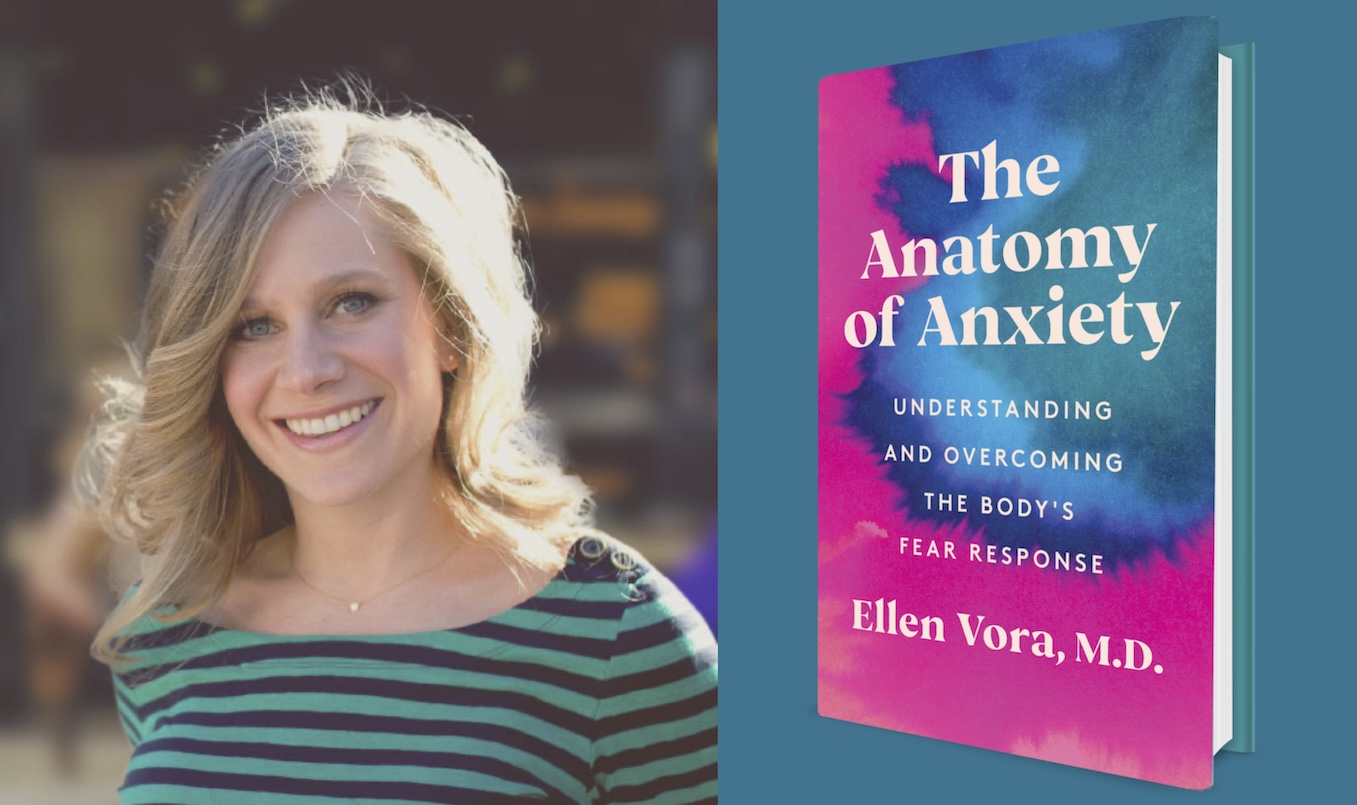
Ellen Vora is a board-certified psychiatrist, acupuncturist, and yoga teacher. She’s the author of The Anatomy of Anxiety and takes a functional medicine approach to mental health. She considers the whole person and addresses imbalance at the root. Dr. Vora received her BA from Yale University and her MD from Columbia University.
The transcript below has been edited for length and clarity. Listen to the audio of the interview here.
