Editor’s Note: This article is being simultaneously published on our affiliate site, Mad in the UK.
This is intended as the first part of a look at pathways and outcomes in ‘psychosis’ and ‘schizophrenia’. Here, I discuss some of what’s not right in the picture for the current paradigm; an approach which, in essence, dates from the 1950s.

By way of introduction, let’s consider a finding from decades ago. In a previous piece on how psychiatric drugs can often tend to make things worse, I referred to a series of WHO investigations (see this pdf). These found better recovery rates from psychosis in lower income countries, compared with their richer counterparts. Known as the ‘outcomes paradox’ or as the ‘better prognosis hypothesis’, it has been considered a well established feature of the global epidemiology of ‘schizophrenia’. ‘Paradoxical’, because in contrast with healthcare outcomes generally being better in ‘developed’ (high income) countries, outcomes for those who had suffered psychosis were apparently better in the ‘developing’, lower and middle income countries.
…course and outcome for subjects in the developing centers were more favorable than for their developed world counterparts… even for subjects whose early course was poor, the likelihood of later recovery favors those in the developing centers…
At the time, the findings were attributed by researchers largely to cultural factors. Perhaps it was better social inclusion of sufferers that enabled recovery.
Subsequently, the picture was challenged. Critics dismissed the better prognosis hypothesis, pointing to contrary findings like much reduced life expectancy for those diagnosed compared with the general population in lower income countries. They argued that the supposedly more favourable sociocultural context in ‘developing’ countries, is often not to be found. There is, after all, plenty of stigma against those experiencing mental ill-health in both richer and poorer societies.
As trends of urbanization and migration gained pace in the ‘developing world’, some pointed to factors like these as much increasing a person’s risk of experiencing psychosis. So perhaps greater urbanization in the industrialized countries, as opposed to more rural living in the ‘third world’ was part of the explanation for the trend.
But to my mind there seems to be a neglected factor that could help explain the trend: different levels of the use of so called ‘antipsychotic’ drugs. As far as I’m aware, this has not generally been much considered in the literature on the outcomes paradox, with few exceptions.
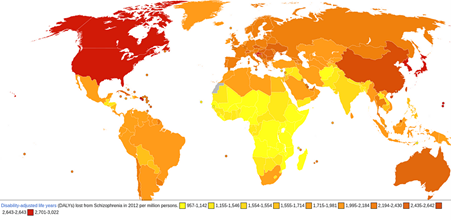
‘Schizophrenia’ Disability-adjusted life years, 2012 (Source)
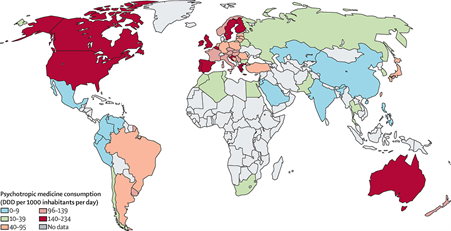
Here I take psychotropic medicine use in general as a proxy for use of ‘antipsychotic’ drugs. Data for 2008–19 (Lancet)
Loosely, one can see here some correlation between recorded levels of disability from ‘schizophrenia’ in the first map, and the levels of use of psychotropic ‘medicines’ shown underneath. The countries with the highest rates of psychiatric drug consumption (pink to red) also tend to have higher scores for disability from ‘schizophrenia’ (darker orange to red). For example, the US, Canada, Australia and Croatia all have high rates of psych drug use and high rates of this ‘disability’; whereas India and the Philippines score low on both scales.
The use of all classes of psychotropic drugs, has some limited applicability as a proxy indicator for the extent of ‘antipsychotic’ use. Attentive readers may notice that China would appear to be an exception to the trend, with a relatively high rate of disability, despite what is recorded by the Lancet as a lower rate of psychotropic drug use overall. This is most likely under-reporting. The Lancet data is based on sales data from European market research. China, obviously, has its own large manufacturing capacity. There is actually relatively heavy use of ‘antipsychotics’ there, as this paper concludes the “proportion of antipsychotic polypharmacy in China is higher than in many other countries…”
The hypothesis that prescription rates are likely a factor in the ‘outcomes paradox’ is lent some tentative credence, by a review of the WHO studies, which noted: “important findings common to many developing sites included: high percentages of subjects who had never received biomedical treatment…”
Due to the many factors at play over time, such as under or over-reporting, and the difficulty of making like for like comparisons, the better outcomes hypothesis remains controversial and open for debate. My arguments here won’t rely on it. The above isn’t intended as definitive, but to provide a bit of background on the outcomes debate and some illustrative context for what follows.
