“Something is wrong with American psychiatry.”
With that statement, Helena Hansen, Kevin J. Gutierrez, and Saudi Garcia opened their recent article, Rethinking Psychiatry: Solutions for a Sociogenic Crisis, recently published in the journal Daedalus. Their work highlights the theories of Frantz Fanon, who believed psychiatric disorders had a social etiology (cause) and, therefore, the solutions to psychiatric suffering must be social in nature as well.
Referencing America’s current mental health crises, including the “youth mental health crisis” and the ongoing overdose epidemic, Hansen, Gutierrez, and Garcia critique the mainstream model of psychiatry, especially regarding biogenesis (biological cause) and psychogenesis (psychological cause), stating that the current models are iatrogenic (causing more harm than good).
Instead, like Fanon, they offer an alternative view of causation, called sociogenesis (social cause), which posits that the experience of society is often at the heart of psychological suffering. The team then offers three examples of interventions that are based on this sociogenic theory and how they help to heal wounds that mainstream psychiatry often cannot.
 What is wrong with American Psychiatry?
What is wrong with American Psychiatry?
“Racial inequalities… continue to worsen, with devastating effects on Native American, Black, and Latinx communities, even as white Americans also continue to suffer exponential increases in mental health–related harm and death. Yet U.S. psychiatry has little to offer for these ills,” the authors write.
“On the contrary, U.S. psychiatry is often a source of inequality and iatrogenic harm, operating within a profit-driven health care system that makes mental health care inaccessible and low-quality even for the white middle class, while clinically supporting police surveillance and mass incarceration in low-income Black and Brown neighborhoods.”
Hansen, Gutierrez, and Garcia connect mainstream psychiatry to what they call the “medical-prison-industrial complex.” This system, they argue, is focused solely on income generation and profit, leaving most Americans without decent mental health care, let alone physical health care, and leading to the prison system becoming the largest provider of mental health services in the United States. This issue has been an ongoing source of controversy, especially with prison abolitionists and disability rights activists.
Often, the only responders available for mental health crises are police, and this starts a domino effect where the police, using their institutional processes and training, lead the person in crisis into the prison system, causing a cycle where the person becomes seen as both criminal and mentally ill; someone in need of constant institutionalization.
The research team references the work of Frantz Fanon, whose seminal work Black Skin, White Masks, where he takes on the European-dominated psychiatric system at work in colonized Algeria, stating that the view of Algerians as suffering from mental illness before they received European-style treatment was backward. That Algerians were not “mentally ill” until they started to experience the degradation and oppression of being occupied by a colonizing force. From this observation, Fanon countered the standing ideas of his contemporaries, who focused on biogenesis and psychogenesis, and stated psychiatric illness was created at the social and institutional levels.
“Fanon’s sociogeny posited that the mind, the body, and illness develop in relation to historically produced consciousness and social contexts. Among Black people, these contextually shaped bodily schemas (or habitus) derive from enslavement and colonial racial typologies.”
This would help explain why black men are more likely to be diagnosed with schizophrenia (“two to eight times more often”) than white men and more likely to be incarcerated than white men (“five times as likely”). Backing up their points, Hansen, Gutierrez, and Garcia state that “the diagnostic criteria for paranoid schizophrenia historically emerged from stereotypes of Black men as violently paranoid.”
Fanon’s sociogenesis is also at the heart of “standpoint theory.” Theorists, such as Sylvia Winter, “drew on Fanon’s sociogenesis to conclude that ‘what the brain does is itself culturally determined through the mediation of the socialized sense of self.’”
According to this theory, not only does individual experience arise within social structures, but so does scientific knowledge. When this knowledge is created through a monocultural lens (cis-male, white, middle-upper class), it reifies the position of the dominant group. This creates a cycle where the experience of the Other is pathologized, and this pathologizing leads to pathological experiences, leading to psychiatric “disorders,” which reifies the original hypotheses of the monocultural scientific community.
Using sociogenesis and standpoint theory, Hansen, Gutierrez, and Garcia call for “time and space for sociogenic healing… [and] collective projects that nourish all participants and foster mutual aid rather than competition over scarce resources.” They offer three examples of sociogenic treatments existing today.
Harm Reduction
“One of the most significant mutual aid movements of the late twentieth century was harm reduction, which emerged in the 1980s in response to HIV/AIDS among low-income, largely Black and Brown people and people who inject drugs, as well as among men who have sex with men.”
