Editor’s Note: Over the next several months, Mad in America is publishing a serialized version of Peter Gøtzsche’s book, Critical Psychiatry Textbook. In this blog, he discusses that depression pills increase mortality, and that psychiatry mistakes withdrawal effects for relapse. Each Monday, a new section of the book is published, and all chapters are archived here.
Depression pills increase total mortality substantially
In 2015, I tried to find out how many people are killed by the three major drug groups, depression pills, benzodiazepines and similar drugs, and psychosis pills.7:307 I used the most reliable research I could find and restricted my analyses to patients at least 65 years of age. The estimated number of drug deaths in Denmark (population 5.8 million) based on current usage was 2831 for depression pills, 721 for minor tranquillisers, and 141 for major tranquillisers. I estimated that fluoxetine alone had killed 311,000 people worldwide in the age group 65 and above up to 2004.
 The high number of deaths on depression pills may be surprising. It is partly due to the fact that so many elderly people take them (12% in the age group 65 to 79 and 19% in those at least 80 years old).7:310 A UK cohort study of 60,746 patients older than 65 showed that SSRIs lead to falls more often than if the depression isn’t treated, and that the drugs kill 3.6% of patients treated for one year.447 The study was very carefully done, e.g. the patients were their own control in one of the analyses, which is a good way to remove the effect of confounders.
The high number of deaths on depression pills may be surprising. It is partly due to the fact that so many elderly people take them (12% in the age group 65 to 79 and 19% in those at least 80 years old).7:310 A UK cohort study of 60,746 patients older than 65 showed that SSRIs lead to falls more often than if the depression isn’t treated, and that the drugs kill 3.6% of patients treated for one year.447 The study was very carefully done, e.g. the patients were their own control in one of the analyses, which is a good way to remove the effect of confounders.
A textbook advised that in the elderly, we should try a depression pill even on a vague suspicion of depression because it can be difficult to distinguish between dementia and depression, and because the consequences for the patients are very serious if we overlook “this treatable condition.”18:121 This advice is deadly. Even if the death risk in the UK study for some reason was exaggerated, it is the best evidence we have, and we have an obligation to follow the evidence.
The psychiatrists are not keen to hear about how deadly their drugs are, and they did not communicate any data about this in their textbooks. Absolutely nothing.
In October 2017, I gave two invited talks at the World Psychiatric Association’s 17th World Congress of Psychiatry in Berlin.8:27 This was arranged by Peter Lehmann, a German reformer who wants to make psychiatry more human, with self-determination and less use of toxic drugs. He contacted the international advisory committee and urged them to invite “users/survivors of psychiatry” as speakers, which they did, and they also invited me.
I spoke at two symposia. One was an International withdrawal symposium that highlighted the increasing gap between knowledge about withdrawal problems and the lack of support for withdrawal. The other was Responding to the frightening reduction of psychiatric patients’ life expectancy.
When I spoke about withdrawal from psychiatric drugs, there were around 150 psychiatrists in the audience. The atmosphere was hostile, and several people asked irrelevant questions such as whether I believed that lithium worked.
Fifteen minutes later, I spoke at the other symposium and my title was Why are psychiatric drugs the third leading cause of death after heart disease and cancer?7 Three psychiatrists out of the over 10,000 at the congress attended. They refused to give interviews and carefully avoided being filmed by a documentary film team that followed me to Berlin, as if they were on their way to see a porn movie. This was a no-go zone. A taboo.
If you read the package inserts or look up relevant published papers, you will realise that psychiatric drugs have harms that can lead to falls and traffic accidents.448-453 These harms include sedation, dizziness, orthostatic hypotension, confusion, and impaired coordination and balance. Depression drugs double the risk of falls and hip fractures in a dose-dependent manner,452,453 and within a year after a hip fracture, about one-fifth of the patients will be dead.
These harms won’t be noticed by the doctors, as many people fall and break their hip anyway. The drugs are therefore silent killers, and doctors don’t learn anything from their much-overvalued clinical experience, which, in psychiatry, leads them astray more often than not.
Depression pills do not prevent relapse
It’s tricky that withdrawal symptoms and disease symptoms are often the same. If a drug is stopped abruptly or over a short period of time, and the patient becomes depressed, it doesn’t mean that the disease has come back.
