last audio interview he gave – a few weeks before his death – he suggested that all psychiatrists should be sent to Mars – “we’d be better off without them’ Whenever he met a client he would ask them what they were going to do when they got well – many cried because no one had ever told them they could get well – and most got the idea they could get well and they did – a belief system and some inexpensive micronutrients. For listing of orthomolecular practitioners see http://orthomolecular.org/resources/pract.shtml and here’s Hoffer’s last interview
http://www.maieliiv.com/linkedfiles/AbramHoffer2.mp3 – hope this works
Report comment
Amnesia, Thanks so much for forwarding the clip from Hoffer. I love his question “What are you going to do when you are well?” So opposite of the “you will have this diagnosis for the rest of your life and be on drugs”. His question assumes recovery, expects recovery, and reaffirms a self-determined future. So often practitioners lose track of this human fundamental.
Report comment
Craig Wagner: Thank you. Dr. Hoffer’s daughter was a dietitian at Women’s College Hospital in Toronto. She often did rounds with doctors/psychiatrists and was horrified by their comments and their treatment of patients.
Report comment
Wow, Thank you! This is so amazingly helpful for people trying to sort out what factors might be involved.
Sadly the current system with its coercive methods make it excruciating difficult to explore all the biological and environmental factors (e.g hormonal imbalances etc.) if you are avoiding becoming tangled up in the ‘system’. Any tips on how to explore these things outside the system (e.g. places to send hair analysis or whatever).
Report comment
Sa, Absolutely. You want to find a biomedical practitioner trained in the Walsh Institute protocols, Orthomolecular protocols, or similar. Look here for a directory: https://www.walshinstitute.org/clinical-resources.html for Walsh trained docs. Note that if you don’t find someone in your area, they have telemedicine providers (you get a blood test run locally and work over phone/Skype with practitioners). For the most complete list of biomedical providers and how they differ, go to https://www.onwardmentalhealth.com/resources. Look at two documents: 1) Biomedical IMH Practitioner Finder, and 2) Biomedical Test Panels. The former helps you find a practitioner, the latter gives you a list of the biomedical tests they should be running. Second document also lists a couple of labs that can do the analysis. Every practitioner favors a little different testing protocol, so I suggest using the second document to arrive at an agreed plan with your chosen provider, perhaps testing in waves. Important: just going to a GP and saying “please run these tests” won’t work. You need someone trained in what all the results mean from a mental health perspective and what specific interventions should be given based on the lab results. At the same time you are working the biomedical angle, I would find a good psychologist/therapist to investigate the psychosocial side. Client/therapist rapport is key. Cognitive Behavioral Therapy helps virtually every diagnosis and there is a variant customized for nearly every diagnosis. Therapists can evaluate the need and recommend specific therapies. If the biomedical and psychosocial efforts don’t predominantly address the issues, you can consider drugs to address residual symptoms (but really study the above infographics first). If you do, start with low dosages, assess impact plus and minus. Not to hawk my book, but it goes through all of the evidence on what seems to work. Steep discounts of book for those in financial need.
Report comment
Thank you so much. I will do this and get your book as well. I am wondering whether or not different options are available (eg, hair anaysis or saliva or something) for someone not willing to go in for blood tests.
Report comment
For my own part I frequently experienced tardive psychosis during mini-seizures brought on by the neuroleptics I took. So I refuse to call those drugs “antipsychotics.” They also caused obsessive patterns of thought that made everyone hate me. Thank goodness these went away when I was taken off my stelazine.
Now the only thing I take is levothyroxin for my bad thyroid. And lots of supplements including a monthly iron infusion due to the number SSRIs played on my gut!
Report comment
Congrats on the great progress. Sounds like you’ve figured out key things to help (thyroid and gut)… Gut/diet issues, including gut permeability are hugely important. Here is a post I wrote recently on the gut-brain connection that you might find interesting (https://www.onwardmentalhealth.com/blog-1/the-gut-brain-connection-research-meets-clinical-care-in-integrative-mental-health). Good luck.
Report comment
Hats off to you, Mr Wagner. I respect your integrity in this matter.
