Another scientific study that ostensibly identifies a biological cause of schizophrenia has appeared and is being widely reported. According to the Los Angeles Times (1/27/16, emphases added):
“Scientists say they have broken new ground in the study of schizophrenia, uncovering a potentially powerful genetic contributor to the mental disorder …
“The study offers the first clear evidence of a neurobiological basis for a disease that places lifelong burdens on patients and their families.
“In a study hailed as a significant step in the search for schizophrenia’s roots, geneticists and neurobiologists zeroed in on a genetic region that … is linked to the mental disorder.
“‘Since schizophrenia was first described over a century ago, its underlying biology has been a black box …,” said geneticist Steven McCarroll of the Broad Institute and Harvard Medical School, the paper’s senior author. “The human genome is providing a powerful new way in to this disease. Understanding these genetic effects on risk is a way of prying open that block box, peering inside and starting to see actual biological mechanisms.'”
According to The Washington Post (1/27/16, emphases added):
“For the first time, scientists have pinned down a molecular process in the brain that helps to trigger schizophrenia. The researchers involved in the landmark study, which was published Wednesday in the journal Nature, say the discovery of this new genetic pathway probably reveals what goes wrong neurologically in a young person diagnosed with the devastating disorder.
“The study marks a watershed moment, with the potential for early detection and new treatments that were unthinkable just a year ago, according to Steven Hyman … a former director of the National Institute of Mental Health, [who called] it “the most significant mechanistic study about schizophrenia ever.”
“‘I’m a crusty, old, curmudgeonly skeptic,’ he said. ‘But I’m almost giddy about these findings.'”
“In patients with schizophrenia, a variation in a single position in the DNA sequence marks too many synapses for removal and that pruning goes out of control. The result is an abnormal loss of gray matter.
According to The New York Times (1/27/16, emphases added), the study showed that the
“…risk [of developing schizophrenia] is tied to a natural process called synaptic pruning, in which the brain sheds weak or redundant connections between neurons as it matures. During adolescence and early adulthood, this activity takes place primarily in the section of the brain where thinking and planning skills are centered, known as the prefrontal cortex. People who carry genes that accelerate or intensify that pruning are at higher risk of developing schizophrenia than those who do not . . .
“[This study is being hailed as] a significant step toward understanding the cause of schizophrenia, in a landmark study that provides the first rigorously tested insight into the biology behind any common psychiatric disorder. . . .
“They did a phenomenal job,” said David B. Goldstein, a professor of genetics at Columbia University who has been critical of previous large-scale projects focused on the genetics of psychiatric disorders. “This paper gives us a foothold, something we can work on, and that’s what we’ve been looking for now, for a long, long time.” . . .
So, we finally have the elusive breakthrough to understanding the biological basis of schizophrenia. Or do we? A close look at the source of all this hyperbolic language raises serious questions about such enthusiasm. (Also see Noel Hunter’s insightful analysis of the problems with this “breakthrough” finding.)
The Incredible, Shrinking, Schizophrenic Brain
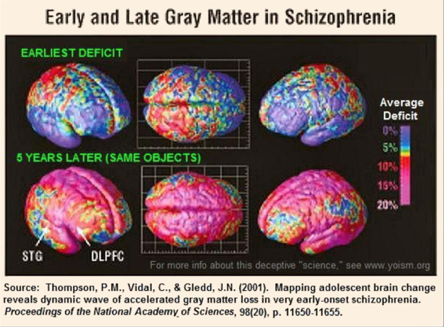
To understand the theory that brain shrinkage is linked to schizophrenia, we start with the fact that normal adolescent and young adult brains shrink. There have been a number of older studies that purportedly showed that “schizophrenic,” adolescent brains shrink more than “normal” brains and that excessive gray matter loss is associated with schizophrenia.
For example, the authors of the 2001 study, from which I obtained the illustration above, reported in the abstract for their paper:
. . . we detected striking anatomical profiles of accelerated gray matter loss in very early-onset schizophrenia; surprisingly, deficits moved in a dynamic pattern, enveloping increasing amounts of cortex throughout adolescence.
. . .These emerging patterns correlated with psychotic symptom severity and mirrored the neuromotor, auditory, visual search, and frontal executive impairments in the disease.
. . . These emerging dynamic patterns were controlled for medication and IQ effects
However, when I carefully read their article, these claims fell apart. Completely.
In order to confirm that the increased brain shrinkage was associated with schizophrenia per se and was not a result of neuroleptic exposure, medication effects were “controlled” by using a comparison group of psychotic but not schizophrenic adolescents (P/NS) who were supposedly equally exposed to meds as well as a control group of normal adolescents. As predicted, the P/NS group exhibited less brain shrinkage than the schizophrenic group. But the P/NS group had much less psychotic symptomatology and, as the body of the study reveals, apparently received far less neuroleptic exposure. Even though they received less medication than the schizophrenic group, the P/NS group did receive a considerable amount of antipsychotic medications and — surprise, surprise — they showed significantly more gray matter loss than the normal controls. The differences between the three groups were consistent with a correlation of gray matter loss with neuroleptic exposure.