However, when the patients have tried to stop taking their drug because of its harms or because they feel it doesn’t work, psychiatrists, other doctors, social workers, and relatives will usually tell them that the symptoms demonstrate that they still need the drug.
It’s an uphill battle to try to stop taking a depression pill,8 but usually, what we are seeing is what I call an abstinence depression. This term is a precise description of what happens, but I might be the only person to use this term. A search on PubMed with “abstinence depression” in the Title field yielded no records, and not even a Google search found any. I shall explain below why it is correct to say that patients become dependent on depression pills, even though mainstream psychiatry continues to deny this.7,8,90
My new concept should become part of the language psychiatrists use and should be included in the disease manuals. I define abstinence depression as a depression that occurs in a patient who is not currently depressed but whose depression pill is stopped abruptly or over a few weeks. Its hallmark is that the depression-like symptoms come quickly (depending on the half-life of the drug or its active metabolites) and disappear within hours when the full dose is resumed. Reintroducing the drug can therefore be regarded as a diagnostic test separating an abstinence depression it from a true depression, as true depressions do not respond quickly to depression pills.
A 1998 trial of 242 patients with remitted depression illustrates the difference between an abstinence depression and a true depression.45 After they had become well, the patients received open maintenance therapy with fluoxetine, sertraline, or paroxetine for 4-24 months. They then suddenly had their therapy changed to a double-blind placebo for 5-8 days, but the timing of the treatment interruption was unknown to them and their clinicians.
The investigators had developed a 43-item list based on withdrawal symptoms reported in the literature, and after the placebo period, patients were asked if they had experienced any of these. This checklist approach will tend to exaggerate withdrawal symptoms, and the study was funded by Eli Lilly, the maker of fluoxetine, which had an obvious interest in showing that fluoxetine causes fewer withdrawal symptoms than the two other drugs because of the very long half-life of its active metabolite, about one to two weeks.
The three most common withdrawal symptoms were worsened mood, irritability, and agitation, which are not signs of a relapse of the depression. As expected, relatively few people had symptoms on fluoxetine:
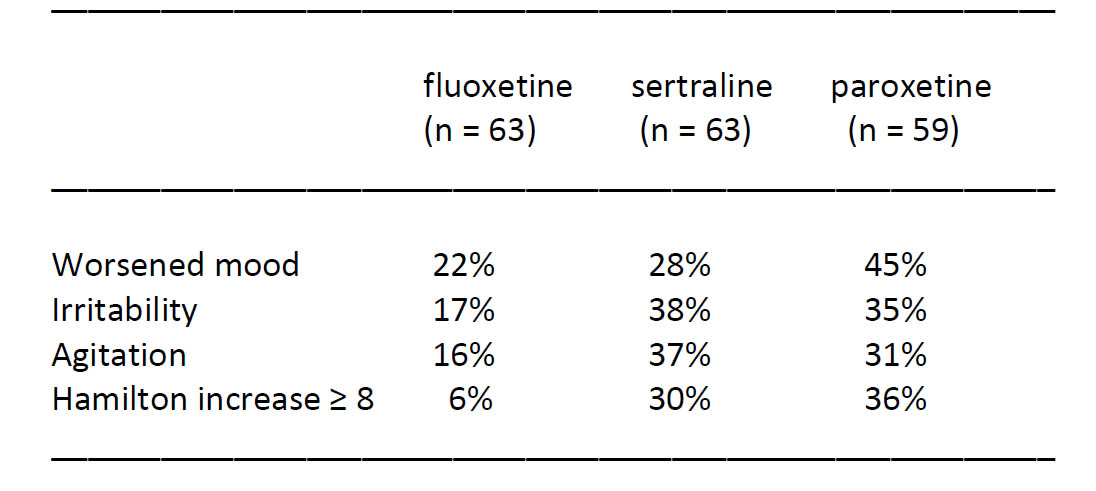
On sertraline or paroxetine, 40 of 122 patients had an increase in their Hamilton score of at least 8, which is a clinically relevant increase.
There would have been many more withdrawal symptoms if the drugs had been withdrawn for 2-3 weeks, particularly on fluoxetine, but even with an interruption of only 5-8 days, 25 of the 122 patients on sertraline or paroxetine fulfilled the authors’ criteria for depression.