Brooke Siem: We had a couple of minutes before recording and you asked how I was doing. I said, “On paper everything’s great, but I’m struggling with this existential feeling of being 38, single, childless, increasingly aware of mortality.” You mention early in your book The Anatomy of Anxiety, that there’s true anxiety and false anxiety, and that true anxiety pushes us to face these big questions. Can you talk more about that concept and how it fits into your work?
Ellen Vora: True anxiety exists so naturally in juxtaposition to false anxiety. Sometimes, we think we’re experiencing deep mental health issues when we’re actually dealing with inflammation, chronic sleep deprivation, or blood sugar fluctuations. That’s false anxiety. But true anxiety, or what I call purposeful anxiety, isn’t something wrong with us—it’s what’s right. It’s when we can deeply connect to what’s wrong in our lives or the world. This isn’t an anxiety to pathologize or suppress, nor is it something we can avoid by just eating gluten-free food or avoiding caffeine. It’s our inner compass, urging us to slow down and pay attention.
When it comes to the big existential issues like this massive vulnerability of going through life in a human body, where we acknowledge that we will die one day, where we will lose the people that we love, or where there’s suffering, we’re not wrong to have true anxiety. There’s a lot to grapple with here. But I believe there are tools to approach these questions with grace, and I touch on this in The Anatomy of Anxiety. My second book, Season of the Witch, explores this even further, pushing the boundaries of how we can meet and approach death differently, find meaning, make peace with life’s unpredictability, and live fulfilled lives. I discourage coddling ourselves with platitudes like “You’ll be fine,” or “Rejection is protection.” Although these phrases are well-intended, they don’t allow us to fully confront true anxiety. Rather than reassuring ourselves that everything will be okay or resigning to the idea that life is just painful, we need to acknowledge and feel what this anxiety is telling us.
Siem: How do you know the difference between true anxiety and false anxiety?
Vora: When I work with patients, I start by addressing false anxiety, because most people have difficulty discerning the two. False anxiety is often the “low-hanging fruit.” It’s quick wins that are in the way. If we’re experiencing a lot of false anxiety, our moods are this pinball game. We’re bouncing all around and it’s very difficult to hear the real clarion call of our true anxiety because we’ll mistake a lot of things for true anxiety when, in fact, it’s our blood sugar. I first help patients address the false anxiety and physiological causes of anxiety so they can gain clarity. Once those are under control, they can get still, slow down, and have an inner conversation to uncover the true anxiety at the heart of it all.
Siem: What’s the checklist or algorithm you use for identifying false anxiety?
Vora: False anxiety can be such a triggering term. I’m aware it could be interpreted as invalidating mental health issues, but that’s not my intention. False anxiety is when something triggers our body into a stress response, which we then experience as anxiety, sometimes even panic. We’re taught that mental health issues are due to genetic imbalances or fixed psychological traits, but often it’s just a blood sugar crash or something equally straightforward. This type of anxiety doesn’t stem from a deep truth about us; it’s simply a physiological reaction. That checklist contains everything from blood sugar to chronic sleep deprivation to blue light to mouth breathing to sleep apnea, and so forth.
Our hormones, our gut health, micronutrient deficiencies, the degree to which we have inflammatory molecules coursing through our bloodstream—there’s an enormous influence from food. Most people are eating foods engineered to be hyper-palatable and nutritionally depleted. They’re inflammatory and this is creating a physiologic mess inside of us. Then, there are some more straightforward aspects of false anxiety where we’re dehydrated or mineral-depleted. The list is long, and there are layers to how we address the false anxiety in their body, but it’s usually something to do with diet and lifestyle.
Siem: You mention in your book that mental health issues wouldn’t have skyrocketed if these disorders were primarily genetic, as our genes haven’t evolved that quickly. Evolution takes thousands of years, yet in the past decade, rates of mental illness have spiked. That doesn’t make sense from a genetic standpoint.
Vora: Beautifully said, and we’re going to talk about epigenetics. Let’s also recognize this has been an improvement upon the old model of mental health when we used to see it as a moral infirmity and shame people for it. In some ways, the disease model and the genetic basis came as a breath of fresh air. But society then became fully entrenched in the idea that mental health is a genetic or a chemical imbalance, which worked too well for pharmaceutical marketing.