Harm reduction is a movement to bring needed services to people who use drugs (PWUD) whether or not they are willing to abstain permanently, and includes syringe exchanges, STI and other disease testing, drug testing kits (to ensure a person’s drugs aren’t adulterated with Fentanyl or Xylazine), medication-assisted treatment (Methadone, Suboxone, etc.), and even moderation management. This movement is designed to fill in the gaps left by a legal system that has criminalized certain drugs and drug paraphernalia based on socio-cultural and socio-economic factors, such as ethnic ties to certain drugs (Opium, Marijuana) or class-based differences in drug use (Crack vs Powder Cocaine). People who lack access to clean syringes or medication-assisted treatment are often left out of the current addiction treatment and policy system, leading to higher incidences of diseases and other issues, such as accidental overdoses. The ethos of harm reduction “is one of community and mutual support, in which those subject to dehumanizing treatment can find refuge and comfort.”
The research team connects the harm reduction movement to other non-drug related movements that share the idea that instead of “eradicating… psychiatric symptoms,” the underlying social conditions are causing the isolation, difficulty, and suffering of people with diagnoses. One example is the “Hearing Voices Network,” which advocates for people who have auditory hallucinations. The group believes that these voices can be as protective as they can be destructive, and they work to help people better understand themselves rather than pathologize the experience. Another example is the “Mad Pride” movement, which, like disability and neurodiversity advocacy groups, rallies for social changes to accommodate people’s differences rather than seeing differences as needing medical and biological reformation and treatment.
Some groups that the team researched include “Boom! Health” in New York City, one of New York’s oldest harm reduction centers, the Atira Women’s Resource Society in Vancouver, and the nationwide to the U.S. Urban Survivors Union (USU). Boom! offers respite and drop-in services, including naloxone kits, laundry, lounge chairs, a pharmacy for medication-assisted treatment, and support groups, which included topics such as “survival sex, intergenerational trauma, an LGBT group, [and] a women’s only group.”
Atira is “internationally known for its safer drug consumption facility reserved for women,” called SisterSpace. This space offers drug testing kits, clean “works” (paraphernalia such as syringes and “spoons”), and well-lit spaces to ensure that drug use is safer and won’t lead to accidental overdose or death. Being women only also allows for safety from any abusers, of which many women WUD are often victims. The USU became well known during COVID by creating the first virtual safe use spaces, where people isolated because of the pandemic could have video resources to ensure notification of authorities in the case of overdose when they used alone.
All these groups attempt to bridge the gap created by social structures and inequalities without pathologizing their users’ and members’ existence and experience. Instead of focusing on diagnoses, medication, and (sometimes forced) psychotherapy, they are offering sociogenic resources to alleviate sociogenic pain.
Harriet’s Apothecary and Systemic Racism
“Central to the movement over the past decade to counteract the detrimental impact of systemic racism on mental health is the work of the Brooklyn-based collective Harriet’s Apothecary. As several other scholars have noted, Harriet’s Apothecary is an example of healing circles dedicated specifically to the trauma of racial oppression.”