Report comment
Although, you are still being alarmist.
c
Report comment
I know that this article is meant to be helpful, and that the intentions are good.
But the first problem is that there is no such thing as an “antidepressant” or and “antipsychotic.” Neurotoxic drugs might more appropriately be termed “depressants” or “psychotics,” because they induce depression and injuries that are often diagnosed as “psychosis.” I’m really tired of the phrase “more harm than good.” Can we just be honest. These neurotoxic drugs were DESIGNED with the explicit purpose to HARM in ways that people would not recognize. They only do harm, even though many who ingest them think that they “work,” as Breggin has noted in his analysis of neurotoxic “spellbinding.”
These are not “meds,” no matter how many people find them indispensable. People find alcohol, tobacco, nicotine, and street drugs indispensable, but that no more makes them medicine than calling a dog’s tail a leg.
Moreover, we need to honestly consider where the Black Box warning came from and why it is there. Do you think that Pharmaceutical companies were eager to put a Black Box warning on their neurotoxins? Of course not. How did it get there? Perhaps there are only a few people in the MIA audience who know the answer to this question.
Finally, integrative psychiatry, just like the rest of the fraudulent, enslaving enterprise, needs to be abolished. Psychiatry IS the camel, and the whole camel is in the tent, not just the nose. Actually, it’s a dragon that must be slain. Psychiatry CREATES the very problems that it purports to cure, and it EXACERBATES any other problem. It medicalizes every day life, and markets madness. It is the science of lies, and it must be abolished.
The abolition of psychiatry is the best path to recovery, and an even better path to prevention of debilitating iatrogenic harm. This is what needs to be communicated. The truth. As far as remarkable stories of recovery… that is a euphemism for survivors of psychiatry. Psychiatric survivors’ stories, as well as the stories of psychiatric martyrs, are sacred and must not be allowed to be appropriated by the very institution that took the lives of the martyrs and nearly took the lives of survivors.
The best infographic for psychiatry would be the word “psychiatry” with a prohibition sign (circle-backslash symbol). And if you really want to use pictures, I highly recommend Auntie Psychiatry’s excellent drawings in her book “Of Course I’m Anti-Psychiatry, Aren’t You?” https://www.amazon.com/Course-Anti-Psychiatry-Arent-You-Illustrated/dp/0957313721
Report comment
dragon slayer —this article is helpful because it talks and shows ways that people can be healthy…
it shows ways that work…this article is more than good intentions…
I have been helped with these ways…I want to focus on what helps me..
just talking about the terrible things that don’t work just makes me sick..
Report comment
The alarmist claims you make about benzodiazepines are not as clear cut as you present them.
This study (http://www.bmj.com/content/352/bmj.i90) published in 2016 in The BMJ
found that higher exposures to benzodiazepines over long periods contributed to a *decreased* risk of dementia.
The study as a whole found no evidence of a causal link between benzos and dementia.
Why present unknowns as established facts?
Report comment
Rasselas.Redux. Thanks for the reference. It is a large study, especially as compared to a previous meta-analysis of many small studies… The data may be more conflicted than the infographic portrays. I need to dig into this especially in comparison to the large Canadian study. Always open to new data. Let the best information prevail. Thanks for the feedback.
Report comment
Rasselas.Redux. On review, I agree that the Gray study throws in a new data point to what had been fairly consistent evidence showing a tie between benzos and cognitive decline. I’ve highlighted the mixed results and softened the wording in an updated infographic that can be found at https://www.onwardmentalhealth.com/blog-1/8-years-of-mental-health-research-distilled-to-4-infographics. I’ll retain the previous version intact in this thread to support the dialog. Thanks again for the reference.
Report comment
Yeah. Pretty silly.
Everyone knows consuming massive quantities of opium for 20 or 30 years never hurt anyone. How alarmist to think they are any more dangerous than gumdrops! 😀
Those Benzo buddies are a bunch of radical conspiracy theorists no doubt.
Report comment
“Everyone knows consuming massive quantities of opium for 20 or 30 years never hurt anyone.”
