Peer Power: Instant magic?
A few years ago, I participated in a workgroup wresting with scenarios focusing on shared decision making and resolving disagreements between psychiatrists and their patients. I’ll never forget how our small group noted that the solution to each scenario’s conflict was to “Bring in the peer!” as if the peer had some magical ability to resolve conflict by moving the patient to agreement. By day’s end, we were sarcastically singing “Bring in the peer to save the day!”, creating a new super hero theme song.
That memory reminds me to closely examine what we do as peer providers, administrators of peer run agencies, and trainers of peer specialists so that we do not veer from the core principles of self-help and our ‘peer-ness’ within this field of mental health.
Does ‘membership’ equal recovery?
Around the country, consumers of the public mental health system speak of ‘empowerment’, ‘recovery’ and ‘independence’ while being disempowered, and made reliant on a system that uses the word ‘recovery’ as only a buzzword. Mental health programs refer to the people they serve (clients) as ‘members’ – life long members in a club that given the choice, most would not choose to join. Yet our peers demand that their wellness, recovery and socialization groups stay in the mental health centers or drop-in (really drop-out) centers. Further, our peer-run organizations are primarily funded by local or state mental health departments and certified peer specialist are paid via billing their state Medicaid.
As a director of a peer run organization funded primarily by our county department of mental health, I have to wonder if we are walking our own talk or are just mirroring what we learned from being a part of the public mental health and SSI entitlement system in which many folks are/were literally system lifers.
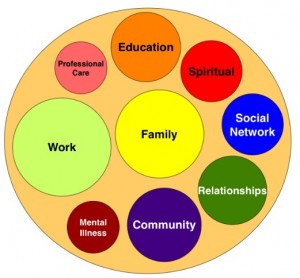
 When our peer groups meet in the mental health centers, I contend the ‘illness’ becomes the center of our lives. We are missing the opportunity to lead full rich lives; explored and celebrated in places that thrive naturally within our community. Wellness Centers offering programs such as yoga and art are a step in the right direction, however, they are akin to ‘drop-in’ centers that drop people out of the same activities occurring in their neighborhood churches, community centers, and YMCAs. Once again, the ‘illness’ is the commonality bringing people together all day, every day for what appears to be forever.
When our peer groups meet in the mental health centers, I contend the ‘illness’ becomes the center of our lives. We are missing the opportunity to lead full rich lives; explored and celebrated in places that thrive naturally within our community. Wellness Centers offering programs such as yoga and art are a step in the right direction, however, they are akin to ‘drop-in’ centers that drop people out of the same activities occurring in their neighborhood churches, community centers, and YMCAs. Once again, the ‘illness’ is the commonality bringing people together all day, every day for what appears to be forever.
Hanging onto the safety net
As we educate and support the people we serve about independence, self-reliance, interdependence and taking advantage of what’s in our natural community, we meet a great deal of resistance. People receiving services in the public mental health system are justifiably fearful of leaving a world that has cared for them, kept them safe, and provided for their needs in the midst of a very fragmented health-care system. The system has ‘welcomed’ them as members when their natural community would not. This has created what we all so desperately want and need – a sense of belonging and community but also reliance and centered-ness in their lives. It is not easy to help people see that they have been duped. This is happening both nationally and internationally.
Moving toward independence
As peers and peer-run organizations, we look to the system for our very sustenance, proclaiming that this relationship and the receipt of funding legitimizes and professionalizes our work as peers. I advocate for our programs to move towards true self reliance, independence and empowerment. I’m not in agreement that all of our peer services should be reimbursed by state Medicaid. This would be a bastardization of the meaning of our work as peers. We must work together to determine which peer services fit with the requirements of Medicaid billing and work toward diversifying our funding to maintain our independence.
‘Bring in the Peer’ must be more to the mental health system than window-dressing that communicates “recovery spoken here” to its constituents and the community. ‘Bring in the Peer’ creates the opportunity to support people in moving through the system with the ultimate goal of leading independent, healthy lives. As we rethink psychiatry, ‘Bring in the Peer’ also means collaboration between peer leaders, providers, and mental health organizations to promulgate the practice of true recovery both inside and outside of our mental health systems.
