Of course, anyone can get healthier and more resilient, and I can too — despite the diagnosis of schizophrenia. It bothers me when certain experts say that schizophrenia is genetically determined and incurable, and can only be treated with a lot of antipsychotics and other psychiatric medications — for the rest of one’s life. There I protest. Because my own experiences have shown that specific exercises can help me to recognize the early symptoms of psychosis even earlier and more subtly, and reduce their intensity — even the delusions! This is my personal story of recovery, which I have been actively pursuing since the onset of my first psychotic episode in the summer of 2010.

My goal is to become permanently self-determined and free from psychiatric medications. For over three years I have been taking the dose that I have individually determined to be the lowest possible for me, namely 1 mg aripiprazole daily, and I am steadily getting livelier and more stable.
I use my increased time as a healthy person for campaigning for more inclusion, diversity, equality, and human rights. In 2022 I was the overall coordinator of the Mental Health Awareness Week, a joint project of the Max Planck Gesellschaft (MPG), a leading German research organization with its 86 Max Planck Institutes, which ran from October 10th, the World Mental Health Day, until October 14th. The online event offered lectures and workshops on a wide range of subjects related to mental health, from prevention to inclusion. With up to 1900 participants and over 60 supporting institutions, both inside and outside the MPG, the week was a great success. I am also Works Council chair and officer for workplace health at the Max Planck Institute for Medical Research in Heidelberg, and a committee member in Asylarbeitskreis Heidelberg, a non-profit association for refugee support, and I sing in Heidelberger Beschwerdechor, an inclusion choir. In my private life I am a married woman, daughter and sister. My personal return to health has been decisively helped by people around me, to whom I am more grateful than I can say.
In the first six years after my first diagnosis, the realities of my life looked completely different. I was taking 15 mg of aripiprazole daily, which is considered the standard dose for maintenance therapy, and thus 15 times my current lowest possible aripiprazole dose — despite serious (side) effects that included loss of ability to think, feel, and act, and loss of satiety, thus resulting in obesity. At that time the psychiatrists declared that I was healthy — after all, I had no relapses and held a full-time job. They viewed the (side) effects of the medications as symptoms of schizophrenia. I now realize that at that time I was just managing to maintain my independence so as to not appear in society to be problematic, needy, or pitiable. When the medication kept me from recognizing problems, it was really as though I had no problems, and therefore didn’t cause problems. And so I became an unproblematic and invisible being and lived out an existence as a shadow on the borders of society.
Then, in 2016, when I started experimenting systematically on myself to live as far as possible without psychiatric medication, I got no support from my psychiatrist: on the contrary! Even a reduction of aripiprazole to 10 mg daily was viewed with suspicion, and no further reduction was allowed — until I stopped going to her and started to fight on my own to get my life back. My first two attempts at quitting (when I had finally found a psychiatrist and a psychotherapist who treated me as an equal and were open to my experiment) landed me in the clinic in 2018 and 2019. My status as a seriously disabled person was then confirmed for a limited period, which gave me some protection at work and made dismissal slightly less easy. It was only through these experiences with quitting that I realized how free of medication I could become, and how the first psychotic symptoms arose in me.
After my third attempt at quitting, I began to find out where the lowest possible dose of antipsychotics lay: a level where I had as few (side) effects as possible and still remained stable. That was the best thing that could possibly happen, and today I am still learning to register changes in my perceptions, thinking, feeling and acting ever sooner and more subtly. I am learning to distinguish between withdrawal symptoms and my susceptibility to stress and psychosis. I am learning, step by step, to replace the protective effect of antipsychotics with my own resilience and to LIVE — as intensely as possible.
For me, schizophrenia is a problem of how information is wired: too few sources of information in my brain and in the environment are coupled so as to be healthy and life-strengthening. Antipsychotic substances inhibit the linking of information sources, regardless of whether they are healthy or not. Thoughts, feelings and actions simply get buried, along with the individuality of the person who is being treated with excess medication. Today it is incredible to me how far antipsychotics artificially made me unable to judge or act. It was as though I was robbed of my ego and thus dehumanized. And yet my psychiatrists at that time told me I was healthy and the antipsychotics were good for me. Good for me? Or did they mean good for them, because I was compliant and easy to care for?