This study shows why doctors get it wrong when they think the disease has come back. We might ask how many patients are likely to get a true depression in a random week in a group of 122 patients whose depressions have remitted. I worked this out based on a study of 362 high school students who had experienced one or more episodes of depression.454 Of the patients who recovered, 5% relapsed within six months and 12% within a year, which suggests a rather constant relapse rate over time. Using these data, I calculated what the expected number of patients relapsing is. This is 122 x 12% x 6.5/365 = 0.03, which suggests that not a single patient of the 22 that “relapsed” in Lilly’s study would have relapsed if they had not been exposed to a cold turkey withdrawal.
Two years later, Eli Lilly conducted another unethical trial with a similar design that harmed the patients.305 The abstinence symptoms after paroxetine withdrawal were severe. The patients experienced “statistically significantly worsened severity in nausea, unusual dreams, tiredness or fatigue, irritability, unstable or rapidly changing mood, difficulty concentrating, muscle aches, feeling tense, chills, trouble sleeping, agitation, and diarrhea during placebo substitution.”
The various harms the patients suffered because of Lilly’s cruel trial design increase the risk of suicide, violence, and homicide.7 This was known long before the trials were carried out.2,7,21
Unsurprisingly, the patients that had been harmed after withdrawal of paroxetine reported “statistically significant deterioration in functioning at work, relationships, social activities and overall functioning.”21
It is only in cold turkey trials I have seen such outcomes. According to the American Psychiatric Association’s disease manual, DSM-5, major depression is present when the patient exhibits 5 or more of 9 symptoms that “cause clinically significant distress or impairment in social, occupational, or other important areas of functioning.”8 Given how the disorder is defined, it makes no sense that drug trials avoid using these outcomes, which are far more important and relevant than a score on a rating scale. The reason is of course that the drug industry knows that their pills do not have positive effects on these essential outcomes.
Since psychiatrists usually confuse withdrawal symptoms with relapse, it is not surprising that two textbooks claimed that if the drug is stopped too early,16:276,17:661 it increases the risk of relapse, and one noted that at least 50% will relapse.16:276
The misconception leads to harmful advice about long-term treatment. A continuation phase of 6-12 months after remission is advised,16:276,18:126 and the longer, the better,16:276 e.g. by severe depression with imminent suicide risk.18:126 This advice is deadly. The drugs might push a patient in imminent danger of suicide over the edge. The same textbook claimed, with no references, that the preventative effect of psychotherapy is not so pronounced as that of drugs.18:126 This false information is also lethal7,272,381-385 because psychotherapy halves the risk of suicide.272
They claimed that if a patient has had two depressions within five years, the doctor should consider continuing with the drug for an extra year; if three depressions, for 5-10 years or lifelong.18:127 If onset after 50-60 years of age, the treatment should be lifelong because the risk of recurrence is almost 100%. It was claimed that an excellent preventative antidepressant effect is achieved. This advice is also lethal because of the high death rate in elderly people given depression drugs.7:310,447
The absurdities were endless. A third book recommended continuing with the drug for the same number of years as the number of depressive episodes.17:360 Even if we imagine there was a drug that worked for depression and prevented new episodes, it would be bizarre. The advice means that the poorer the effect, including no effect, the longer the patient should take the drug. If seven depressions, the patient would be “sentenced” to an additional seven years on the pill and be called treatment-resistant as well. This gives connotations to criminal law. The more treatment-resistant a criminal is, i.e. the more offences and jail sentences, the longer the last jail sentence will be.
Some pages later, the same book claimed that the risk of relapse in bipolar is about 85% but only 35% when medically treated.17:377 This is also wrong. All maintenance studies are seriously flawed as they measure withdrawal effects in the placebo group, not relapse.