Moving forward: Collaboration in Los Angeles County
 One good example of such collaboration is the ICSC pilot project sponsored by the California Institute of Mental Health (CiMH) in Los Angeles County. Using the Institute for Healthcare Improvement’s Breakthrough Series, the collaborative brought together peer leaders, people currently receiving services, program directors, providers and peer advocates with the aim of assessing how our services keep people ‘stuck’ and improving services that increase ‘client flow’ through the system. This ICSC project yielded improvements in our LA County provider organizations’ capacity to serve new clients, by increasing the rate of flow to higher levels of recovery (lower levels of care), as well as transitions out of the mental health system into the community.
One good example of such collaboration is the ICSC pilot project sponsored by the California Institute of Mental Health (CiMH) in Los Angeles County. Using the Institute for Healthcare Improvement’s Breakthrough Series, the collaborative brought together peer leaders, people currently receiving services, program directors, providers and peer advocates with the aim of assessing how our services keep people ‘stuck’ and improving services that increase ‘client flow’ through the system. This ICSC project yielded improvements in our LA County provider organizations’ capacity to serve new clients, by increasing the rate of flow to higher levels of recovery (lower levels of care), as well as transitions out of the mental health system into the community.
The true magic of peer support
The efficacy of peer support is well documented and peer programs such as Wellness Recovery Action Plan are considered evidence-based practices. Thus it is imperative that the use of peer provided services be included within our mental health system. This must be done in a way that does not restrict what we do as peers based on ‘medical necessity’. To be truly effective, the focus must be on the person and not the diagnosis. While our professional colleagues are constrained by ‘billing’, as peers we need the freedom to provide support by doing with rather than doing for.
By ‘Bringing in the Peer’ together, we can help to bring out the whole person.
















You raise a lot of interesting issues, including about independence of peer organizations. It’s only when an organization is financially independent of a system, that it can serve as a fully effective advocate for people who are being abused in that system – or even as an independent voice to disagree with practices in the system that are not conducive to well being.
We need creative solutions to financing our organizations, including working grass roots as volunteers which some of us are doing, and also seeking funding from foundations which is happening as well.
Good luck and thank you for this blog.
Report comment
Thank you Tina.
I am finding that fund diversification within the mental health field has everyone venturing in new unchartered territory. This will indeed require Peer Run Organizations to think about issues of fund diversification, creative solutions such as volunteering to offer services and collaborations to help stretch funds further to maximize what we do.
And of course it is really important that we measure what we do (outcomes) as that is not only helpful to monitor how we are doing but it also helps to secure funding.
Hoping people are willing to share creative ideas 🙂
Keris
Report comment
“The efficacy of peer support is well documented and peer programs such as Wellness Recovery Action Plan are considered evidence-based practices. Thus it is imperative that the use of peer provided services be included within our mental health system.”
I found this statement rather puzzling as a 2009 meta-analysis (Systematic Review of Peer Delivered Services Literature 1989 – 2009: http://www.bu.edu/drrk/research-syntheses/psychiatric-disabilities/peer-delivered-services/) cited on the “Recovery Within Reach” site – http://www.recoverywithinreach.org/peersupport/peersupportresearch – doesn’t seem to support such a conclusion. Here’s the plain language summary:
“Peer delivered services for individuals with severe psychiatric disabilities are based upon the premise that an individual with a “lived experience” is uniquely able to contribute to the rehabilitation and recovery of a person needing services. Peer delivered services have proliferated greatly in the past decade to the point where they are now an accepted component of mental health services and programs in many states. Peer services are an outgrowth of the consumer movement which emphasizes that mental health policies and services should embrace a philosophy of “nothing about us without us” and that there should be dignity, equity and mutuality in all helping relationships. Despite the proliferation of peer run services, there is no accepted or widely used typology of peer delivered services which both hampers the field and complicated this systematic-review. For this review, we divided the studies of peer services into the following categories and report the plain language summary in the same way: peer delivered services added to traditional services; peer delivered services offered in mutual support groups; peer delivered services in the context of drop in centers; peer delivered services offered primarily in a one-to-one service, peer delivered residential services and other.