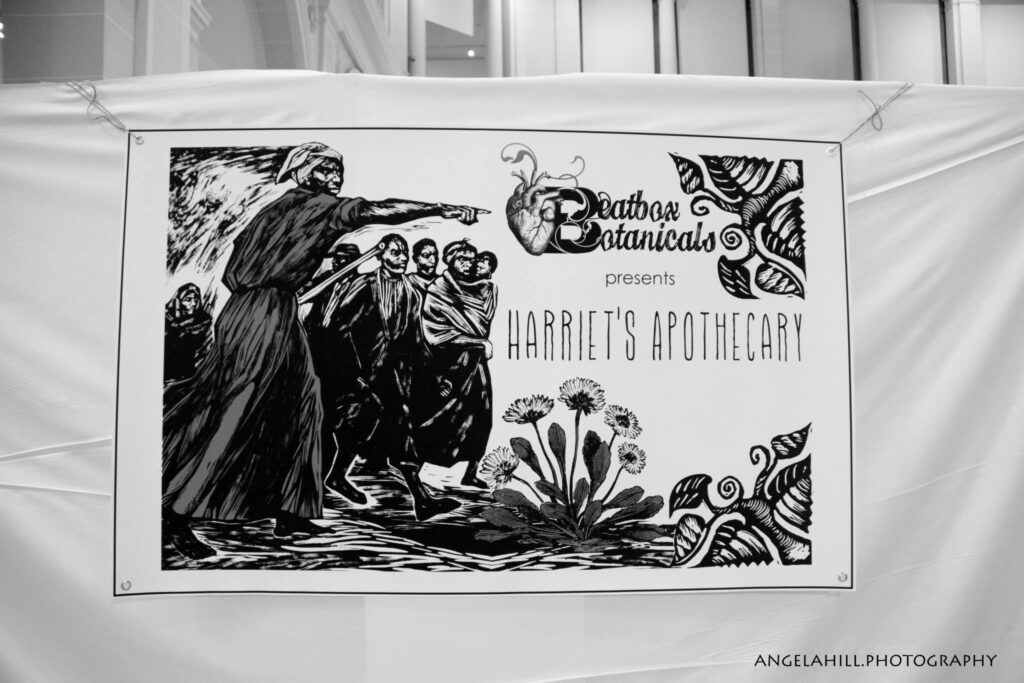 Named after the Underground Railroad’s Conductor, Harriet Tubman, this organization tries to carry on Tubman’s goals of liberation from racism, helping people of color find “power, healing, and safety” while also reflecting on Tubman’s background as a nurse and herbalist, who used “botany, geography, astronomy, herbal medicine, and wildlife biology to help lead enslaved people to freedom.” The Apothecary travels between multiple sites, including “the Black Women’s Blueprint in Crown Heights, a community arts center in East New York, the Brooklyn Museum of Art, and Soul Fire Farm in upstate New York.” Each event is timed with seasonal changes, connecting to forgotten and oppressed religious and cultural practices, which help ground members and users to their own experiences of systemic racism and oppression.
Named after the Underground Railroad’s Conductor, Harriet Tubman, this organization tries to carry on Tubman’s goals of liberation from racism, helping people of color find “power, healing, and safety” while also reflecting on Tubman’s background as a nurse and herbalist, who used “botany, geography, astronomy, herbal medicine, and wildlife biology to help lead enslaved people to freedom.” The Apothecary travels between multiple sites, including “the Black Women’s Blueprint in Crown Heights, a community arts center in East New York, the Brooklyn Museum of Art, and Soul Fire Farm in upstate New York.” Each event is timed with seasonal changes, connecting to forgotten and oppressed religious and cultural practices, which help ground members and users to their own experiences of systemic racism and oppression.
The group speaks about health, including mental health, through ancient and current holistic models and energy-based therapies and helps connect local healers to the apothecary’s attendees on a sliding scale. These healers include art therapists, massage therapists, Reiki, nutritionists, acupuncturists, yogists, peer-support groups, and healing justice workshops. From a sociogenic perspective, this is a vital resource as it “provides a space for Black people to reconnect with the shreds of the land-based identities and practices that their ancestors, many of whom had lived off the land for generations, had left them.” These connections help create multiple and varying narratives, outside of contemporary and mainstream theories, around colonialism, oppression, slavery, generational trauma, and economic injustices.
The Apothecary connects powerfully with existing Blac feminist movements and organizations, especially land-based healing groups, including “the Audre Lorde Project; Soul Fire Farm, the most prominent Black farming hub in the Northeastern United States and a founding member of the Northeastern Farmers of Color Network; Southerners on New Ground; and the Detroit-based Allied Media Conference and Emergent Strategies Immersion Institute.”
By grounding psychiatric disorders and diagnoses literally in the ground and with the land, discussions, and understanding of the social and institutional violence that was perpetrated for centuries, including contemporary events such as George Floyd, affect their user’s individual experience of the world and themselves. This changes the narrative from internal to external brokenness and offers opportunities to heal at the social level.
New Haven Farms and Community Gardening
“Over the past decade, public health discourse in the United States has focused on food deserts and the aggressive marketing of cheap, nutrient-poor, and calorie-dense processed and fast foods in low-income communities of color as an explanation for their disproportionate diabetes and cardiovascular disease…. Many U.S. cities and towns have launched local urban farming and community garden initiatives that produce food and increase social connectedness.”
 In New Haven, CT, you will find New Haven Farms. This urban farming program works with Medicaid programs in Connecticut to serve low-income, often Latinx neighborhoods with healthy food options not often found in those communities. These programs were so good for the participants’ health that “health center providers began writing prescriptions for farm participation to patients at risk for diabetes and other chronic conditions.” Research showed that participants’ A1c level, a blood measurement used to detect and diagnose diabetes, lowered and became healthier due to the better food.