Opium doesn’t hurt people, by the by. In fact, the evidence, as scant as it generally is for taboo psychoactives, suggests that frequent opium use lengthens life, rather than reduces it.
What causes problems with opium isn’t the opium, it’s all the other shenenigans that tend to come with it, like prohibition, violent criminal supply lines, adulterants, narcissistic rock stars, violent crime, prostitution, and so on.
Opium itself is a fairly benign substance if used sensibly by sensible psychonauts.
Synthetic opioids are another matter entirely.
But I was only pointing out to Mr Wagner that the evidence linking benzodiazepines to the unestablished disease of dementia is altogether uncompelling, and at turns, contradictory. All we can say is that there is a strong correleation in some studies and a very weak correlation in other studies. And that it is alarmist to cherrypick only the studies that support a causation claim.
Mr Wagner agreed with me and altered his graphic a little bit, to tone down, as much as he felt was necessary, the alarmism.
Report comment
DragonSlayer… You touch on an interesting subject. I like MIA’s “rethinking psychiatry” mission because it leads to the follow-on step of re-doing. If we were to put the circle-backslash through today’s psychiatry creating a clean slate, what would we build on that clean slate tomorrow? Wouldn’t we include some of the non-drug options that integrative mental health promotes today (e.g. good diet, sound sleep, mindfulness, nutrient balance, helping people work through past trauma, freedom from abuse, etc.)? I think a lot of what integrative mental health people are thinking is “I’ll let others worry about what to do with conventional psychiatry, I’ll predominantly leave it alone and create a wellness oriented approach on a clean slate in my own practice”…
Report comment
Craig, I’ll pick up that metaphor right where you dropped it! (First, it’s a given that psychiatry is a pseudoscience, a drug racket, and a means of social control. It’s 21st Century Phrenology, with potent neuro-toxins. the DSM-5 is nothing more than a catalog of billing codes. All of the bogus diagnostic allegations in it were invented to serve as excuses to sell drugs, and bill insurance & the Gov’t, i.e., Medicaid & Medicare)
So given that “clean slate”, we wouldn’t build ANYTHING on it! We’d leave psychiatry, *AND* the so-called “mental health system”, right there on the scrap-heap of history, where they BELONG! Most so-called “mental illness” is largely built on dysfuctional parenting, and ACE’s, combined with a generally sick society. (That’s NOT to “blame parents”, they themselves were raised by parents who were raised by abusive, dysfunctional parents, etc., We can break the cycle at any point in time. Why NOT NOW?) The system as it exists today, exists largely to cover up physical and sexual abuse, and “blame the victims”, and to serve as a means of both social control, and employment. The so-called “mental health system” serves post-industrial fascist capitalism in a couple of ways. It puts excess workers on “disability”, which makes them more dependent on Gov’t, which thus makes a large, powerful Gov’t at least *seem* more necessary. It provides employment to those who would otherwise have supervisory, or administrative jobs in factories which either no longer exist, because they’ve been outsourced overseas, or become obsolete through automation. This dynamic also explains the complex, convoluted, wasteful billing process, which is deliberately Byzantine, and the fact that there are 2 paper-pushers doing “billing” for each hands-on medical person, i.e., Dr., or Nurse, etc. And of course, there’s the DRUG RACKET aspect of the so-called “mental health system”.
All of these factors COULD BE addressed, in the absence of psychiatry, simply by building entirely new social structures, where the Gov’t, and Insurance pay people to simply DO things TOGETHER!
Sorry, Craig, but NO!, we do NOT need to “replace” psychiatry. We need to KILL IT OUTRIGHT. DEAD.
After all, it’s *human*, it’s gonna die someday, anyway.
(And, above, that “good diet, sound sleep, mindfulness, nutrient, etc.,…is MUCH harder in the current paradigm than it needs to be. That’s why the current system gets such poor results. Duh.)
It’s NOT a “healthcare maintenance system” we have now, it’s a SICKNESS CREATION system….(Duh x2)…
(c)2018, Tom Clancy, Jr., *NON-fiction
Report comment
Good diet and sound sleep are ineffective if your SSRIs wipe out your digestive tract and your neuroleptics create insomnia.