Results of this review suggested that adding peer delivered services to traditional mental health or to case management services does not result in significant differences in outcomes that favor the peer delivered services over traditional services. A small number of studies indicate advantages of peer delivered services in engagement and retention of individuals in services, but not in outcomes. These results suggest that peer providers may offer unique and distinctive skills and experiences that can be helpful in the engagement and retention of individuals in services however, that evidence is modest. There is also evidence that peers provide services differently in terms of the focus on face-to-face interactions outside of the traditional office milieu. Taken together, these studies do not provide clear evidence that peer delivered services provide advantages in terms of client outcomes such as employment, perceived social support, criminal justice involvement, housing stability, working alliance, service use, re-hospitalizations, quality of life, or substance abuse. Several authors have suggested that these results should be interpreted as supportive of the notion that peer providers can deliver equivalent services to those of professionals, rather than expecting peer delivered services to out-perform traditional services.
There is some evidence that peer delivered services, provided in a group context, can be effective in engaging individuals and in improving outcomes. The peer delivered group interventions vary substantially one from another, making conclusions difficult to draw in this category. The data do suggest that individuals who adhere to group interventions (i.e., attend a substantial number of sessions) appear to benefit whether the intervention is more tradition in nature, is similar to AA, or a different model altogether. However, conclusions from randomized designs using intent-to-treat analyses (i.e., involving all subjects randomized) do not reveal significant positive outcomes. Observational and correlational studies, such as those done in drop in centers or in Double Trouble for Recovery groups, suffer from problems with attrition and loss to followup. Despite this, it is safe to conclude that of those people who engage in peer delivered interventions in groups regularly, benefits do accrue in the areas of abstinence from substance abuse, stability of psychiatric symptoms, self esteem, self efficacy, empowerment, quality of life, perceived social support, satisfaction with services, medication adherence, reduced criminal justice involvement. The extent to which attrition and selection factors affect these outcomes cannot be estimated, but do pose a threat to these conclusions.
For the one large study of peer delivered interventions using multiple models (drop in centers, mutual support groups, and education and advocacy) and multiple sites, there is evidence that participation in a peer delivered intervention was associated with global positive changes in well-being. In terms of peer delivered residential interventions there is equivocal evidence of outcomes when examining level of functioning, quality of life or other outcomes. In two studies of a primarily one–to-one peer delivered service focusing on social supports there is no consistent evidence of effectiveness. Service satisfaction, however, does appear to favor individuals receiving peer delivered services.”
Furthermore, a 2010 meta-analysis by Pfeiffer et al. “Efficacy of peer support, interventions for depression: a meta-analysis” – http://www.preparedpatientforum.org/research/support_021711.pdf – reaches a more careful and measured conclusion:
Abstract
Objective: To assess the efficacy of peer support for reducing symptoms of depression.
Methods: Medline, PsycINFO, CINAHL and CENTRAL databases were searched for clinical trials published as of April 2010 using Medical Subject Headings and free text terms related to depression and peer support. Two independent reviewers selected randomized controlled trials (RCTs) that compared a peer support intervention for depression to usual care or a psychotherapy control condition. Meta-analyses were conducted to generate pooled standardized mean differences (SMD) in the change in depressive symptoms between study conditions.
Results: Seven RCTs of peer support vs. usual care for depression involving 869 participants were identified. Peer support interventions were
superior to usual care in reducing depressive symptoms, with a pooled SMD of −0.59 (95% CI, −0.98 to −0.21; P=.002). Seven RCTs with 301 total participants compared peer support to group cognitive behavioral therapy (CBT). There was no statistically significant difference between group CBT and peer interventions, with a pooled SMD of 0.10 (95% CI, −0.20 to 0.39, P=.53).