In New Haven, CT, you will find New Haven Farms. This urban farming program works with Medicaid programs in Connecticut to serve low-income, often Latinx neighborhoods with healthy food options not often found in those communities. These programs were so good for the participants’ health that “health center providers began writing prescriptions for farm participation to patients at risk for diabetes and other chronic conditions.” Research showed that participants’ A1c level, a blood measurement used to detect and diagnose diabetes, lowered and became healthier due to the better food.
As for psychiatry, it would assist and offer support as wanted while running available support groups. Still, in terms of medicine, a local farmer went through all the plants being farmed at the location and identified all the medicinal and nutrient properties being grown. This allowed participants to use food medicine before pharmaceutical interventions or even as an alternative to pharmaceutical interventions.
“Horticulture therapy” has been practiced by Helena Hansen at other sites, including the Sobriety Garden at Bellevue Hospital in New York State. It has “operated for twenty-five years on a half-acre plot bordering the hospital and Franklin Delano Roosevelt Highway… [as] both a site for horticultural therapy and community-building for a socially disconnected patient population, often referred from the city’s homeless shelter system or mandated to the clinic by drug courts.” This form of therapy was often helpful for patients with significant trauma histories who were uncomfortable in traditional settings. People would also return to the garden to stave off emotional crises and addiction relapses.
Food and gardening itself can serve as an alternative psychiatric practice. “Annatina Miescher explained that she practiced psychiatry as ‘art with found objects: our job is to help people take the shards of their difficult lives and put them back together in new and beautiful ways.’” In addition to the physical alleviation, practicing gardening can help “remediate root causes of sociogenic mental health problems.”
This all begs the question, “Where does the psychiatrist who practices biomedicine fit into this sociogenic model?”
Hansen, Gutierrez, and Garcia identify multiple ways where psychiatrists can become involved and have been involved in these alternative, sociogenic treatment models. First, psychiatrists can work alongside (instead of over) these groups, offering support for acute needs and medical assistance for those who want it. But they can also create shifts in understanding medicine by prescribing food and gardening as medicine and therapy.
Second, psychiatric researchers can show how these tools and approaches actually work at the biological level, shifting the discourse from an in-out (a person’s internal psyche/brain is broken, causing maladaptive emotions and behaviors) to an out-in model (the social and institutional constructs are affecting the person even at the biological level). This research can “foreground the biosocial turn in the life sciences… to explain how social environments influence brain development and function.” These changes include epigenetics, gut-brain connections at the microbiome level, and the contemporary understanding of neuroplasticity, as opposed to the past view of a static brain.
Third, these changes can help save the profession itself.
“The leading reasons offered for burnout involved providers’ inability to address the social and systemic drivers of their patients’ health outcomes. For psychiatry to survive as a profession, to attract and retain practitioners, psychiatrists must be enabled to intervene on social and systemic drivers of their patients’ health.”
For this change to take place, practitioners must advocate and act for change to the current model, elevating the status of these approaches to mainstream techniques. In addition, Hansen, Gutierrez, and Garcia point out that an uncomfortable conversation around power must occur. This means that biomedical practitioners can no longer be the top authority on these issues, and that would mean that therapists, alternative practitioners, and even the patients themselves exist at the same level as the psychiatrist. This also means that psychiatric providers need to be recruited and even trained within the communities they are from and will serve.
“Psychiatrists must organize this change, in recognition of Rudolph Virchow’s famous observation in 1848 that ‘Medicine is a social science, and politics nothing but medicine at a larger scale,’ with the addition that medicine is also politics, on a community-partner and clinician-training scale.”
****
Hansen, H., Gutierrez, K. J., & Garcia, S. (2023). Rethinking Psychiatry: Solutions for a Sociogenic Crisis. Dædalus, 152(4), 75-91. (Link)















I would like to express my thoughts on the matter with utmost respect to the authors involved. It appears to me that the content may have been crafted with the intention of securing publication, incorporating elements of social awareness, particularly centered around issues of race and indigenous perspectives. My inference stems from the strategic inclusion of terms such as “prison complex” and “police,” which are known to evoke strong reactions.