The great challenge, in my opinion, is that this situation cannot be improved by simply and collectively stopping the use of antipsychotics and psychiatric medications, because less use of medications means that more interventions without them will be needed to treat stress and psychosis. It seems to me that the whole of society in the First World is at its limit right here: where psychiatric medications are endlessly available while alternative therapies are inadequate. When schizophrenia sufferers are treated with (too many) medications and then stop taking them because of the intolerable (side) effects and are left alone, the result can be a severe relapse. They are then often passed on to clinics where they are treated with still more and stronger medications. The vicious circle of excessive medication, stopping and relapsing can cause patients to lose all hope of improvement, and ends up being dangerous or even fatal.
Yet approaches without medication are available, such as Open Dialogue, which is based on reciprocal attention and appreciation on the part of all participants and has proved effective in preventing relapse. It is clear to me that all of society, i.e. not just affected persons but also the relatives, other caring persons and health professionals need to be willing to work actively and systematically on themselves, to listen and talk to each other as far as possible. Without these joint efforts towards a social co-existence with mutual respect, improvements or (partial) cures for so-called schizophrenia and mental disorders in general will, in my view, hardly be possible.
Becoming more resilient means, for me, that I take the fragments of my identity which have become lost in the course of my life so far, and carefully and attentively re-assemble them into an intact ego so that I can perceive myself ever more accurately and clearly. What am I and why? Where is my place in this world? I look back on past times until they feel alive and warm: perhaps only for a moment, perhaps now and then, perhaps even for the rest of my life. I believe that it is helpful — and an essential part of living — to sense these moments and remain in touch with myself.
A simple exercise helps me to be stable with as little medication as possible. 1) I let myself be aware of how I really feel and why, and then 2) I consciously examine whether and how strongly the thoughts, feelings and actions are psychotic. When, for example, I hear a loud bang at home and then for a moment feel fear, I pause for a moment and assess inwardly what has happened: the bang came suddenly, the source was clearly the building site nearby. It is alright that I felt fear for a moment, but now no longer, because there is no danger from the building site. I can now relax, because I am not psychotic.
This means that I make myself consciously aware of what is happening in my head, both the thoughts and the feelings and the context in which they arose. In this way I narrow down the thoughts, feelings and context, which gives me confidence, and I can then let go of what I have realized. A cognitive exercise like this need only take a tiny moment. After years of practice, it happens in me almost automatically, and the repetition of the exercise has clearly shown me that early psychotic symptoms can be accurately reversed. I call the effect of this exercise my redundant mental filter, in contrast to the main mental filter which everyone is equipped with and which automatically sorts and filters information. When my main mental filter registers signs of a disturbance, I sense this with my redundant mental filter and, so to speak, can repair the main filter.
Becoming more resilient means, for me, also having more self-control and self-responsibility. I need to regain the control over and responsibility for my own thoughts, feelings and actions which have run loose, triggered and reinforced by the psychoses. What matters is the breaking out of the cycle of thoughts, feelings and actions around the delusion and other psychotic symptoms, to keep them from becoming chronic and finally to stop them. I believe that people in whom a schizophrenia has been diagnosed are less susceptible to stress and psychoses if their egos are more intact, self-controlled and self-responsible. Such experiences of recovery and resilience are made not only by me but also by my husband. He has likewise had experience of multiple psychoses, but for 13 years he has now been free from psychiatric medication and the psychiatric care system. Here he has successfully followed his own special path, which differs from my own.
Given these accumulating personal observations, I find it hard to understand why, even today, research on schizophrenia focuses so heavily on genetics; why helping affected persons involves antipsychotics above all; and why the knowledge and experience of affected persons are barely recognized. If we have an increased susceptibility to stress and psychoses, then there are always reasons for this, which are as individual as we ourselves are.
For improvements here or a (partial) cure, it is necessary to make care systems accessible and to determine the individual causes, so that we as sufferers can work with psychiatrists, therapists and other professionals in the healthcare system. The goal of every therapy should be that we can make our way in life as independently as possible. I am convinced that people will have fewer mental problems the more they are seen and appreciated as they are and want to be.
Excessive treatment with antipsychotics and psychiatric medication in general can hide the true causes of mental problems and disorders, stand in the way of real healing, and destroy real social interactions. As humans and as inhabitants of the Earth we all depend on each other: physically, intellectually, and emotionally. So all of us need to be willing to learn from and with each other in mutual respect, to live together and establish a resilient community.