This genetic model, however, promotes a fixed mindset toward mental health. It implies that mental health issues are part of who you are, something you’re stuck with, but that are treatable with medication. If meds or therapy work, that’s fantastic. But after 11 years in practice, I’ve observed that most people aren’t adequately supported by medication alone, and some are even harmed.
The problem with the genetic model is that if treatments don’t work, people lose hope and feel beyond repair, thinking they’re inherently broken. That’s why I want to cry from the rooftops, “No! No! Do not despair! Do not lose hope. We gave you a very limited menu of strategies, and it turns out there are many paths up that healing mountain.”
I approach mental health with a growth mindset, suggesting that mental health issues are symptoms of some sort of imbalance. Identifying the root cause—whether it’s physical, psychological, or due to unresolved trauma—can lead to healing. Functional medicine sees genetics as loading the gun, with environmental factors pulling the trigger. I say this to empower people and give them hope that there is something we can do about it.
Epigenetics is an important part of this conversation because we’re so plastic. We have so much control over how our genetic predispositions manifest. When we emphasize lifestyle, diet, and addressing trauma, people feel they’re being handed a to-do list. It can feel overwhelming, shaming, or foolish as if they should have known all along that a walk could help. This is why the meme about taking a “stupid walk for my stupid mental health” resonates—it’s easy to feel foolish for not knowing that a simple walk could make a difference.
Siem: I’ve noticed, both in my life and work as a chef for pro athletes, that simple changes—especially in food and environment—can make a huge difference. It’s frustrating that we’re often told mental health is complicated, when really, it’s about making things simpler, not piling on supplements or new products. But society emphasizes complexity.
Vora: The things that truly make a difference are simple, but they’re hard to do. Our world doesn’t make it easy. We need nourishing sleep, sunshine, movement, community, quality food, clean water, and air. These are basics that used to come naturally, like what was available for free back in evolutionary times. Now, you have to intentionally and proactively design your life to reclaim them. There’s no real shortcut.
But when we’re overwhelmed, we crave shortcuts or hacks. We tell ourselves that maybe if we find the right supplement from the upper echelons of “bro wellness,” we can bypass all the effort of lifting heavy things and going to sleep early.
The wellness industry started with people taking health into their own hands after feeling dismissed by doctors. They discovered that food and lifestyle have a huge impact on health. But now, we’ve lost the plot. Wellness has become overwhelming and consumerist, leading people to fear food or socially isolate or follow endless rituals. Instead, what we need to do is identify the non-negotiables that actually work and build them into daily life. Set it and forget it without feeling like a patient and constantly being put into a state of fear.
Siem: From my perspective, it feels like conventional psychiatry is trying to medicate both true and false anxiety. But I’m particularly interested in what happens when true anxiety is medicated. For me, I was grieving, and at 15, I was put on Effexor XR and Wellbutrin XL, which changed how I viewed the world. When I got off these drugs at 30, I went through a severe withdrawal and had to face all the things that were medicated away. It was terrifying, and I had no guidance.
I wish I had known about you back then, as you’re one of the few psychiatrists speaking openly about withdrawal and the emotional responses tied to trauma. Could you talk about the intense anxiety during withdrawal, which can sometimes be even worse than what someone felt before starting medication? What do you think is happening both physiologically and emotionally?
Vora: I was recently in Vienna, and I love to tell myself that all my problems would be solved if I were in Europe where there are fewer pesticides. But I also noticed that, even there, there’s no cure for the human condition. People still have struggles, and that’s part of the problem with conventional psychiatry. We’re going to lose people we love. We’re going to have senseless traumas in our lives, and we’re given no tools to hold space for these experiences without immediately trying to make suffering disappear. We need to be with grief. We need to be with our feelings. We need trauma-focused therapy for trauma.