Continue to bail with a teaspoon while I drill more holes in the boat with my Black and Decker.
Report comment
Having been through Mental Health, Inc., I am sad to say…a kinder, gentler, more humane psychiatry is still…psychiatry. There was a time when I thought Orthomolecular, maybe Orthomolecular plus psych drugs in low doses, maybe “talking treatments,” etc. might be the way (or at least…a way) forward. I was wrong.
Give Mental Health, Inc. an inch, they’ll take a mile. Not only do I agree with Szasz and other critics that psychiatry is a belief system, I think psychiatry is such a dreadful, destructive belief system that one could quite accurately call it a modern day death cult.
So…while a part of me still admires those who do intensive research on “mental illness” and Mental Health, Inc. and offer up humane ways of dealing with “psychosis,” etc…the bigger part of who I am simply wants to see more people work towards the abolition of psychiatry and everything else Mental Health, Inc. is selling us. The pills are toxic, the talk is nothing more than poisonous lies, and the entire industry is filled with prideful, mediocre, dangerous people who seem hell bent on lobotomizing the whole damn world.
Report comment
Peter Breggin from 7/8 years ago – Psychiatry and the Holocaust–The Violence Initiative – Part 1
“It all began with the systematic murder of mental patients”
https://www.youtube.com/watch?v=MQZdUmxG1Es
“Now where was American psychiatry during this…”
https://youtu.be/MQZdUmxG1Es?t=499
https://en.wikipedia.org/wiki/Robert_Foster_Kennedy#Controversial_Views
Report comment
Hi Survived, and I’m glad you did! Thanks for the comments. I think Szasz is right that every discipline has a belief system, including psychiatry. My dear friend Stephanie is a great example of belief systems at work. She was diagnosed with bipolar disorder as a young adult. She was in and out of psychiatric hospitals for many years. She tried an endless variety of therapies: psychotropics, electroconvulsive therapy, transcranial magnetic stimulation, ketamine treatments, acupuncture and herbs, meditation and yoga, and more. The game changer was when she changed her belief system and fired her psychiatry team at a leading university after four years of countless treatments that made her worse, not better. She went into a different hospital and luckily had an inpatient integrative psychiatrist. With that care, instead of daily suicidality she enjoys being alive. She ended her drug-centric belief system and was open to any alternative. Luckily she found one that worked for her. The important thing for me here is that we don’t need to wait for the old belief system to wither away – any individual in an instant can change their belief system. That’s what Stephanie did. I find that one of the best ways to encourage a dysfunctional belief system to wither away is to walk away from it and put our energies into a new one – and communicate compellingly about it. It takes a long time, but it is demise by neglect. We each must decide. If the drug-centric belief system is flawed, what is a better one? After 8 years of searching I’ve found nothing better than the non-drug approaches of integrative mental health. But, if there are better things, I’m all ears!
Report comment
what a very good blog here….let the drug thing wither away and walk away….yes yes..
and healthy eating and healthy exercise is at the top…but it is hard work..
but we have a very big problem…people want a quick fix…
Report comment
People still don’t get it. There is no need to replace psychiatry with anything. Abolish psychiatry. Get rid of it. Would anyone want to replace slavery with something else? Should we try to replace Naziism with something else? Of course not. All this talk of reform, criticize, and replace completely misses the point. Once a person understands what psychiatry is, and why it must be abolished, that person clearly understands that the only need is to abolish it, not to replace it with something else or to reform it or criticize it. If it is true (and it is), that psychiatry is causing (and has always caused) the death and misery of millions of innocent people, why on earth would a person defend it? This is one of most deceptive things about psychiatry. So many people believe that there is something good about psychiatry, that it has something to do with helping or healing, when in reality it is a pseudo-scientific system of slavery, torture and drugging. But until people see that fact clearly, there will be endless discussion about how to reform psychiatry, make it better, or replace it with “alternatives.” Szasz saw these things clearly many, many years ago. Karl Kraus saw them clearly many years before Szasz. When will the world wake up to the truth?