Translated from the German by John Wray.















Moyu says, “…(when I had finally found a psychiatrist and psychotherapist who treated me as an equal…”
Being thought of as an equal and treated as an equal is where healing begins in any relationship.
Report comment
Very true! Thank you, Birdsong.
Report comment
Moyu says:
“Becoming more resilient means, for me, that I take the fragments of my identity which have become lost in the course of my life so far, and carefully and attentively re-assemble them into an intact ego so that I can perceive myself ever more accurately and clearly.”
“I look back on past times until they feel alive and warm….I believe that is helpful — and an essential part of living….”
“Given these accumulating personal observations, I find it hard to understand why, even today, research on schizophrenia focuses so heavily on genetics; why helping affected persons involves antipsychotics above all; and why the knowledge and experience of affected persons are barely recognized.”
“If we have an increased susceptibility to stress and psychosis, then there are always reasons for this, which are as individual as we ourselves are.”
“Excessive treatment with antipsychotics and psychiatric medication in general can hide the true causes of mental problems and disorders, stand in the way of real healing, and destroy real social interactions.”
“As humans and as inhabitants of the Earth we all depend on each other: physically, intellectually, and emotionally. So all of us need to be willing to learn from and with each other in mutual respect, to live together and establish a resilient community.”
Thank you for sharing your remarkable story and insights, Moyu. It’s a beautiful testament to the resilience of the human spirit. I hope it inspires real change in the mental health system and the world at large.
Report comment
Dear Moyu,
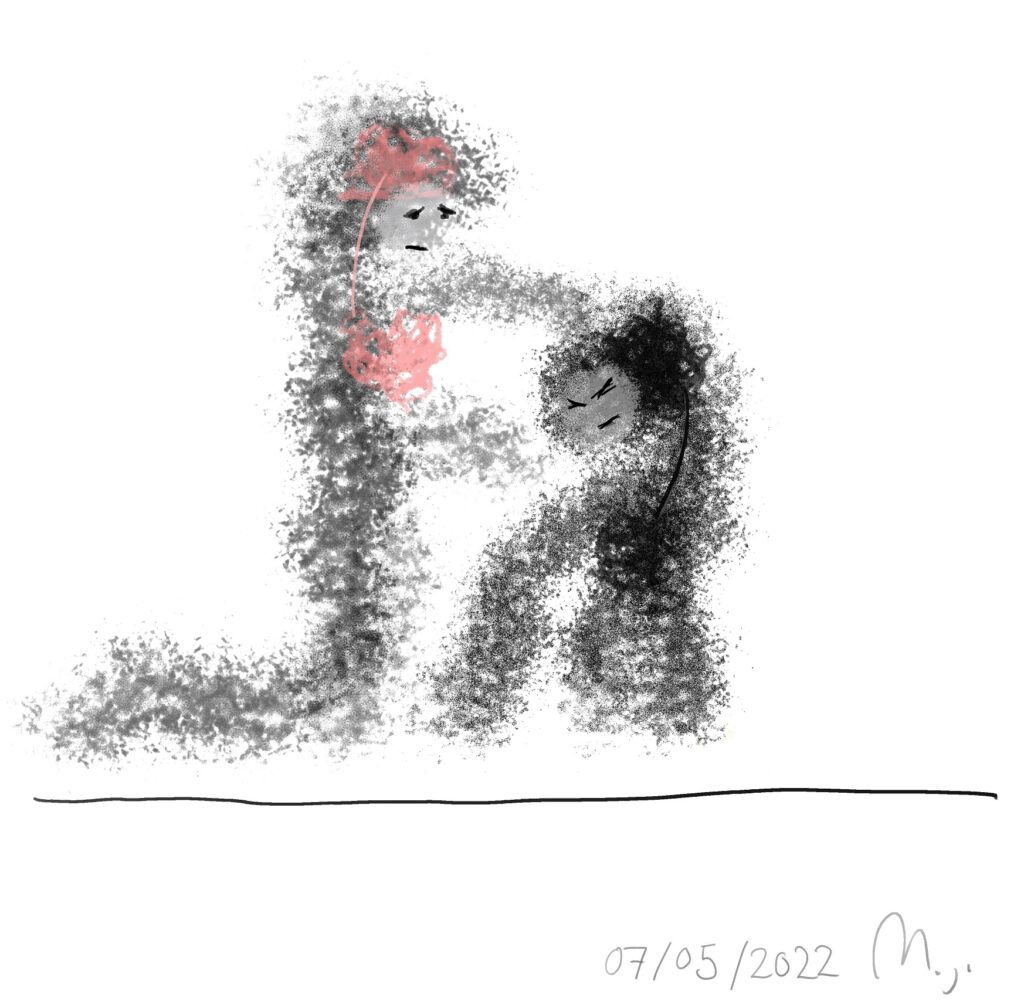
Your art is amazing, just like you.
