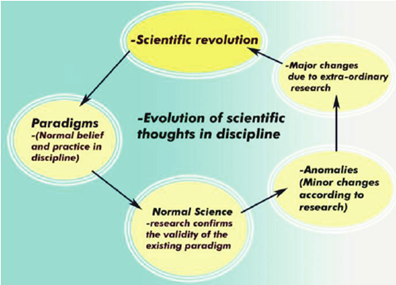
A recent peer-reviewed article delves into the scientific challenges within psychiatry’s biological paradigm of psychosis. The authors argue that the conventional view, which treats psychosis as a physical illness and emphasizes symptom-centered and drug-based treatments, prevents the field from evolving in our understanding and treatment of psychotic disorders. The article’s authors also considered the role that mental health nurses might play in moving the field toward a scientific revolution.
“In acknowledging this potential crisis, one also acknowledges an ‘essential tension’ between the safety of remaining working within the confines of existing paradigms and the risk of developing new theories and ways of understanding,” the authors write.
“This tension is likely to only increase as increasing numbers of those working within mental health services endorse a variety of theories and models in relation to psychosis. While risk-taking might be uncomfortable, scientific revolutions can only be resolved through exploration, debate, and experiments within and between paradigms.”
Published in the Nursing Philosophy journal, the article by Mark Pearson and colleagues from the University of Nottingham in the UK examines the state of psychiatric science and its relation to psychosis. They traced the history of the biological paradigm, highlighted major anomalies, and discussed the potential for a paradigm shift towards a more humane approach that values the voices of those who have historically been silenced and discredited.















If a thing which was called mental illnesses were pathological there would be a blood test and brain MRI. ıt is a hypothesis that it is pathological. psychiatry calls psychosocial events pathological and requsts to treat them with drug but
psychiatry can never treat with thing which is said a drug by psychiatry. psychiatry appoints a guardian and condemns the child to live with the family which is the source of psychosocial.
Report comment
To add how psychiatric nurses can impact patient care: host discussions about wellness, nutrition, sleep hygiene and managing stress within the inpatient setting. I have received support from management in discussing with patients whether or not to take psych meds.
Report comment
The Harding Longitudinal studies of the Vermont and Maine state backward hospital patients show up to 70% of no hope patients recover when they are removed from Psychiatric care, given a safe place to live and someone who believes in them. Psychiatry knows that their hospitals make many patients worse and respond with a revolving door philosophy. Until Psychiatry can uniformly achieve a 65 – 70% success rate with psychotic patients, research should be focused on what Psychiatry is doing wrong and why patients improved when removed from psychiatric care. Until then they have no right to do any other research.
Report comment