If we accept that the supposed sociocultural advantages in ‘developing countries’ may indeed not be present, the data does, however, seem to show that something is wrong with the conventional approach. If neuroleptic ‘antipsychotics’ are the solution, then we’d expect to see more favourable outcomes where they are used the most.
Another apparent finding of the WHO studies that was widely accepted in the literature, was that increased length of time without any appropriate care intervention for psychosis looks to correlate with a poorer long-term outlook for patients. This was widely taken by psychiatrists as supporting biochemical intervention with the use of ‘antipsychotics’ at the earliest opportunity. The conclusion that duration of untreated psychosis (DUP) was a key factor determining prognosis, would later be used to justify the mainstream innovation of Early Intervention in Psychosis (EIP) programmes.
Whilst accepting that a lack of any appropriate care intervention for those experiencing psychosis is undesirable, I intend to show here that ‘treatment’ for psychosis should not be taken as being synonymous with the use of neuroleptics; and that the conventional treatment model can result in a poor outlook, often quite avoidably.
As international comparisons can be open to contestation, I turn to same country data on long-term rates of clinical remission of symptoms and ‘functional’ recovery, after patients received ‘early intervention’. Data tends to show that longer-term functional (ie social and occupational) outcome measures appear no better for those who received EIP, than for those who did not.
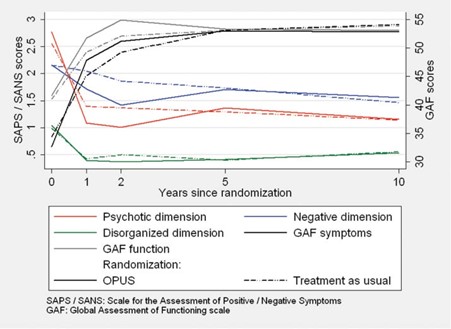
(Source: Ten year follow up of the OPUS trial…) Symptom and functioning scores showing that any initial benefits of EIP over standard treatment are lost by the five year point.
The evidence from the OPUS trial is that any benefits from EI are sustained only for the duration of the intervention, which in this case was 2 years. After this point, when patients are returned to standard mental health care, the difference between the two arms of the trial rapidly diminishes until there are no clinically significant differences.
Several reviews of the longer term effectiveness of EIP seem to agree that its advantages fade after the intervention has ended; noting that there is little evidence of ongoing benefit for recipients of EIP programmes over standard treatment after the intervention period of 2-3 years.
The mainstream response to this finding, insists there must be a ‘critical period’ after first episode psychosis (FEP) and the interventions just need to be sustained a bit longer to cover this period in order to realise the hoped for longer-term benefit. This hope appears to be forlorn, based, as it is on the consensus that ongoing treatment with neuroleptics prevents relapse. I’ll show that this consensus rests on shaky ground. And I’ll have some more to say about the ‘critical period’ and EIP in Part 2.
Something clearly looks awry with the orthodox paradigm. Before we continue let’s remind ourselves of a few of its key tenets:
- The dopamine hypothesis of schizophrenia — this argued back from the mode of action of the neuroleptics observed to calm disturbed patients. As the drugs blockade dopamine signalling, this was taken as indicating that schizophrenia symptoms therefore resulted from excessive dopamine signalling.
- Longer periods of untreated psychosis (DUP) correlate with poorer long-term outcomes. It was assumed then, that…
- The psychotic state amounts to a neurotoxic brain process. The idea being that if left untreated, it would damage the brain. Accordingly, it would be unethical for doctors to withhold drug treatment.
- Thus, neuroleptics are indicated for all cases of psychosis.
But there was always something lacking in the dopamine explanation. For instance, there is typically a time lag of weeks between the commencement of the dopamine blockading effect of neuroleptics and observed remission of clinical symptoms. If ‘psychosis’ is due just to excess dopamine, it would be expected to dissipate without such delay. Moreover, around 30% of patients will be deemed non-responsive to neuroleptics. At best, dopamine signalling can be said to mediate or regulate psychotic symptoms. This is not the same as accounting for their causal origin (aetiology). I delve further into reductive biochemical theories of psychosis in Part 2.