It is noteworthy to point out that a significant proportion of mental health concerns are prevalent among those who have the means to access psychotherapy and psychiatry services. A cursory examination of platforms like Psychology Today reveals a discernible absence of mental health professionals catering to individuals from socioeconomically disadvantaged backgrounds who find themselves entangled in the criminal justice system.
IMHO, the deployment of these terms seems to align with a trend wherein professionals may use provocative language to appeal to mainstream media for publication purposes. Frantz Fanon’s perspective sheds light on a pertinent aspect not found in this discourse. He, as a black psychiatrist trained in the Western context (France), posits that the European mindset, founded on notions of superiority, not only influenced their colonization efforts successfully (changing language and the laws of many colonized places) but also had lasting implications for boomerang effects on its owners.
Fanon’s assertion implies that the European belief in their inherent superiority led to a self-fulfilling prophecy or cannibalizing itself, where the act of marginalizing others resulted in internal strife and harm. This delusional sense of superiority, according to Fanon, has led to the unintended consequence of psychiatry, initially conceived as a tool for influencing “others”, now turning inward and influencing those within the same societal framework.
It is my belief that associating mental illness or health with socioeconomic factors is a misleading and often seems pandering. While it is true that individuals ensnared in poverty may face challenges in accessing mental health resources, it is essential to broaden the conversation. To be equitable, let us consider those with the financial means who find themselves entangled in the existing system. This perspective is crucial as it highlights the need for change even within the framework of capitalism, emphasizing that transformative shifts occur when the system begins to impact individuals who traditionally possess the means to navigate it and benefit from it.
Report comment
Those that have the financial means, who “find themselves entangled in the existing system,” want NOTHING to do with the existing system … aside from the fact we’re speaking out against it.
Report comment
While I find your language a bit convoluted, I agree with your point.
Fact is, Franz Fanon is considered a hero by Marxists and Critical Theorists. And those buzzwords you mentioned, as well as others used in the article, are all very involved in the field of “liberation studies,” as it used to be called.
I consider this to be a fad, and a dangerous one. It points strenuously at a problem that is quite real and argues for a solution that is quite unreal. The result has been a lot of confusion, if not actual violence (terrorist acts) with no worthwhile result.
The key problem is that it urges, essentially, a rage against the machine, rather than a workmanlike and sensible dismantling of the machine. This gives the machine more power than it deserves. I believe it can be sensibly dismantled without causing a third world war.
Report comment
100% agree with this. It destroyed 10 years of my life and only after stopping all mood stabilizers and anti depressants my life could
Take off. Medicines cause more problem than fixing it. Leave alone the fatal side effects, it overcharges your brain and destroys your common sense and natural healing.
Psychiatrist will never teach you how to cope with your feelings and correct the behavior. They will not stop any medication and will never motivate you to be self sufficient. They make you drug addict.
Report comment
I couldn’t agree more with Dh. Psychiatry is all about the monetary profits. The leaders of the Amer Psych Ass’n COULD have chosen a restorative approach in psychiatry but instead have chosen to make as much profit as possible. Their vehicle for this is the drugs and talk therapy approach. It’s designed to cure no one. In fact, it has a recovery rate of .0005% according to King County (Seattle area) in their 2002 and 2003 Annual Reports of King County Ordinance #13974. The problem is not that mental illness is incurable: the problem is that psych drugs don’t work because, again, they aren’t designed to cure anyone. One restorative approach I used for my loved ones was “Orthomolecular” medicine. Please see my 3 videos on YT at “Linda Van Zandt’s Mental Health Recovery Channel” for more info.
Report comment
There are some good psychiatrists, though what many activists want is for them to simply stop doing harm. Every psychiatrist silent on issues like civil commitment and forced drugging is complicit. Worse, many advocate to expand the practice.
Victims shouldn’t have to beg for mercy from the system that’s supposed to help them. I only learned after many years of psychiatric abuse that some people *actually* thought it helped and were not trying to be punitive. To me, and many others, it was so obviously punitive.
“Mental illness” is the dark valley in which harm becomes help, slavery becomes care, and the revocation of rights becomes justified. It must, as a concept, be radically reformed or outright abolished.
Report comment
I see no good in defending any group that collectively views psychologically distressed people as A) a source of scientific curiosity, or B) a source of professional advancement, or C) their personal pot of gold.
