Once second-generation antipsychotic drugs came on the market (which are known as “atypicals”), there were claims by psychiatric researchers that they would lead to much better outcomes for people diagnosed with schizophrenia. Unfortunately, government-funded studies (as opposed to research funded by the pharmaceutical companies that manufacture the drugs) have shown that patients are not doing any better than patients on the old drugs like Thorazine and Haldol. Moreover, the problem of early death associated with antipsychotic drugs has accelerated since the introduction of the atypicals.
A. Efficacy Studies (Not funded by pharmaceutical companies)
1. Atypical Antipsychotics in the Treatment of Schizophrenia: Systematic overview and meta-regression analysis. British Medical Journal 321 (2000):7273.
After a systematic review of the research literature, British investigators conclude that “there is no clear evidence that atypical antipsychotics are more effective or are better tolerated than conventional antipsychotics.”
2. Effectiveness of Antipsychotic Drugs in Patients with Chronic Schizophrenia. New England Journal of Medicine 353 (2005): 1209-23.
Known as the CATIE study, researchers funded by the National Institute of Mental Health report that the new atypicals provide few, if any, benefits over the old drugs. Outcomes were poor for patients on both the new and old drugs.
3. Effectiveness and Cost of Olanzapine and Haloperidol in the Treatment of Schizophrenia. JAMA 290 (2003):2593-2702.
Researchers with the U.S. Veterans Administration report that olanzapine (Zyprexa) does not provide any benefit over haloperidol in terms of compliance, symptoms, or overall quality of life.
4. Randomized Controlled Trial of the Effect on Quality of Life of Second-vs. First-Generation Antipsychotic Drugs in Schizophrenia. Archives of General Psychiatry 63 (2006):1079-1087.
5. Cost-Effectiveness of First-v.-Second-Generation Antipsychotic Drugs. The British Journal of Psychiatry 191 (2007):14-22. (Abstract only.)
British investigators funded by the U.K. government report that, if anything, patients on the older drugs have a better quality-of-life than on the atypicals.
B. Long-term Outcomes
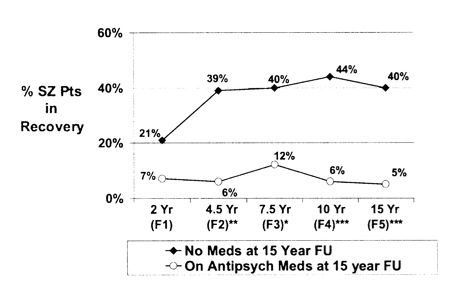
6. Factors Involved in Outcome and Recovery in Schizophrenia Patients Not on Antipsychotic Medications: A 15-Year Multifollowup-up Study. Journal of Nervous and Mental Disease, 195 (2007): 407-414.
NIMH-funded researchers followed the long-term outcomes of schizophrenia patients diagnosed at two Chicago-area hospitals in the late 1980s, and they found that at the end of 15 years, 40% of the schizophrenia who had stopped taking antipsychotics were recovered, versus 5% of those who had stayed on the drugs. Long-term outcomes for patients with other psychotic disorders were also much better for those off the drugs than for those who stayed on the medications. (This is the first look at long-term outcomes since atypicals like risperdal and olanzapine became the recommended treatment.)
C. Adverse Events, Tardive Dyskinesia, Brain Shrinkage and Early Death with Atypicals.
This is a small sampling of the many studies that detail the problems induced by atypicals. In particular, there is growing literature on how Zyprexa and the other atypicals may induce metabolic dysfunction, and those studies are not available here. The section will be updated in the future.
7. Extrapyramidal Side Effects with Risperidone and Haloperidol at Comparable D2 Receptor Levels.Psychiatry Research: Neuroimaging Section 75 (1997):91-101.
NIMH researchers report that when risperidone and haloperidol (Haldol)at are compared at equivalent therapeutic levels, risperidone induces extrapyramidal symptoms in 42 percent of the patients, compared to 29 percent of the haloperidol group.
8. Neurologic Side Effects in Neuroleptic-Naive Patients Treated with Haloperidol or Risperidone.Neurology 52 (1999):782-785.
In a study of 350 patients never before treated with neuroleptics, Physicians at McMaster University in Canada find that a low dose of risperidone caused Parkinsonism in 59 percent of the patients, compared to 52 percent of patients treated with haloperidol. The incidence of akathisia was also higher in the risperidone patients, leading the researchers to conclude that “risperidone may not be a useful alternative to typical antipsychotic drugs.
9. Adverse Effects of Risperidone on Eye Movement Activity. Neuropsychopharmacology 16 (1997):217-228.
University of Pittsburgh researchers report that risperidone, when administered to neuroleptically naive patients, caused a disruption in eye movement still present four weeks after treatment was initiated, evidence of a neurological side effect lingering for a much longer time than it did in patients treated with haloperidol.
10. Clozapine Diabetes Mellitus, Hyperlipidemia, and Cardiovasular Risks and Mortality.Journal of Clinical Psychiatry 66 (2205):1116-1121.
Patients treated with clozapine are at increased risk of dying from cardiovascular disease resulting from clozapine-induced obesity and metabolic disorders.
11. The Effect of Atypical versus Typical Antipsychotics on Tardive Dyskinesia: Eur. Arch. Psychiatry Clinical Neurosciences 257 (2007):169-172.
Twenty percent of patients on atypicals developed tardive dyskinesia in less than five years, a rate similar to that with standard neuroleptics. Severe TD may even more of a problem with the atypicals than with the standard neuroleptics.
12. The Influence of Chronic Exposure to Antipsychotic Medications on Brain Size Before and After Tissue Fixation. Neuropsychopharmacology 30 (2005):1649-1661.
After 17 to 27 months of exposure to either haloperidol or olanzapine, the brains of macaque monkeys shrink 8-11% in weight and volume.
13. Effect of Chronic Exposure to Antipsychotic Medications on Cell Number in the Parietal Cortex on Macaque Monkeys.Neuropsychopharmacology (2006):1-8.
After 17 to 27 months of exposure to either haloperidol or olanzapine, macaque monkeys show a 14% decrease in glial cells in the brain.
14. Prospective Analysis of Premature Mortality in Schizophrenia in Relation to Health Service Engagement: Psychiatry Research 117 (2003):127-135.
This study concluded that “risk for death in schizophrenia was doubled on a background of enduring engagement in psychiatric care with increasing provision of community-based services and introduction of second-generation antipsychotics.”
Mad in America Documents
The evidence for antipsychotics
Antipsychotics and chronic illness
Antipsychotics and progressive brain dysfunction
Early death associated with antipsychotic drugs
Outcomes in the era of atypical antipsychotics
Modern experimental programs producing better outcomes












[…] these akathisia-, diabetes-, tardive dyskinesia-causing, brain-shrinking drugs with [at best] dubious efficacy forcibly slow-released in their bodies for a month. So Janssen has kindly provided several little […]
Report comment
[…] it or not, psychiatry hasn’t actually evolved much since then. The new drugs are not nearly as different from the old ones as most people have been led to believe- they’re even more harmful in some cases. The distinction between pharmaceutical companies […]
Report comment
[…] it or not, psychiatry hasn’t actually evolved much since then. The new drugs are not nearly as different from the old ones as most people have been led to believe- they’re even more harmful in some […]
Report comment