When you medicate during a major emotional process, you’re not removing the energy of that emotion. There’s conservation of mass. We can blunt our body’s ability to emote it and feel it and access it, but in withdrawal, there’s a recapitulation of that process—a kind of “salt in the wound” when withdrawal is already hard in its own right. So, if you were going through a big life change, like a divorce, and medicated it, then in withdrawal, those feelings often resurface, demanding attention. In many ways, I believe it’s best to feel our feelings, the sooner the better. This brings up a distinction I’d like to discuss later—between psychedelics and antidepressants in terms of how they impact our ability to feel emotions.
As for withdrawal, some people discuss ways to support it physically, but when it comes to holding space for the emotional aspect, I’ve learned a lot from Kelly Brogan, who describes withdrawal as a birthing process or initiation. I remember being in labor, and two things can be true about it: it’s incredibly hard, and you can do it. When I was choosing between an obstetrician and a midwife, I was told that a midwife might sit in the corner knitting during labor. At first, I thought, “Why would that be a good thing?” But I realized that what you don’t want during birth is a fear-based, reactive, intervention-heavy approach. Of course, there’s a time and place for interventions and emergencies, but mostly, labor is a painful yet natural process that you need to move through. The midwife’s presence, calmly knitting and saying, “You’re doing great, mama,” actually strikes the right balance. It’s supportive without panicking, allowing the process to unfold rather than trying to control it.
An early experience with a patient taught me a lot. He started on Prozac during a divorce, not because of depression but due to situational stress. Once things stabilized, he wanted to taper off, and I supported him with what I now see as an overly aggressive taper. He then started experiencing suicidal thoughts—something he’d never faced before. This wasn’t a relapse; he hadn’t been suicidal before. He was experiencing withdrawal. This didn’t go back to some state he was in before. This was a new state he was in. This taught me that we often misinterpret withdrawal symptoms as a relapse, which frustrates me about the psychiatric community’s approach to withdrawal. There’s a culture of blaming patients, assuming symptoms in withdrawal mean they need medication, rather than recognizing these symptoms as part of the withdrawal process.
Siem: How many of your patients experience new psychological discomfort during withdrawal? In the withdrawal community, there’s a narrative that if you taper slowly enough, you can avoid symptoms entirely. I sometimes wonder if these intense emotions have a purpose. Where do you draw the line between useful emotional processing and signs that the taper may be moving too quickly?
Vora: This question is at the outer bounds of my philosophical musings. Some patients are highly motivated to avoid withdrawal symptoms entirely, often due to past experiences with difficult tapers. In those cases, they’re more inclined to “ask for the epidural” by going as slowly as possible. This requires working through the trauma from previous withdrawal attempts. Others are open to allowing some discomfort if it means making steady progress. It’s always a balancing act between making the process bearable and sustainable emotions, but where it’s manageable enough to prevent setbacks.
I don’t necessarily think everything happens for a reason, but I think everything that happens is something we can make meaning from. When my patients have a big emotional process with a taper, it’s often fruitful work for learning about their wants, their desires, their needs, and their fears. It’s part of a self-actualization process so when it comes up, we roll with it. When it’s unbearable, we do everything we can to mitigate it. When it’s not possible to fully mitigate it, we say, okay, there’s something to pay attention to here.
Siem: I find the intersection between trauma and withdrawal fascinating. The withdrawal process seems to bring past experiences to the surface, sometimes magnifying them. For instance, feelings from childhood or past traumas can resurface unexpectedly. How do you help patients manage these trauma responses when they’re going through withdrawal?
Vora: I think there’s a profound similarity between trauma and the experience of withdrawal. During withdrawal, you might feel victimized by the prescriber who put you on the medication, the one who took you off too quickly, or an unsupportive industry that closed its doors when you needed help. There’s a feeling of powerlessness and fear, of not having the ability to find safety, which can vividly recall past trauma.
When trauma happens in childhood, the system can be overwhelmed by a stressor it isn’t equipped to process or handle. Without language, support, or a safe space to make sense of it, that energy becomes trapped—stored in the brain, tissues, and fascia—manifesting as symptoms. We weren’t ready then to understand it on a conscious level.