Returning to patient outcomes, a much cited 2013 study by Wunderink et al made the case for assessing social and occupational functioning, rather than just clinical remission of symptoms when looking at a treatment’s long-term effectiveness. The study found that patients with remitted symptoms after first episode psychosis would have better longer-term chances of functional recovery after drug discontinuation, or dose reduction, rather than maintaining standard treatment.
The psychiatrist Sandra Steingard concurred with the findings on recovery rates:
There are other studies that support Wunderink’s findings. Johnstone and colleagues conducted a somewhat similar study, known as the Northwick Park Study, in the 1980s. They randomly assigned 120 patients who had recovered from a first episode of psychosis to maintenance treatment with drug or placebo and followed them for 2 years. While the placebo group had a higher rate of relapse during this time, they also had an overall higher rate of employment. The authors wrote, “It suggests the disquieting conclusion that the benefits of active neuroleptics in reducing relapse may exact a price in occupational terms.”
Although discontinuation was associated with a higher chance of relapse, by the three year point in the Wunderink study the risk of relapse between the maintenance and discontinuation groups was equal. After five years the discontinuation or dose reduction group can even be seen to have a lower rate of relapse.
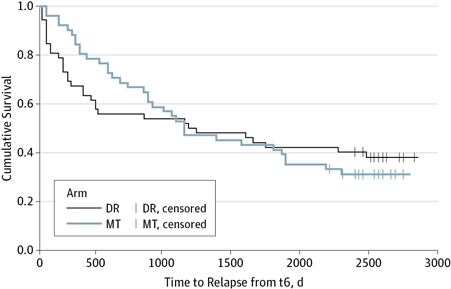
Despite experiencing fewer relapse events for the first three years, by five years the maintenance treatment cohort fares less well than the dose reduction cohort.
It appeared that maintenance treatment only prevented relapse over a limited time scale.* It remains the psychiatric consensus, however, that maintenance treatment is warranted, as it avoids relapse.
In what does this apparent benefit consist? I contend that much of it is a comparative statistical effect generated by drug trial participants suffering ‘rebound’ effects from drug withdrawal. This tends to happen when, according to trial protocols, participants are switched from their prior neuroleptic treatment to placebo within an unduly short time-frame. Taking this properly into account would suggest, that much of the evidence base supporting ‘maintenance treatment’ is skewed and distorted.
It is not uncommon in the UK, for patients in remission after a first episode of psychosis to be told that if they continue taking antipsychotics for two years, this will minimize their risk of relapse going forward. I believe such guidance to be ill founded. Essentially, it just reflects the fact that the trials on which the guidance is based, typically have only a two year follow-up period.
Trial participants are usually drawn from those already taking medication rather than drug naive patients. The placebo group is withdrawn from the antipsychotic with a short taper and washout period. Whilst the antipsychotic group is simply maintained on their pre-existing drug regime. Here is a typical 4-week taper schedule, as used in the STOP Psychotic Depression II trial:
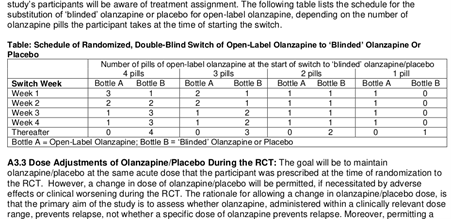
(From the Pharmacotherapy Protocol for the STOP PD II Trial)
A 4-week taper can be considered an abrupt taper. In fact eight trial participants in the placebo group ‘relapsed’ within that short tapering period. The majority of the ‘relapses’ in the placebo group then occurred within 12 weeks of the start of the taper.
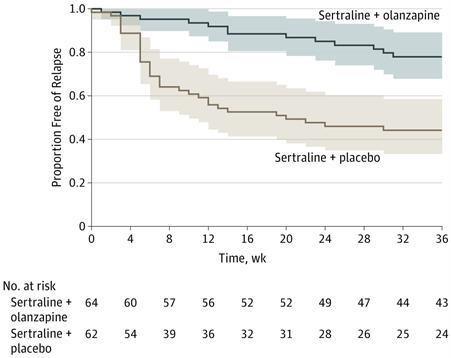
(The STOP PD II randomized clinical trial) ‘Relapses’: The bulk of those in the placebo group happen within two months of the end of the taper.