It was claimed that quetiapine significantly reduces relapse of mania—which is unlikely to be true—and that such an effect has not been shown for other psychosis pills.16:305 It is even more unlikely that one psychosis pill, and not all the others, should work. This is plain wrong.436
This textbook recommended maintenance treatment already after a single manic episode, for 2-10 years or lifelong, unless caused by psychoactive drugs.16:305 It was not explained if this only means street drugs or could also be prescription drugs, but many psychiatric drugs can cause mania, including depression pills and ADHD drugs.7
The book explained that abrupt discontinuation always increases the risk of relapse because it is expected that the disease will last a long time.16:306 This statement is ludicrous. It is not because the disease will last a long time but because the patients get withdrawal symptoms. This has been described for all psychiatric drug classes.135
Gradual cessation over at least four weeks16:584,19:295 or a couple of months18:239 was advised, but only one book advised particularly small dose changes by the end.19:295 One book offered dangerously misleading advice, as it postulated that withdrawal symptoms could be avoided if the pills were discontinued over two weeks.17:360 Elsewhere in this book,17:660 the authors recommended what they called slow withdrawal over 1-2 months, which is not slow.8,136
According to the textbooks, about 20-30%18:239 or one-third16:584 will get withdrawal symptoms by abrupt cessation. This is not correct either. Half of the patients will suffer from such symptoms after depression pills, and in half of them, they will be very severe.136
The information about withdrawal symptoms varied but included dizziness, headache, tired-ness, gastrointestinal symptoms, influenza-like symptoms, insomnia, anxiety, irritability, agitation, sweating, sadness, increased dreaming, muscle contractions, and electric zap feelings in the extremities.16:584,17:360,17:660,18:239,19:295 Absent were the most serious harms, akathisia, increased risk of suicide and violence, and abstinence depression.
Two books claimed that the patients do not become dependent on depression pills,17:661,18:239 and one of them noted that, because of this, relapse should not be misinterpreted as withdrawal symptoms, and it added that recurrence will typically occur several weeks after stopping treatment.18:239 A third book noted that withdrawal symptoms usually occur within a few days, varying from one day to two weeks, and that the duration varies from a few days to several weeks.19:295
These statements are also wrong. Depression pills lead to dependence (see page 79), and withdrawal symptoms can occur much later, after months, e.g. if the patient becomes stressed, and they may last for years.8,136 Another book noted that one-third would get withdrawal symptoms if the drug was suddenly stopped and advised tapering over at least four weeks but did not explain how.16:584
In one book, the authors warned that about 40% of patients with bipolar stop treatment and that this carries a great risk of new episodes.16:296 Obviously, the patients don’t like the drugs but the psychiatrists don’t care.
The widespread professional denial of the drug harms patients experience was displayed when I mentioned on the TV news in 2011 that depression pills can change the personality. In a commentary to this, the president of the Danish Psychiatric Association wrote that it is misleading to focus on a side effect that is so scary for patients, and which is extremely rare.455
It isn’t. Six years earlier, Danish psychiatrists had published a study in which 43% of 493 patients agreed that the treatment could alter their personality and 42% that they had less control over their thoughts and feelings.89 82% agreed that as long as they took the pills, they didn’t really know if they were necessary. The patients’ replies correspond closely with what other researchers have found,308 but the Danish psychiatrists refused flatly to believe what the patients had told them. They called the patients ignorant and wrote that the patients needed “psycho-education.” However, the relatives had the same opinion as the patients about the pills. Perhaps they should also be taught they were wrong?
***
To see the list of all references cited, click here.












All readers please be advised that this is the opinion of ONE Doctor and does not reflect.the current evidenced-based best practices for treating clinical depression.
Please follow your own prescriber’s orders. The sun does not rise and set with Dr. Peter Gotzche’s opinion.
Report comment
Many people can’t survive without medication or electrical stimulations .
Many will conduct suicide without medication.
People just have to find the right medication. Staying without a proper treatment, if mentally imbalanced people may not have a normal life .
Report comment
The science does not support your assertions. No medication has been found to reduce suicide rates, and most antidepressants increase rates. Recovery rates have been shown to be LOWER when taking antipsychotics over the long term. Only 30% of users report significant benefits from antidepressants, which is barely more than benefit from placeboes. This is what the science says. Repeating mythology doesn’t make it true. How do you KNOW these things you have claimed to be true?
Report comment
That completely depends on the person in question and their circumstances. Yes, some people benefit from medications. Others are completely destroyed by them. It depends on a case-by-case basis.
Also, when people have legitimate practical problems (which many people who end up in the MH system globally do), trying to drug it away solves nothing.
I respect a person’s choice to go about their day taking meds if it’s helping them. But an equal amount of effort must be put into weaning people off these drugs when they’re doing more harm than good and when their problems have nothing to do with getting drugged.
Another question to ask. Why are they mentally imbalanced to begin with? Just “brain disease”? Nothing to do with circumstances? How can you fix those problems with pills?
Report comment