Withdrawal in adulthood can bring those old feelings back, but now from a place of an adult mind. This creates an opportunity to work through them constructively. We can acknowledge feeling powerless, victimized, or unsafe, and ask, “How can we secure you in some way?” By re-parenting ourselves, showing up with support and safety, and building the right framework around us, we can make withdrawal reparative, allowing the healing of past wounds. But that’s only if the right support is in place; otherwise, it risks becoming a damaging repetition of the original trauma.
Siem: Withdrawal has felt like time travel to me. I lost my dad suddenly when I was 15, and withdrawal made me feel as if I was re-experiencing the shock and loss of that event. I hadn’t processed those feelings fully back then, but during withdrawal, they resurfaced. It’s as if there’s a recognition of past pain that was on hold, and the experience of withdrawal brings it up in a visceral way.
Vora: The brain is our lens on the world, and when it’s going through the turmoil of withdrawal, it can make you question what’s real or true. But withdrawal is absolutely real. Once, I spoke to a functional medicine practitioner about supporting withdrawal from psych meds, and she told me her patients didn’t experience withdrawal. I remember wondering, Am I the problem? Am I a bad doctor? But I realized we often don’t ask the right questions to truly understand patients’ experiences, so we miss the reality of what they’re going through.
Withdrawal is real, and I think we need to lean on others for validation because the industry often gaslights us into doubting its existence. When withdrawal disrupts the brain’s neurochemistry, it does bring the body back to the trauma. Those without a history of trauma may sometimes have an easier time, but for others, withdrawal triggers a bodily memory: I know this feeling, and this isn’t okay. It activates survival responses as if the body recalls the original threat.
I’ll always say this: we need more space for grief. After my mom passed, I was in Brazil working with ayahuasca and experienced a profound ceremony that felt like a funeral for her. I thought “This is how a funeral should be”. It’s about witnessing the loss, crying deeply, and truly feeling the magnitude of it. Here in the U.S., we don’t have systems in place for genuine grieving. We’re an emotion-phobic culture, surrounded by people who become uncomfortable when we cry. We apologize, try to contain our tears, as if holding back a sneeze. But we need to allow for big, messy, raw cries in the presence of people who can hold that space. We need to be able to drop to our knees and let waves of grief wash over us—even when it’s inconvenient.
Grief, to me, isn’t negative. I’ve gone through two significant losses, more if you include pregnancy loss. Yes, I’m sad about losing loved ones, and I reflect on the complexities, the things I wish I’d done differently. But grief is also an exquisite form of love—a minor melody, but the same song. My sister helped me understand this during my pregnancy, after my mom’s passing, when I worried about grieving while carrying a child. She told me that the placenta filters the grief, and only love reaches the baby. Every time I had a primal cry during pregnancy, I carried that image, feeling that I was bathing my baby in love.
I think we need more space for this reframing of grief, seeing it not as a burden but as a shared human experience. We each carry unprocessed grief, and by grieving around each other, we give each other permission to do the same.
Siem: Grief doesn’t just come from losing a person; it can arise from lost relationships, jobs, or other attachments. When people feel intense emotions over these losses, they may think they’re mentally ill rather than simply grieving.
Vora: Unrealized dreams, pregnancy loss, not having the children you want, or even the children you do have—these are all valid forms of loss. We need to acknowledge all kinds of grief, big or small, without ranking or invalidating them. There’s no “oppression Olympics” when it comes to grief; whatever resonates for you in that moment, let yourself feel it.
We have a tendency to pathologize these natural responses, but as I often say, there’s no cure for the human condition. Losses are part of life, and none are more or less valid than others. We simply need to give ourselves permission to feel them fully and be present with them.
Siem: One of my favorite quotes from Joanna Cacciatore, a grief researcher, is, “Grief waits for you until you’re ready to do the work.” It’s incredibly true; you can medicate for a while, but eventually, these emotions come back up. I’m grateful you’re talking about this, and I know it’s a theme in your new book.