By around 14 weeks the rates of relapse in the olanzapine and placebo groups are seen to have roughly equalized. This closeness in time of the ‘relapses’ in the placebo group to the drug discontinuation phase, and their subsequent levelling off, suggests that the bulk of them could have been due to withdrawal effects. This is not an uncommon phenomenon in trials of antipsychotics. Mark Horowitz found that “[i]n one meta-analysis, 60% of all relapses over 4 years occurred within 3 months of drug cessation.” This supports the objection that many of these ‘relapses’ likely arise from drug withdrawal effects.
Horowitz explains what can happen:
Withdrawal-associated relapse has been attributed to neural adaptations to long-term antipsychotic treatment (dopaminergic hypersensitivity) that persist after antipsychotic cessation…This hypersensitivity to dopamine may render patients more susceptible to psychotic relapse when D2 blockade is diminished by antipsychotic dose reduction.
The brain compensates to the dopamine blockading effect of the drug, by increasing the sensitivity or number of dopamine receptors. If the drug is then ‘washed out’ of the system, there will likely be a disruptive surge in dopaminergic signalling, among other effects.
‘Supersensitivity psychosis’ can occur in people with no psychiatric history during withdrawal from off-label use of the drug. This phenomenon is also thought to play a role in some cases of ‘treatment resistance’. The theory being that, for some people, as their brains adapt to the cumulative exposure, any capacity of the drugs to ‘tamp down’ dopamine signalling is effectively cancelled out, by the greater sensitivity arising from increased receptor density. Signs such as closeness in time to drug discontinuation and symptoms of a more somatic character may indicate that an apparent ‘relapse’ may be a drug withdrawal syndrome, and hence, not necessarily a resurgence of some ‘underlying condition’.

Neuroscientific researchers have linked dopamine dysregulation to disrupted filtering of sensory information, associated with what they call ‘diminished functional connectivity’ between brain regions. They hypothesize that the ‘aberrant salience’ considered characteristic of the phenomenology of psychosis, may be due to this reduced ‘functional connectivity’.
One of several papers that came out of the STOP PD II trial argues that olanzapine stabilizes such ‘functional connectivity’. Participants were given MRI scans at the start and end of the trial, or if they relapsed.
Overall, functional connectivity between the secondary visual network and the rest of the brain did not change in participants who stayed on olanzapine but decreased in those switched to placebo… this suggests that olanzapine may stabilize functional connectivity…”**
But as we have seen, the effects found in the relapsing placebo participants look, most probably, to be the results of ‘antipsychotic induced dopaminergic hypersensitivity’ and abrupt withdrawal.
Nevertheless, the takeaway headline about STOP PD II was that taking olanzapine for 36 weeks ‘sustains remission’. The UK public health research body NIHR parroted that remitted patients benefit from continuing on olanzapine. By the same logic one would conclude that maintenance treatment with benzodiazepine sleeping pills was indicated for everyone who had been treated for insomnia!
As trial designs like this tend to be the rule rather than the exception, a large part of the evidence base supporting maintenance use of ‘antipsychotics’ can be seen as unsoundly based on poorly informed trial protocols.
But what happens when, instead of trials based on withdrawing antipsychotics from those already accustomed to taking them, a trial is carried out with drug naive participants. This trial at the Orygen centre in Melbourne, Australia indicated that psychosocial intervention alone could, for some, be sufficient to remit clinical symptoms:
“In the highly selected sample recruited to this study, psychosocial treatment alone was not inferior to psychosocial treatment plus antipsychotic medication at the end of the intervention period, raising the possibility that some young people with early psychosis may not require antipsychotic medications to recover.”
The psychosocial interventions had comparable clinical efficacy with administering neuroleptics. Additionally, when MRI scans were performed they showed the ‘aberrant functional connectivity’ associated with psychosis could be ‘normalized’ in drug naive patients, when they received placebo pills and intensive psychosocial intervention over three months; suggesting that psychiatric drugs may often not be necessary in order to resolve such ‘abnormalities’.