Report comment
When slavery officially ended the newly freed citizens did need help. Many continued living like slaves as sharecroppers. Racism got worse–not better. The KKK was started.
Northerners promised the ex-slaves “five acres and a mule” since they might get the vote and the Yankee demagogues wanted it. Sadly land and the 19th century equivalent to tractors never materialized.
Report comment
Yes. That actually further proves my point, because slavery continued under another name. This would be the equivalent of criticizing or reforming psychiatry. The abolition of slavery did not put an immediate end to slavery, and slavery continued to be practiced in other ways. This is the same thing that reform and critical psychiatrists seem to wish for. Rather than abolish psychiatric slavery, they want to continue psychiatric slavery in other forms. We do need to think carefully about the abolition of psychiatry, and what we can learn from the abolition of slavery. Of course those who are freed from the tyranny of psychiatry will need help… but that help cannot and should not come from anything that is related to psychiatry, critical, reform, or otherwise, because then it is just psychiatry, or slavery, under another name.
Report comment
Stefanie was more fortunate than many caught in psychiatry. I’m glad she got better. Just wish there were more stories like hers.
Report comment
Beeing trained as physist and ingeneer I object that my dicioplines are like “every discipline has a belief system”. If engineers base on belief are make mistakes the products (bridges, plains and so on) will collaps. Every phisicist knows that the only thing science really can do is “falsify” theories.
Psychatry is a week science and psychiatrist disregard its results. Unfortunately many of us patients beleive in what psychiatrist are telling then also the results are a desaster i. e. 8.1 to 20% recovery. Open dialogue achievs quadruple recovery rate, reduces schizophrenia per year to one tenth and disability allowance/sickness is reduced to one third: http://wkeim.bplaced.net/files/recovery-en.html
The only solution I see is that we patients make a revolution and stop to accept thatwe are made sicker.
Report comment
“But, if there are better things ,I’m all ears !”
At this point it’s not rocket science so to speak to understand that we have deprivations and impositions. Psychiatry is the Mother of all impositions .Abolish it . As well as most all of AMA “medicine” a grand imposition . Then we have the ADA heavy metal including mercury dentistry, another entrenched imposition. Then we have a eugenically adulterated and genetically modified and artificially limited food supply , another imposition and deprivation at the same time. I could go on and on. Minus the deprivations and impositions, Walla…. feeling great appears.
Report comment
Here are some better things.
1. Non-coercive counseling. Choice theory and Finnish Dialogue are good.
2. Hearing Voices support groups.
3. 12 step programs like EA.
4. Journaling, writing and other art forms.
5. Nutritional supplements–especially if emotional problems are caused by a deficiency.
6. Exercise minus Zoloft. Seriously. Zoloft makes exercise less effective at helping depression.
7. Figuring out how your life stinks and fixing it or coping more effectively.
8. Sleeping at least 7 hours a night but less than 9.
9. Figuring out how to taper off your SSRIs. These cause depression and prolong episodes. My bouts of depression used to last a week.Thanks to the miracle of SSRIs I had a single episode of low grade depression for well over 10 years.
10. Doing nothing at all. Sometimes a safe space is necessary, but it’s not supposed to be a “treatment center.” Just 3 hots and a cot, the ability to exercise, peace and quiet, and a few sympathetic ears to vent to.
With the “safe and effective treatments” psychiatry provides “schizophrenics” have a 16% recovery rate. Without any treatment the number is 70%.
Which odds do you prefer?
Report comment
For those of you who are interested in learning the truth about psychiatry, I recommend the following educational resource: https://psychiatricsurvivors.wordpress.com/2016/05/10/the-truth-about-psychiatry/
Report comment
I’m warming a little to the graphics. Anyone who reads them should begin to get the idea. Neurotoxins aren’t good for your health. I feel if we go into “mental health”, anyway we put it, we’re actually dealing with an abstraction. The point is that doctors should be warning patients about these drugs rather than prescribing them, and doing so for life. Given that there are so very many people who have been completely duped, I think they have to be a positive step in a better direction.