Vora: Yes, my new book starts with my experience of grief, which then opened up a larger exploration of spirituality. It’s a complex topic, especially for a physician, but I lost my atheism after my mom’s death. I now see the world as more than just random, material occurrences, which has been deeply healing for me. The book doesn’t prescribe a singular spiritual path; it encourages readers to seek what feels true and resonant.
Siem: I’ve noticed shifts in how we talk about these topics, especially in recent years. To close, has anything shifted in your perspective since writing the book?
Vora: Great question. If anything, I’ve become more aware of the nuances in how we talk about mental health. I’m steadfast in my belief that nutrition impacts mental health, but a friend recently suggested my approach could be “giving diet culture.” I now consider how to balance dietary recommendations with the awareness that we exist between the extremes of toxic diet culture and, sometimes, an overcorrection of body positivity. We need nourishment without fear, shame, or fragility.
I also want to thank you, Brooke, I’m in so much gratitude to you for the role you play in discussing medication withdrawal and the pharmaceutical industry. It’s still a vastly under-discussed topic, and I’m grateful for the space to share my thoughts on it.
Siem: Thank you! Your insights have had a big impact on me, and I’ve learned so much from you. I can’t wait to read your next book.
***
MIA Reports are supported by a grant from Open Excellence, and by donations from MIA readers. To donate, visit: https://www.madinamerica.com/















I strongly urge MIA to NOT publish or keep this interview online, as it poses significant harm to individuals dealing with mental health conditions.
To suggest that a “certified board psychiatrist” (whatever that means) can label bodily sensations such as inflammation, sleep deprivation, and blood sugar imbalances as “false anxiety” is both misleading and detrimental to public health.
Mental illness often involves a disconnection from the body’s communication and an inability to process social or environmental pain—what this individual refers to as “true anxiety “in the latter. But, to dismiss bodily distress as “false anxiety” minimizes the profound impact that physical health has on mental well-being.
“I first help patients address the false anxiety and physiological causes of anxiety so they can gain clarity. Once those are under control, they can get still, slow down, and have an inner conversation to uncover the true anxiety at the heart of it all.” Language is extremely important so to minimize the body over something socially like relational aspect by a doctor is misleading I hope I am very wrong in this take!
But, I think this is not a matter of misinterpretation; the perspective presented here is fundamentally flawed and actually harmful to unsuspecting people who read your site thinking you are on their side.
Either please remove the interview entirely or revise it to reflect a more nuanced and responsible understanding of mental health, even if it contradicts the interviewee’s claims. It is crucial to approach such topics with care and consideration for the individuals who are most affected.
This type of discourse proves beyond any reasonable doubt that psychiatry is not medical or a doctor! What doctor says your body communication is “false anxiety”. Doctors use words literally not symbolically and if she is using these words symbolically than she is not a doctor!
If you do not agree with my comment in principle then please do not moderate my comment so it stands to warn people that their “false anxiety” is not false at all.
Ps. I tried to use Chatgpt to be cordial and reasonable in my comment but it told me my response was more emotional than “factual” so I decided not to use it! I am keeping it emotional response because I value emotional response just as much as “factual” response.
Thank you,
Report comment
Nothing wrong with an emotional response in my mind. Besides, you’ve got plenty of factual backup for your points!
Report comment
Thanks Steve for your kind words. The AI did not approve my take on “psychiatry”.
Report comment
Quite literally, in the interview, she addresses your concern. I suggest re-reading this when you are less upset, or actually read her book. The whole point is that bodily distress directly contributes to mental health.
“False anxiety can be such a triggering term. I’m aware it could be interpreted as invalidating mental health issues, but that’s not my intention. False anxiety is when something triggers our body into a stress response, which we then experience as anxiety, sometimes even panic. We’re taught that mental health issues are due to genetic imbalances or fixed psychological traits, but often it’s just a blood sugar crash or something equally straightforward. This type of anxiety doesn’t stem from a deep truth about us; it’s simply a physiological reaction. That checklist contains everything from blood sugar to chronic sleep deprivation to blue light to mouth breathing to sleep apnea, and so forth.”
Report comment
Beautiful interview, just beautiful. Almost like reading a poem or singing a prayer.