The findings are instructive in reminding us that biochemical interventions are not the only modality for affecting brain processes. Given that the human brain is the most complex object known to science, and that how it produces consciousness still remains a mystery, it is probably best that such narrowly reductive biochemical interventions are kept to a minimum. The history of harm caused to patients by psychiatric treatments more than amply testifies to the dangers.
In Part 2, I hope to show how changing assumptions about diagnosis and causality can provide a basis for reappraising treatment interventions, with the aim of minimising ongoing iatrogenic harm. But to wrap up this part of my discussion:
Why does long-term use of neuroleptics correlate with poorer social and occupational outcomes? As surmised by Wunderink et al, their prolonged use “might compromise important mental functions, such as alertness, curiosity, drive, and activity levels, and aspects of executive functional capacity to some extent.” Dopamine is generally acknowledged to play a role in motivation and ‘reward related behaviour’. I’ve noted before the flattening of emotion and expression that neuroleptic drugs tend to produce.
But, that is not all. Perhaps the most important finding of the STOP PD II trial is that olanzapine exposure thins the brain’s cortex:
“…exposure to olanzapine compared with placebo was associated with significant decreases in cortical thickness in the left hemisphere and the right hemisphere.”
The researchers assessed that 36 weeks of exposure to olanzapine would result in a 1.2% loss of a person’s cortex, which reconfirmed the results of previous animal studies where lab monkeys exposed “for 17 to 27 months lost roughly 10% of their total brain volume, both gray and white matter…”
Although STOP PD II study papers acknowledge that reductions in brain volume are “typically interpreted” as undesirable, the trial is taken as demonstrating the benefit of continuing with olanzapine. The cost of ‘sustaining remission’ for 36 weeks is just 1.2% of your cortex. Good deal, huh?
Needless to say, there are many other drawbacks and morbidities*** associated with long term use of ‘antipsychotics’. When one considers this and the above effects together, is not altogether surprising that social and occupational prospects can be dimmed in those kept on standard treatment.
Notes:
* The recent RADAR trial in the UK showed at its two-year mark that; although, more relapse events occurred in the discontinuation group, this group did not show worse ratings for clinical symptoms or functioning than the maintenance treatment arm. It is not clear to what extent the trial was able to incorporate the most recent guidance on ‘hyperbolic tapering’ and deprescribing. I cover some of this guidance in the following parts. Also, it should be noted that the trial took place amid the Covid19 pandemic and restrictions. Both the virus itself and the lockdown restrictions have been linked with raised risks of mental health difficulties.
** In fact this finding from STOP PD II was a lesser, secondary one and not the primary outcome on ‘functional connectivity’ that the neuroscientists had been hoping to see.
*** The work of Mad In America and its founder Robert Whitaker has helped pave the way for wider public awareness of the harms caused by a culture of psychiatric overdiagnosis and prescribing. Among other leading voices that have influenced my thinking are David Healy, Richard Bentall, Peter Breggin, and Joanna Moncrieff.












Great blog, Neil, thank you.
Forgive me for repeating my medical research findings re: the “schizophrenia” symptom “treatments.” The positive symptoms of “schizophrenia” (“psychosis” and “hallucinations”) can be created, via anticholinergic toxidrome.
https://en.wikipedia.org/wiki/Toxidrome
And the negative symptoms of “schizophrenia” can be created, via neuroleptic induced deficit disorder.
https://en.wikipedia.org/wiki/Neuroleptic-induced_deficit_syndrome
And when the so called “cure,” actually creates the symptoms of a so called “disorder.” That means the “illness” is an iatrogenic “illness,” NOT a “genetic illness.” And this explains why the “wealthy” countries that are pushing these neurotoxins onto the masses, for profit, also have the highest disability numbers.
And I will say I did, not too long ago, help a loved one dealing with non-psychiatric malpractice, heal from the worst “psychosis” I’ve ever seen (and that comes from one who has been in a “mental hospital”) … with a mere low dose of lithium (albeit, it did take a couple days longer).
I agree, alternatives to the systemic use of the psychiatric neurotoxins, are definitely needed. Some families (or most) don’t react well to the psychiatric neurotoxins.
And we here at MiA should work together to get direct-to-consumer pharmaceutical advertising made illegal in this country again.
Report comment
Thank you
Report comment
The reason for the disparity is obvious: people in ‘developed’ countries have more access (money) to pharmaceutical poisons. And pharmaceutical poisons can make you sick.