Antidepressants don’t relieve depression effectively, and taken long term, they may exasperate it.
“Antipsychotics”, neuroleptics, atrophy the higher functioning of the brain, and they decrease brain mass (i.e. destroy brain cells).
Benzodiazapines should never be prescribed long term. They are addictive, and they impair cognitive functioning.
It’s not an information war that people are suffering from here so much as it is a disinformation war, and as such, reliable information can become a powerful inoculate to it, and an invaluable armor against it.
Report comment
Frank. You make a good point that doesn’t get discussed: people are not getting a complete picture of the downsides of these drugs from prescribers. Most often, the dialog is, “there are a variety of side effects (insert list here), but severe ones occur seldomly, and let’s stay close to monitor your specific reaction”. These graphics can put more substance to the side-effects dialog. However, I can see where it is difficult for a prescriber to say, “Although meta-analyses show that antidepressants are only slightly better than placebo, I’m prescribing them anyway.” They don’t want to undercut their prescribed care. The issue of conformance comes into play as well, and I understand how prescribers don’t want to scare people away from what are (rightfully or wrongfully) front-line therapies. Given all that, I think it is important to make this information available in an easy-to-consume form for lay people. And you are absolutely right: at the high level, there is only one purpose to all three of the drug infographics – they are an attempt to have people understand that drugs by themselves rarely are satisfactory, and they therefore must look beyond them…
Report comment
I see psychiatric drugs as essentially harmful. They are construed as helpful, but they aren’t helpful. They are so harmful that doctors should be leery of prescribing them. These drugs are advertised as miraculous medicine for people suffering from “mental illnesses”. In a hospital, actually incarceration, setting, they complement the confinement. A lot of people have been duped into thinking these harmful substances are beneficial to health. I think they are detrimental to health, and to me, that’s exactly what these infographs show. The question is, how do you get people who have been duped into thinking something that is bad for them is good for them to take better care of themselves. I think of the infographs as a start in that direction.
Report comment
Frank, yes, its a start. And there are many voices here at MIA making many starts. Hopefully we can reach some good ends with them.
Report comment
Craig I have always felt condemned when these “magical” pills did not work. People yelled at me when I seized, gained weight, couldn’t smile. These were actually proofs of my “compliance.”
I’m off the damned drugs. No one can even tell. They seem amazed that I can smile and have lost forty pounds.
Refusing to consider myself mentally ill helps me act more responsibly.
How is considering yourself hopelessly insane supposed to help you behave yourself? It teaches that you can’t help yourself and if you keep pill popping all your problems will resolve themselves or be resolved by the Keepers of the Mad enabling you. Isn’t learned helplessness the proper term?
Report comment
Let us quantify “For many people, antipsychotics reduce psychosis.” from a patient perspectice.
Reduction of 50% or more of psychotic symptoms are achieved according to Leucht et al 2009 effect of “(overall 41 versus 24% responded under SGA drugs and placebo, respectively) or an NNT of 6” i.e. for a small minority (1 in 6 patients) at the beginning of psychosis.
What about longterm-effects?
Leucht et al 2012 deals with maintenance treatment with neuroleptics. The studies range from 7 to 12 months. The results for preventing readmission are 1 in 5 patients (NNT = 5) and the conclusions for further research are “focus on outcomes of social participation and clarify the long-term morbidity and mortality.” “Nothing is known about the effects of antipsychotic drugs compared to placebo after three years “(Leucht et al. 2012, p. 27).
There is no evidence of maintenance treatment for more than 3 years (FHI: ISBN 978-82-8121-958-8). Bjornestad, Larsen et al. 2017 admits that evidence of maintenance medication is missing: “Due to the lacking long-term evidence base (Sohler et al. 2016) …”
From a patients perspective recovery is what we patients want.
There is no evidence that antipsychotics promote “psychosocial functioning, professional functioning, and quality of life” (Buchanan et al 2010 PORT Treatment Recommendations). Recovery treatment still wins terrain and will be put into a historical context. Mike Slade et al. 2014 describes the implementation of recovery with both usage and abuse of the term. http://wkeim.bplaced.net/files/recovery-en.html
Thank you for an article giving much valuable information, but “For many people, antipsychotics reduce psychosis” is obiously wrong. Psychosis is not reduced but only one in 6 patients get reduced symptoms (not psychosis) 50%.