Conclusion: Based on the available evidence, peer support interventions help reduce symptoms of depression. Additional studies are needed
to determine effectiveness in primary care and other settings with limited mental health resources.
Published by Elsevier Inc.
Report comment
Gitty-
You are raising some really good points about the dearth of research which of course means that we need more research. Here (the topic of research and being involved in research) is where I think Peer Run Organizations worry about being copted because we have experienced outcome reasearch that in the past has not resonated with our definitions of “outcomes”/ “wellness” and /or reminds of us of our lives under the microscope (many talk about feeling like guinea pigs to be studied rather than people to be assisted/supported). Recognizing our own filters about “research” and “outcomes” is important as is participating in and developing more research to measure what we do as peers and its effectiveness – not to determine if traditional or peer services are better than each other – but, as I stated in my blog and where you quoted in the first line of your comment, how they can be incorporated into exisiting mental health treatment as well as stand alone when people have transitioned out of the mental health system.
There are also some other great outcomes to think about related to peer services related to the wellness, self-esteem and “recovery” of the person providing the peer support service.
In a later comment, I will list more research that addresses some of your concerns as well as some other interesting outcome measures of Peer Support.
Thanks so much for your comment.
Keris
Report comment
peer support is a vexed problem. Here in the UK some peer supporters employed by hospitals and healthcare providers do just about the same job as nursing support staff (the entry level, unqualified jobs in mental health). They sometimes cajole medication on patients. A trainer said they should not do that and promptly lost the job as a trainer.
Services push the idea of peer support but don’t really change the ethos of the services they deliver and the peer supporters they employ are steeped in the medical model. So something which I suspect started as a valiant attempt by service users to humanise the service may well have been co-opted in many parts of the UK, if not the rest of the world.
I went on a peer support course for my local drop in centre and it was so bad I wrote a letter of complaint with some ideas of how it could be improved. It had been designed by someone from the services and it showed. It was based on some simple counselling ideas (but 10 minutes counselling practice is pretty useless for most people), some simple life coaching ideas (about 5 minutes of practice was given), some ideas about signposting to other services, a list of diagnosis to learn (eg depression, schizophrenia, bipolar, anxiety) and the “correct” treatments (a list of drugs), there “side effects” and possible alternatives (like talking to people, otherwise known as therapy). Nothing on trauma and nothing on how people actually help each other (putting each other up when homelessness is looming, taking late night phone calls, going for walks in the park, going to the meeting with the awful shrink, encouraging each other to get the treatment we need when the services want to discharge us, help with claiming benefits and all those other kindnesses, big and small, which we do for each other). Nothing on critiquing the services and sharing our experiences of good and bad services and how to avoid the bad ones and access the good ones and a strong suggestion that people should be referred to services for long term care and in any crisis when a lot of peoples experiences are that services are often neglectful and sometimes harmful.
Peer supporters in the day centre really like being employed there, it gets them out of the house, give them a bit of money and a sense of purpose. It can be a road back to proper employment, and therefore, to use the buzz word, a road to recover. But I fear that the people who get the most out of peer support are the peer supporters. The basic ethos of the centre has not changed much since it changed to being staffed mainly by peer supporters, it is still dominoes, tea and maybe a patronising, sometimes friendly chat.
Sometimes I spend time listening to the members of the day centre, usually because I am researching a theatre project where professionals are helped to understand the experiences of service users. It often turns into something like a therapy session. People calm down and often open up about the traumas that caused the initial breakdown. Often I get the impression that this is the first time people have talked about their traumas despite years of using services.People often look at me after that like they could use some more of my time, but I don’t usually offer it because I know I would need support myself to deal with it all. I would do it if proper support was on offer, I might even do it on the near minimum wage of a peer supporter.