[Duplicate comment]
Report comment
The reason for the disparity is obvious: people in ‘developed’ countries have more access (money) to pharmaceutical poisons, and pharmaceutical poisons can make you sick.
Report comment
Mr. Broatch,
Thank you for an accurate view of antpsychotic damage, during & after ‘treatment’.
I was falsely diagnosed bipolar 1 in 2004 thanks to the infamous DSM-IV, Frances Allen-led corruption & my psychiatrist’s financial-conflict-of-interest (OpenData.gov), immediately drugged aggressively with antipsychotics, anticonvulsants, benzos (‘sleep-aids’), & ‘mood-stabilizers’, everyday for the following 12 years. My addiction and the side effects were profound.
I lost everything of meaning: my friends, family, job, home and sense of safety in the world. I quickly became bankrupted & homeless at 54 years old.
My psychiatrist applauded my “med-compliancy”.
12 years later, I forced a doctor-guided, 2.5 year withdrawal following an avoidable anaphylactic event (leveraging their liability)-ironic in the light of prior equally serious side effects… 2 NMS events, myocardiopathy (declared “fatal” in hospital)…and much more, for the entire 12 years (“treatment-resistant” poster-child!).
I also had them ‘change’ their diagnoses to NOS- mood-disorder & anxiety (no sh*t)…in writing.
My last dose of any psych drug was March 2016. My first seizure ‘event’ was April, followed by 18 more for 2 years. Cardio, neuro, and advanced brain institute testing & interviews followed….NONE receptive to pointing towards 12 years of psych drug effects! I brought reprints of clinical findings to wholesale, nervous indifference…avoiding the elephant in the room. They would NOT implicate another prescriber…even obliquely.
*Had I been a street-drug addict, it would have been the ONLY topic regarding cause, damage, & assistance.
I was met with annoyance & limited pursuit followed by ‘Good luck & good bye”. The polite vibe was that I was STILL seriously mentally ill, in denial…so sad.
I ‘treated’ my brain-damage (pre-frontal focal lesion manifested by micrographia) and drug-free re-entry into the world, in addition to a very difficult PTSD (exit doctor description) outrage that had no one to commiserate with…as “lifetime” labels are brutally enforced, no challenges tolerated.
I also found an indifferent world and hostility from some members of the psychiatric-reform community. I thought my story would inspire HOPE, not snark.
Escape, self-rescue WAS possible.
*As my withdrawal & their removal of a ‘lifetime’ diagnosis and treatment (the industry’$ foundational dogma) was a secret in the industry, done to avoid a public kerfuffle in a 2nd-tier city-a threat nonetheless, it screamed loudly of their own acknowledgement of life-ruining mistakes made, the patient-sacrificing paradigm that disturbs no one, and most-importantly, their lack of conviction in their own “evidence-based” ‘science’.
“Lifetime SMI and drug treatment?….not if you’ll shut up and go away.” (After the statute of limitations expired)
I wrote about it (RxISK, MIA-2018-2019) with the American Psychiatric Association as a directed contact, offering it to local & national media, or specialized investigative journalists, including 60 Minutes, WAPO, NYT, & (then & recently) Propublica. I constantly look for local psych-survivor/resistance groups to collaborate with. I have found none.
My experience proves the fraud.
I stay engaged in the fight for SAFETY and exposure of targeting vulnerable people looking for help and the resulting exploitation for profit…and ruined lives.
I want my story to be of use. Paula Caplan was the singular support I needed & gratefully received. She is gone and I am out of ideas. At 73 years, my energy is starting to ebb a little.
Thank you very much for this accurate, well-developed piece.
Report comment
Thank you. I understand a little what it means to have your viewpoint and experience written off. And I think you’re right to bring up the contrast with the drug addiction field. There “recovery” means getting free from mind altering substances. Whereas in the mental health field it tends to mean remaining on them indefinitely.
Report comment
‘Anitpsychotics’ interfere with the psyche’s ability to naturally restore itself, which can happen, given enough time and favorable circumstances.
Aggressively ‘treating’ psychotic episodes with neuroleptics for years (or any amount of time for that matter) assaults the human body, and mis-perceiving withdrawal effects as a ‘recurrance of the original illness’ is not just a mistake, it is a crime.
Report comment