Report comment
Same! I remember seeing a psychiatrist talking about how much they liked the “ethical dilemma” of deciding to commit people to conservatorships. Like, those are people’s lives they’re playing with! It’s not some fun thought experiment. It’s making a decision about someone’s fundamental human rights that can affect them for years if not life. I hate how objectifying the whole profession is. Every person is a test subject to be analyzed and torn apart, not respected and believed.
Report comment
It’s dehumanizing the way psychiatry cruelly dissects people psychologically and then neurologically mummifies them with psychoactive substances. And you’d have to be someone who gets off on power to like toying with people’s future the way psychiatry is allowed to do.
Report comment
There is a corresponding viewpoint getting more attention in mainstream psychiatry called the Social Determinants of Mental Health (SDoMH), a subcategory of Social Determinants of Health in general medicine. This article even takes the premise further. I would agree with the prominent role of capitalism with setting up systems of psychiatric care where the first priority is profit (managed care). What I also applaud is attempt to bridge some of the wide gap between MadInAmerica and the psychiatry that is subject to this system, but that still wants to help people. We potentially can do more together.
Report comment
“We can do so much more together.”
Really? Well, let me tell you something: I don’t need any more “help” from the very same group that saw me as “ill” and prescribed “medications” that were not only unnecessary but caused worse problems. And mouthing terms like “Social Detriments of Mental Health” won’t change a profession based on misinformation and exploitation.
Report comment
Hear hear!
Report comment
🙂
Report comment
Psychiatry is not subject to this system. Psychiatry benefits from this system. Psychiatrists have enormous power, individually and collectively.
Report comment
I can’t stand it when bullies play the victim.
Report comment
I see, in fact, psychiatry as the planet’s biggest mental health problem.
Report comment
It’s one big head fake disguised as medicine.
Report comment
The answer to psychological distress is not “out there” it is within the psyche of every human being, it is caused by our innocent misunderstanding and use of thought. We feel our thinking and when it’s dark and stressful, we feel down, depressed, and anxious. When our thing is light, and relaxed, we feel happiness, joy, and compassion. One need look no further that within themselves for the ‘cure’ they seek.
Report comment
While that’s an interesting theory, it subtly or not so subtly is victim shaming. Much of the mental distress I’ve witnessed is due to trauma. In my case I was sold into trafficking and developed depression, PTSD and an eating disorder. I am in recovery now, but it was not because I had ‘light or relaxed’ thoughts. It’s because I was lucky enough to escape the life through Jesus who brought me people who were able to sit with me as I processed the pain and horror.
Report comment
More individuals need to those of us who have experienced trauma. Glad you found individuals who would walk with you thru the healing process; which must have been painful in many ways. You are courageous to work thru the traumas. I shared a couple of my traumas with a couple members of the Episcopal church family I belong to but the end result was two individuals I shared the traumas with ended up twisting what I told them and they turned some church members against me. No one who has been thru trauma should be re-traumatized thru churches, Social Workers, Psychiatric l, etc. Best wishes to you as you continue your healing path.
Report comment
I’m so sorry this happened, Faith.
Report comment
What?
Report comment
Other interesting approaches to consider that promote a social understanding of “mental illness” and its solutions are Peer Support and Integrative Community Therapy. Thanks for collecting a great list of examples. I found this valuable and inspiring.
Report comment
So… what about the sick people who are well fed, powerful, and can afford all the therapists they could imagine? What do we do about them? Aren’t they the ones causing the anguish that Fanon and others are so concerned about?
Report comment
This is unbelievably irresponsible. Postmodernist claptrap and DEI oversight of medical treatments and care will put tens of millions of people in jeopardy while you are indulging your social experient on people who desperately need mental health care. The author is some adjunct professor at some no name college but unfortunately this article will be cited as solid evidence as justification to toy with the lives and health of the most vulnerable among us.
Report comment
It might be interesting to hear a specific objection you have to a specific claim or study.
Report comment
Possibly Mr. Sloan found the reference to the work of Franz Fanon triggering. It was for me! My objections to the “social justice” approach to mental health are expressed elsewhere.
Report comment
“First, psychiatrists can work alongside (instead of over) these groups, offering support for acute needs and medical assistance for those who want it.”
Did you even read the article?
Also, would you like to cite these studies on people who comply with current psychiatric practice faring better than those who don’t in the long term? Because, there’s tons of data showing otherwise. Disability and suicide rates go up when these meds get introduced and overprescribed. People who stop taking their meds are more likely to be in recovery years down the line. There is also data showing that places and programs minimal medical intervention with strong social support fare much better than our current isolating and drugging system.