Report comment
Dear Birdsong, thank you very much! I am honored by all the attention and appreciation you give me 🙂
Report comment
The honor and pleasure is mine, Moyu. The world needs more people like you
Report comment
“It is clear to me that all of society, i.e. not just affected persons but also the relatives, other caring persons and psychiatrists need to be willing to work actively and systematically on themselves, to listen and talk to each other as far as possible. Without these joint efforts towards a social co-existence with mutual respect, improvements or (partial) cures for so-called schizophrenia and mental disorders in general will, in my view, hardly be possible.”
Hello Moyu,
I always appreciate these kinds of articles that bring in the absolute essential role family can play in the healing journey if they are willing to listen and engage their loved one how s/he needs it. I always refer to the journey my wife and i are on as ‘our healing journey’ even though she has d.i.d….I had to be willing to do a lot of changing and learning from her so I could become the healing companion she needed…and 15 years later…we are mostly thru her trauma and dissociation…which is what i feel causes the symptoms that many refer to as psychosis, at least for my wife.
It’s not an easy process, but i believe our reliance on attachment concepts have allowed us to see foundational healing for her without the drugs…and transformative change in myself as well.
If you’d ever like to connect, i always relish the chance to share the wonderful things we discovered along the way and even wrote a little book about some of the highlights of it.
Take care,
Sam
Report comment
Hi Sam, thank you for your hopeful words. It sounds to me very much like you have been through a lot together over the last 15 years. “Our healing journey”, that is a very good expression. Maybe healing never comes alone… Yes, please let me know what the title of your book is.
Report comment
It’s a free download I have on my blog: https://samruck2.wordpress.com/2022/12/04/healing-companions/
Wishing you and your husband the best.
Sam
Report comment
Dear Sam,
Thank you so much for sharing your book here. I have read the first few pages and it is overwhelming – most beautiful and painful at the same time.
When I have read it through, perhaps this weekend, I will write back here.
Best wishes,
Moyu
Report comment
Dear Sam,
Thank you once again for sharing your healing story here. I have now finished reading your book, although I certainly could not give it the attention it deserves.
I can only admire your healing journey over the last 15 years. I wonder if I too could ever be as patient and devoted a partner as you were to your wife…!
All the best wishes,
Moyu
Report comment
Sam Ruck, this is nice:
https://www.madinamerica.com/wp-content/uploads/2022/03/ENGAGING-MADNESS.pdf
Only, this quibble: I like to print out hard copies. My aging eyes are still good enough so I can manage without a giant-sized print font. I am unable to change your pdf file so as to adjust the print size and, so, save a part of a tree.
Report comment
In a 2022 (?) post on the Mad in America blog, Sam Ruck supplies this link:
https://www.verywellmind.com/attachment-styles-2795344
I don’t know that anyone other than me has encountered the following issue: wanting “secure attachments” on the one hand, while being challenged by exposure to a spirituality that seeks to eschew attachment.
It is possible, although in not knowing Buddhism well I am far from sure, that their concept of “attachment” is something quite different from what Sam Ruck hearkens to in western psychology. This exploration has helped me some:
https://www.lionsroar.com/how-we-get-hooked-shenpa-and-how-we-get-unhooked/
Report comment
I would agree, attachment in the Buddhist sense is a much more ineffable quality than a sense of “attachment” to one’s caretakers. The latter has less to do with managing one’s desires and expectations and more to do with needing someone to keep us safe and feeling cared for when we are vulnerable and incapable of caring for our own bodies.