Report comment
agree Birdsong very lovely. I just read the Guardian interview from 2022 when the book came out.interesting commentary about anxiety and some people being very empathic in a world full of pain and trauma and fear
Calling it false anxiety is unfortunate tho as it implies you are making it up but she is advising to first fix up the habits that contribute: poor sleep,crap food, caffeine, drugs that cause anxiety,endless scrolling, no vitamin D etc which is all valid. I can actively increase my anxiety by doing all those things.
Report comment
So happy you feel the same, K! 🙂
I’m not crazy about the term “false anxiety” for the same reason, but I didn’t want to make an issue out of it because like you said, she addresses the things that could be aggravating an inflammatory response.
Thank you for mentioning the Guardian interview. I look forward to reading that, too!
Report comment
“Psycho-Oncology: How Unresolved Emotional Trauma Can Cancer”, Nickerson Institute of Integrative Health Training, published by the Canadian Holistic Nurses Association
Report comment
I think in the long run we are better served by more perspectives rather than censorship, no?
Report comment
I thank Dr. Vora for this straightforward description of the functional-holistic paradigm of well -being. Thousands of school children would be spared risky referrals to pill-pushers if their basic health needs were understood and satisfied in natural ways. Our society needs to make the knowledge, skills, and means for health available to all. Functional-Holistic care will help people to feel and behave better and to cause less harm to themselves and others. Misfortune and bad actors will still cause trauma, and we will still need institutions to protect the innocent ; along with doctors, therapists, coaches, friends, volunteers.
Nutritionist Doctor Julia Rucklidge has described how the knowledge of nutrition has been discovered and lost multiple times throughout history. We need to keep the expanding knowledge of nutrition front and center. Following is a link to MIA articles by Dr. Rucklidge:
Nutrition and Mental Health: An Interview with Julia Rucklidge, Ph.D.
Mad In America › 2021/04 › nutrition-mental-health-interview…
Thumbnail image
Apr 17, 2021 … Nutrition and Mental Health: An Interview with Julia Rucklidge, Ph.D. … This episode of “Mad in the Family” discusses the links between …
Report comment
As a psychotherapist (I know…I’ll get labeled as “evil” on this site), I often start with the low-hanging fruit with children and adults and check if they are sleeping regular hours, eating healthy unprocessed foods, getting enough exercise, getting enough stillness/meditation. And all of these are often rare. Usually they are on psychiatric rx and also alcohol, THC, caffeine, etc. No wonder they have “anxiety” — their bodies are processing garbage and telling them that fact. “False anxiety” is an unfortunate label and she should stop using that term IMHO. But her description and intention both seem clear and useful.
Report comment
Makes sense to me!
Report comment
RE: I understand that a patient might become upset if a new doctor challenges a diagnosis which they have embraced. Sometimes doctors over-simplify explanations and that can feel demeaning of one’s intelligence. Yet, other patients may not mind the “handy” improvised label; we are all so different. In any case, Differential Diagnosis is critically important, given that the same symptoms have many possible causes. I understand that Functional-Holistic medicine invests more in the Differential Diagnostics which when properly done would reduce the rush to treat the patient with the wrong meds. BTW: An allopathic doctor, who did not use the Functional-Holistic approach to explore the context of a patient’s complaints, told me that the symptoms of anxiety and depression often overlap. I have witnessed a cavalier approach in the prescribing of medication to become a quick turn in the wrong direction.
BTW: Breaking news today is that an asthma medication has been linked to suicidal thoughts. Wouldn’t this include anxiety? Wouldn’t we want the adverse effects to be identified and the offending drug to be withdrawn? Here’s the link to breaking news: https://www.democratandchronicle.com/story/news/health/2024/11/24/singulair-asthma-study-mental-health-fda/76549193007/
Report comment
“We are the medicine for each other.” ~ Teal Swan
URGENT: TURNING POINT for Humanity! Teal’s MIND-BLOWING Truth About Humanity’s FUTURE SURVIVAL! @InspiredEvolution
Report comment