If the meds are used, they should be a last resort and mostly in acute crises. The clinical data in support of meds is in the short term, not on the order of many years. Also, a lot of meds that are given should be contraindicated more. For example, young people are given SSRIs for having attempted suicide. SSRIs have been known for decades to exacerbate and even cause suicide risk in young people. These are not the answer.
Meds are not the be all, end all of mental health, and to imply so is very ignorant to the needs and plights of those you claim to care about.
Report comment
We have all witnessed a 40 year long social experiment starting with the rise of the chemical imbalance theory/lie and FDA approval+ mass marketing (including bought off mainstream media) of neurotoxins passed off as “medication”, thanks to a devil’s deal between psychiatry and pharma. The experiment has led to disaster–a holocaust. Traditional psychiatry needs to let go of its hubris and admit to massive failure. Let someone else have a turn.
Report comment
This is rambling and unedited but something the educated community seems to miss.
Epigenetics is a real thing.
In animal behavior we merely refer to it as instinctual behavior.
I have heard Buddhists refer to it as “the karma of past lifetimes”. Whatever we wish to call it, that helps us understand the phenomena, doesn’t matter as long as we recognize its effect.
Human are effected to a lesser degree than animals with more rudimentary brains
Maternal instincts are something we often hear of, and in animal husbandry we often see examples.
One mother will have far more maternal instinct than another.
Another thing readily observable is the different personality/temperament among the offspring which certainly effects the behavior of the individual.
They’re individuals, not merely a bunch of clones.
Some animals, with more primitive brains, such as chickens, exhibit strong instinctual behavior without the benefit of ever having met their mother(epigenetics) while other animals benefit from contact with the mother such as imprinting behavior in dogs.
This is known as the socialization period. (In puppies, the first three months of life).
The young puppy’s ability to cope with future situations will largely be determined by how successfully and thoroughly it is socialized.
I use the examples because they are obvious and readily available to the observer .
To understand humans you have to understand nature.
If you understand nature it helps you understand humans.
Both genetics and environment are at play in our behavior.
In higher forms of life such as humans, epigenetics appears play a lesser role than early childhood development.
It is the mother’s involvement with the child during the imprinting period, what in humans we call early childhood development that will form the child’s perspective for future experiences.
Instinctual behavior exists in humans but to a lesser degree than in lower animals.
In more advanced lifeforms the early childhood development is the most critical factor. A mother should have a selfish interest in her child and focus her love and attention on that child, getting it off to the best start possible. When that doesn’t occur the results are often tragic.
Report comment
Stop worrying about genetics and heed what the Buddhists are trying to tell us.
Past lives are real, as is the loss of past life memory. Operating together, “karmic” relationships are formed that are very difficult for us to unravel unless we unlock a much greater awareness of past lives. Even the Buddhists could not achieve this, yet at least they are aware of it.
Some modern therapies ARE achieving this.
Report comment
Interesting that there is no mention in this article of borderline personality disorder diagnosis — arguably the most criminalized, most “othering” psychiatric diagnosis. In court, for example, it is more often the prosecution rather than the defense that will hire an “expert witness” to diagnose a female defendant with BPD.
Glad to hear New Haven is developing a more progressive approach. New Haven is where I experienced life altering abuse under the name of “psychiatric treatment”. I hear they also have non-police responses to mental health crisis. Not so when I was there. I had police threatening to break down my door, restraining me, mocking me, showing up with the fire department, lights on and sirens blaring, when I was suicidal due to brain damage from ECT, trauma, and undiagnosed akathisia caused by psych drugs.
Report comment
I would posit that BPD is the most “othered”, most criminalizing diagnosis.
“Results suggested BPD patients are viewed by mental health professionals as ineffective, incomprehensible, dangerous, unworthy, immoral, undesirable to be with, and dissimilar to the mental health professionals. Moreover, disgust propensity and the pathogen component of disgust sensitivity were associated with stronger negative attitudes towards BPD patients.”
From Eur Psychiatry. 2022 Jun; 65(Suppl 1): S373. Published online 2022 Sep 1. doi: 10.1192/j.eurpsy.2022.947
PMCID: PMC9567085
Mental health professionals’ attitudes towards patients with borderline personality disorder: The role of disgust
Report comment
It’s good some people are finally seeing psychiatry for the scientistic buffoonery that it is.