Report comment
Hi Hayden Hall,
I’d strongly suggest following the link I gave to Moyu, if you have interest, and downloading Healing Companions, as it combines Engaging Madness and another little booklet I’d written and expands them into a more-flowing narrative style with a lot more personal stories.
if you think you’d really like to read it, but simply can’t see the font, please contact me at my blog email, and I’ll be happy to give you a word document of it, and then you can change it to whatever size works best for you.
As for attachment, Steve is largely correct. However, I would add that attachment theory includes romantic couples and not only those in caretaking roles of basic necessities…and yet, helping my wife feel safe, loved and cared for…were huge parts of helping heal the trauma she suffered as a toddler and the dissociation that developed throughout her life as a result.
Sam
Report comment
What a beautiful and articulate account. It often strikes me how strong, courageous and resilient many survivors are and you are no exception Moyu.
Report comment
Thank you very much Cathy 🙂
Report comment
This is very inspiring, and I had to share this with my mom, who doesn’t really grasp the concept of collective effort with mental health. As I kind of suspected, she wouldn’t get the entire concept of this article. She got this is a person who is very smart, insightful, and extremely motivated to help herself, but is also an exception. But I think she missed the main point, that I understood to be not self-motivation, but more importantly, was being treated respectfully and that EVERYONE (not even with mental health issues) has to work on themselves, and not point fingers at the one who’s “not functioning like everyone else” and not the “fix them” ilk or else a good outcome will very low or nonexistent.
Report comment
Exactly. Thank you, Rachel 🙂
Report comment
Hi Moyu,
Thank you for your story,
It echoes my own in many ways and in particular my numerous failed attempts and finally successful one at quitting anti-psychotic medication. I am now completely medication free (touch wood) but it has been a long and difficult journey. A lot of that journey has in my opinion been made unnecessarily difficult by lack of accurate and honest information. In particular I was told for many years by so called experts that people such as myself with schizophrenia had an incurable brain disease that requires life long medication. Fortunately the situation seems to be slowly changing due to the efforts of people like Robert Whitaker and many others.
I live in Australia where mental health services are pretty basic. There appears to be very little treatment available in the public sector other than diagnosis and medication. The use of legally binding Involuntary Treatment Orders (ITO’s), mainly used to authorize the enforced use of Long Term Injectable(LTI) anti-psychotic medication, has reached almost epidemic proportions here. This makes it even more difficult for anyone who wants to reduce their dependency on anti-psychotic medication, even when the side affects are quite horrendous. If you go to a mental health medical practitioner and ask for help to reduce your medication there is a very good chance that they will have you placed on an ITO on the basis that your intentions pose a risk to the community.
A small group of friends with lived experience of the Australian mental health system have recently started up a peer-to-peer not for profit mental health advocacy group for fellow Australians. We have called ourselves THE PINK PANTHER MOVEMENT and we identify with the global MAD pride movement. We have just set up a website. https://www.pinkpantheractivists.au
I am just working on a front page article for the website which includes information about the challenges of getting off or reducing anti-psychotic medication. I was wondering if you would mind me using a few pieces of your story in my article as a real life example of someone who has achieved it. My own experience and example is incredibly messy and probably a better example of how not to go about doing it (LOL).
If you wish, I could submit the final article to you for your approval prior to publishing it on our web site.
I don’t think I legally have to seek your permission to do this as my understanding is that it would come under the copyright fair use rule but I prefer to ask your permission anyway.
Regards
Tim Wilson
Report comment
Hi Tim,
Thank you very much for your post and the request.
The Pink Panther Movement and your homepage are great! You can certainly refer to the article and my experiences.
I remember that when I had my second relapse in 2019, the doctors in the clinic wanted to give me a Long-acting Injectabel (Abilify Maintena), of course in the so-called antipsychotic dose. They also considered appointing a court-appointed guardian for me.
It makes me angry to think about it.
Because if I had blindly followed the medical advice of the clinic doctors at that time, I would have spoiled my recovery experiences of the last years and I would be back in the state of the “unproblematic and invisible being”.
What is left in this world at all if we can only ever make the problems invisible instead of thinking about them and solving them together? What kind of world do we want to live in?
It is certainly a long road for us as sufferers and other caring people to fight to be treated as equal human beings with ALL who do not believe in a real healing of mental illness.
Let’s not give up!
Best wishes,
Moyu
Report comment