Report comment
Walter, excellent comments. Thank-you. Points well taken. Would like to reach out off-line and compare notes.
Report comment
Thank you beeing open minded 🙂
Report comment
Based on your comments I modified the paragraph on antipsychotics. See https://www.onwardmentalhealth.com/blog-1/8-years-of-mental-health-research-distilled-to-4-infographics. To maintain the integrity of this comments stream, I’ve left the original intact above. Thanks for your insight.
Report comment
I agree. Yet nearly all the health professionals, “loving” family members, and even some grateful consumers swear the stuff is magically effective.
I see the shuffles, flat expressions, vacant eyes, and inability to function. I have also experienced all the above and more. Are others blind or just dismissive of things they don’t like or that contradict TV?
Report comment
Important to note that “psychosis” is an experience that can be brought on by lack of sleep, ADE to street or prescription drugs, lack of B vitamin, being on a ventilator, dehydration and is a symptom of over 60 medical diseases. As such drugging it is medical malpractice. The number of people who end up with a specious “mental illness” dx because they were suffering a one time event is incalculable as is the long-term damage to their lives. Seeking the root cause of the experience is not the preview of Allopathic quackery- it has NOTHING to do with health or healing, it pathologizes people for profit. Nothing could be sicker or more twisted than that.
Report comment
Well said Judi.
Report comment
Thank you very much for these infographics.
With regards to long-term treatment with neuroleptics may I suggest to include the issue of drug withdrawal leading to rebound psychosis (due to neurolpetic-induced dopamine receptor upregulation) with a high probability.
This issue should be adressen at the beginning of neurolpetic long-term treatment so patients and their friends and families all know that it will be very difficult for them to get off these meds in case they don’t work (which is in the majority of cases).
In addition, the lack of psychiatrists willing and knowledgeable in helping patients stay safe in the neuroleptic treatment withdrawal process is another huge issue in and of itself.
Report comment
“it will be very difficult for them to get off these meds in case they don’t work (which is in the majority of cases). ”
This is so true. If Robert and the rest had experienced this they would be shocked and realise very quickly why psychiatry is utterly brutal, has to end and not be so focus on the endless studies proving nothing but what ever bias the authors have.
Report comment
Silvi, thanks for the great suggestion… I’ll take a look at the research and see if I can distill it down to a compelling nugget to add to the antipsychotic infographic. The antipsychotic pic above does not speak to withdrawal, but the antidepressant and benzo pics do, so that certainly weighs in favor of including it in some way.
Report comment
Silvi, after reading up on dopamine super-sensitivity and its effect on withdrawal I’ve added another hexagon to the antipsychotic infographics. See https://www.onwardmentalhealth.com/blog-1/8-years-of-mental-health-research-distilled-to-4-infographics. I’ve not modified the graphic above to retain the integrity of this comments section. Thanks for the insight!
Report comment
I want to make some graphs of my own.
1. A line graph. One dark, solid line for the number of mass shootings in America. Several lighter, divided lines for numbers of various psych drugs consumed.
2. A pie chart divided to show how people get diagnosed and enter the mental health system. X% who got in through “losing it” for no easily discernible cause. Y% who were severely traumatized from rape or veterans with battle fatigue. Z% who took SSRIs for depression, nerves or off label purposes and wound up with nice little Bipolar labels. And we mustn’t forget kids who start out by fidgeting in class, get put on ritallin and are accused of bipolar as young adults.
3. A bar chart depicting life expectencies of those diagnosed with schizophrenia and bipolar throughout the past hundred years. Contrasting those in the 1900’s with the 1960’s and the present when all these Safe and Effective Treatments are so readily available. Whether we want them or not.
Report comment
Good idea to use the graphics indeed.
Just noting that:
Health Canada issues a 2005 warning stating that AD’s carry the same risk of suicidal ideation in ADULTS, as they do in other populations. This fact gets missed repeatedly.
the risk of completed suicide is 12X higher for Prozac than other AD’s.