Sometimes the only way forward is backwards.
Report comment
The researchers are on the right track, but I consider the following quote disturbingly optimistic:
“Psychiatrists must organize this change, in recognition of Rudolf Virchow’s famous observation in 1848 that ‘Medicine is a social science, and politics nothing but medicine at a larger scale’, with the addition that medicine is also politics, on a community-partner and clinician-training scale.”
Only fools try to change the nature of the beast.
Report comment
Yes, this attitude continues the idea that psychiatry could one day actually know what it is doing and deserve to run life on Earth. This group has never, however, demonstrated any such ability and is unlikely to ever do so.
Report comment
Psychiatry is the profession that “fails up”. The worse their treatment outcomes, the more they’re “needed” (according to the mainstream).
Report comment
I had such high hopes that max in America would FINALLY post a logical and scientific article…I was supremely disappointed. More nonsense, non scientific, cherry picked garbage to throw the baby out with the bath water and 10x any harm created by the system. Social interventions are an excellent idea and should absolutely be a part of the treatment modality, but this article is 5% that point and 95% anti scientific, biased nonsense.
Report comment
They should remember that it’s a social solution and not a physical solution the next time someone tells them that they want to mutilate their genitals.
Report comment
I like this article.
MY bona fides…an alumnus of
Psychotropic Gladiator School, PhD honors program, & post-grad research studies.
I wish they also emphasized the diagnostic targeting of all females in their essay (as ex: schiz-Black males). Ya’ know-more than half the global population…by the male drivers of the psych industry…..
Their mentions of female activist groups with common-sense & compassionate alternative ‘treatment’ was very good. (It didn’t connect the dots tho)’.
On Borderline….BPD is just the diagnosis ‘du jour’… bu11sh$t.
As bipolar disorder was ‘waning’….challenged more & more frequently….the ‘new’ re-purposed shiny object/ICD code was THIS crap. We’ve seen this movie.
Like BD, females are the targets for borderline diagnoses…and drugged sedation also.
*To the annoyed Commenters who don’t get what all the ‘fuss’ is about at MIA….
**Who ARE the living human models of Behavioral Perfection writ large, we should be aspiring to mimic…according to the psychiatric industry-U.S. and/or global?
*Name just ONE…& make your case. Take your time.
I’ll be right here.
Report comment
There are some people who think psych meds help them but they’re not told the truth: that the drugs are designed to be “needed” for life because they don’t cure anyone. The late psychiatrist, Abram Hoffer, MD, treated almost all his patients with niacin, which is one form of vitamin B-3 and he had a very high success rate in restoring his patients’ mental health. It worked miracles for my “ADHD” son but it did nothing for my “bipolar with psychosis” son. What restored his mental health was following Dr. Carl Pfeiffer’s work on histamines. As I lowered my son’s histamine level with nutraceuticals from our local health food store, his psychiatric symptoms disappeared and his mental health was restored. And now I know of a second restorative approach, both of which the Amer Psych Ass’n has been FIGHTING for decades. If you think the APA cares about YOU, you’re wrong. They’re in it for the profit. –Linda from YT, “Linda Van Zandt’s Mental Health Recovery Channel”
Report comment
This whole situation is very paradoxical for me.
What Fanon gets is obvious: Of course forced poverty, famine, political inequality and race baiting or other suppressive social practices are going to make the targeted people feel like shit.
But what Fanon misses should also be obvious, though these days still is not: That “mental problems” exist in all strata of society, that being physically or politically comfortable does not equal being mentally comfortable, and that most researchers have no idea what human beings really are, how we have suffered, or what our actual situation on Earth is.
If anything, the politically and financially comfortable are better at hiding the mentally and emotionally deficient that exist among them, and yet those beings probably pose the most danger to society. The poor, the hungry, the unhoused are not the ones starting or supporting wars or other forms or social unrest, nor the ones financing such social atrocities. The ones who are doing that are the truly sick.
So, how does Fanon’s model solve the problem of mental and emotional depravity among the elites? I know that all attempts so far to eliminate or replace elitist structures with “populist” or “merit-based” structures have largely failed. The elites have always been able to figure out how to maintain or regain control. And among them is where the true problems lie. That is what I want to see addressed by the new generation of psychiatrists. If they don’t address that issue, I don’t trust them any farther than I can throw them.
Report comment