When we put on the plays about service users experiences and then lead discussions on the issues the day centre members start expressing opinions very vocally in ways that the centre workers have not seen very often, if at all. People who might easily be seen as institutionalised often passionately contribute to the discussion. Real peer support starts to emerge. But this is not taken up by the service despite their promise to involve members more and listen to what members want.
In peer support it is important to remember that He Who Pays the Piper Pays the Tune.
I don’t really care who offers me support. I believe that what works is building trusting relationships, working through traumas and building an active community. I have been part of communities that do this in other settings, ie not mental health, but I think it is entirely possible to make this work with peer supporters, but what is on offer at my local day centre, of peer supporters offering tea, dominoes and a few social activities, is not really going to help many people “recover” in the full sense of the word, of having no or few symptoms, having an active life and playing an equal and active part in the community.
Report comment
John-
Your comment illustrates the very point of my blog. I think there is value in serving tea and playing dominos as it helps people who struggle with socializing gain skills in an environment and with people who are understanding, patient and have “been there, done that” as peers.
But if that is all that is available for everyone – it not only becomes a “one size fits all” approach but it also minimizes the role of peers AND so unfortunately reduces services that people receive that could aid in their recovery.
I also like that you state that support for you can come from anyone that builds a trusting relationship with you– what a great reminder that meeting a person where they are is most important! Not everyone is into peer support while others find it a crucial part of their recovery.
A reminder of the complexity of individuals requires flexibility and many choices/options to support folks in their recovery.
Keris
Report comment
I don’t have too much trouble with tea and dominoes either, but it is the same people who play dominoes who, when I listen to them, open up, calm down and tell me about their traumas. And it is the same people who also come to the theatre based consultancy and for what may be the first time speak out and give critical opinions of the centre and it’s service. These are people who have used the service for years, if not decades.
Tea and dominoes are fine providing the staff use the opportunity to get to know the members in greater depth and then reflect on the members, how they are and what they are interested in, so they can then approach them in a different way to try and build these peoples confidence and help them move on.
It doesn’t happen, there is not enough reflective practice built into the system. So we see the same people using the service year after year, doing the same things.
it is a waste of peoples lives and in my opinion a waste of state money.
Report comment
Wow – yes indeed! If the staff are not using the dominos and tea times to interact, get to know people, and help them move forward with their lives – yikes.
Can I ask if there is a system, center and/or treatment assessment completed by “clients” at a local and national level?? And if so what happens to the feedback and data?
It is one thing to obtain feedback from people who receive services and guite another thing to give the results back to the Centers and people they serve and most importantly do something with the information (especially around improvements!
keris
Report comment
Keris, First I want to commend you in doing your blog, and the issue you raise is a critical one. “Bring in the peer” is indeed the system’s response to all its short comings. But that does not work. We need a change in the culture and operations at all levels. Until that occurs, the research on peer support will be meaningless. We peers can only work our magic in organizations that value and support the lived experience of recovery that peers can bring. The system needs to replace the medical model with an empowerment model, in order for peers to be effective. I am going to start a blog here on that topic.
by Dan Fisher, peer psychiatrist
Report comment
Thanks Dan. I might add that the research may be focusing on the wrong question and /or imposing models of analysis that do not fit with what peers do. Our work is not “model” based per se nor is it “programatic ” based (as in one size fits all, all peer groups services look alike).
Our ability to operate always from a person-first/human encounter individualizes our work.our work as you know isn’t about diagnosis but about people and their experiences. Empowering people we serve to direct and make choices results in our need and ability to be flexible. Yet in research design this called a challenge or seen as problematic.
When I tell people Project Return Peer Support Network has over 100 peer groups and they are all diffferent- it’s mind boggling for researchers (and lay people) to grasp. Our ability to articulate, measure and evaluate what we do is not so much a challenge but rather an opportunity to develop program evaluation and research methods that effectively work with/match what we do rather than continually using methods that may not be the best fit.
I think it will also help shift and broaden the conversation as will your blog.
Keris
Report comment