And that the most important fact of all is missing, which is that the DSM is junk science – rendering the ‘treatment” of imaginary “diseases” mass medical malpractice, insurance fraud and defamation of character to slander and accuse people of being “mental ill” with no scientific evidence supporting the claim.
Report comment
Hi Craig,
I met and briefly spoke with Robert Whitaker here in Australia a couple of weeks ago.
This is a very good article and very useful – Well done!
I have found 6 of the references. Are the rest available? It looks like there should be a total of 11.
FYI: I am the co-author of several Papers on ‘The Situational Approach…” to Suicide Prevention and Mental Health Literacy’. I emailed links to these Papers to Robert Whitaker following our chat.
http://malesuicidepreventionaustralia.com.au/wp-content/uploads/2017/06/Situational-Approach-Document_web.pdf
http://malesuicidepreventionaustralia.com.au/wp-content/uploads/2017/06/Mental_Health_Literacy_Paper_web.pdf
Thanks Craig
Anthony
Report comment
Anthony. Thanks for the kind words. It is a little confusing, but there are actually 4 sets of references: each of the first three infographics has their own references (note at the very end of the article there are separate links for each of these infographics, pointing to their associated references – these links take you back to pages on my site, http://www.OnwardMentalHealth.com) and the text of the post has its own set of references which are included at the “show 6 footnotes” links above. Also thanks for your references, I’ll look them up. Also note that I have an updated version of this post on my site at https://www.onwardmentalhealth.com/blog-1/8-years-of-mental-health-research-distilled-to-4-infographics that has benefited from the wisdom of some who posted comments above, resulting in changes to both the benzodiazepine and antipsychotic infographics.
Report comment
Thanks Craig
All good now.
Anthony
Report comment
I live in Canada. I have had the worst care. I got myself off of quetiapine with the help of a naturopath and a compounding pharmacist. After years of complaining about side effects I finally had had enough when my dentist consulted an expert and he said my tongue swelling must be a drug side effect. Funny thing. Noting happened. I got off the toxic stuff and was fine. My psychiatrist retired (she’s going blind – I do have compassion but can’t help but see the irony). She said she was not referring me to anyone else because I was FINE. I am not though. Physically. I am 100% chronically constipated and 100% dependent on colonics. That is after three years of trying every other therapy. Not so funny is the response I get from every specialist I see. They will not confirm that any of my side effects are related to the meds I took. I took clonazepam also. I have had nerve conduction done, two colonoscopies, four MRIs, etc. etc. As soon as I mention the quetiapine they shut my file and get up out of the chair and start walking to the door. I was told there is no point trying to sue because there is no way to win. I can’t enjoy my grandchildren ad I can’t afford my medical care. I am trying to heal my nervous system and this is helping me cope but I get hopeless often. The psychiatrist mentioned that I have tardive dyskinesia in a letter to my family doctor but never bothered telling me about it. I only found out because I asked for a copy of the letter. I am trying to “let go” but I am too angry. I should add that when my psychiatrist agreed that I could discontinue the drug she told me to come back when I was done. That is all the “help” she offered.
Report comment
I should add that when my psychiatrist agreed that I could discontinue the drug she told me to come back when I was done. That is all the “help” she offered.
Report comment
I was told by a lawyer I consulted that because of information in a paper titled “Up to Date” which gives doctors impunity basically I would not be able to sue. I think it is time to expose this company that produces this “Up to Date” information for what it is. If a doctor consults this company (which is U.S. based) then as long as they follow the “latest” guidelines they cannot be held accountable for any harm. We hear all the time that we are too litigious. I would like to know how much money this company makes and if any of my tax dollars (in Canada) are going to this company. There is absolutely no incentive for doctors to even try something new if they can just carry on without fear of a lawsuit. This company must have a lot of employees. I started to think that my doctor was a psychopath since she chose to keep me on drugs despite the side effects but now I believe anyone who would work according to this “Up to Date” information will never be up to date. Why bother?
Report comment