So despite their claim that schizophrenia causes or is caused by gray matter loss, the actual data in the 2001 study actually supports the idea that there is a loss of gray matter due to neuroleptic exposure with significantly more loss with more neuroleptic exposure. This is precisely what was reported in a 2008 New York Times article describing twenty years of research by Dr. Nancy Andreasen, former editor of The American Journal of Psychiatry. (Also see Joanna Moncrieff’s more thorough discussion of the brain shrinkage-schizophrenia research.)
Fast Forward to Today’s Breakthrough Finding
The twenty-plus authors of the new, “landmark study” start with the assumption that “Schizophrenia is a heritable brain illness with unknown pathogenic mechanisms.” They believe they have now discovered a pathogenic mechanism (the “C4A” gene) for this heritable brain illness — a specific variation of a gene that leads to problematic pruning of synapses during adolescence and young adulthood. Here we run into a number of problems.
For argument’s sake, let’s assume that the unlikely, genuine breakthrough has occurred. I say unlikely because there have been dozens of supposed advances in the biological understanding of schizophrenia that have turned out to be spurious. But even if this one turns out to have some validity (i.e., if it is replicable) it may be grossly misleading to suggest that it in any way explains “schizophrenia.”
What the term “schizophrenia” refers to
As we know, schizophrenia is a term that is typically used to diagnose people who have exhibited psychotic symptoms as defined in a checklist found in the Diagnostic and Statistical Manual of the American Psychiatric Association (now in its fifth edition). Not being able to identify the cause of the constellation of symptoms referred to as schizophrenia, the diagnosis has had to be based on whether the individual exhibits two or more of the symptoms in the list (delusions, hallucinations, disorganized speech or behavior, catatonia, lack of emotional expression, avolition).
It is universally acknowledged by virtually all researchers that the set of symptoms we label schizophrenia may not be caused by a specific illness. We may be lumping together in one category phenomena with completely different etiologies. Even if we see the requisite number of symptoms on the list and have ruled out known, non-schizophrenic causes of psychosis, schizophrenia remains an umbrella term for a variety of functional problems.
Yes, we know that brain disorders can cause psychosis
Now, surely we can acknowledge that there are genuine, biological, brain disorders that cause psychosis — e.g., neurosyphilis can produce the symptoms of psychosis. As my brother-in-law lay dying of AIDS, he periodically suffered from an opportunistic brain infection (toxoplasmosis) that caused him to hallucinate people whom he would talk to. When he was treated with antibiotics, the hallucinations went away.
The claim of the current study could be seen in this light: They have discovered one such neurological, brain disorder caused by the C4A variant of a gene that guides synaptic pruning during the transition to adulthood. But just as neurosyphilis and toxoplasmosis are not explanations for the phenomena we call schizophrenia, neither would C4A disease be such an explanation. Yet even this more limited claim has some major difficulties.
The C4A gene is rarely associated with schizophrenia
Here we have our first problem. Approximately 4 in 400 people (1%) get diagnosed with schizophrenia. In contrast, among those with the C4 gene, 25% more or 5 in 400 people (1.25%) get diagnosed with schizophrenia. That’s the biological finding that is being considered a breakthrough in understanding schizophrenia! Yet this means that ~99% (98.75%, to be exact, or 395 out of 400) of those with the schizophrenogenic gene don’t exhibit symptoms of schizophrenia. How can this be said to be a finding of a biological cause for schizophrenia? Before I consider an alternative interpretation of the facts, let’s look at some other problems with this study’s conclusions.
Schizophrenia or C4A disease?
Amongst those who have been diagnosed with schizophrenia, only a small number have the C4A gene. It is possible — remember, we’re giving the researchers the benefit of the doubt and assuming their findings have replicable validity — that they have identified a real, neurological disorder that can be caused by a problematic gene. Since this would explain the phenomenon in only a small group of those who get the schizophrenia label, it is likely that — rather than identifying the cause of schizophrenia — they have identified a genetic disorder that interferes with proper brain development.
There are other genetic disorders that cause brain abnormalities that can induce psychosis, e.g., phenylketonuria, Tay-Sachs disease, Wilson disease, and the leukodystrophies. However, the DSM diagnostic criteria for schizophrenia explicitly state that, in order to make the diagnosis, “The disturbance [cannot be] attributable to . . . another medical condition.” So even if the resultant brain abnormalities from these genetic disorders on occasion cause psychotic symptoms, that would clearly not be schizophrenia. Just so, if a new genetic disorder has been found to cause psychosis, that is not schizophrenia; in the vast majority of cases, schizophrenia is used to refer to individuals without the C4A gene and whatever biological processes that gene may bring into play.
Schizophrenia and excessive loss of gray matter
Next. One of the findings that the authors are trying to explain is the loss of gray matter in schizophrenia. Yet, as we saw in the above analysis of a typical study that claims to show a link between schizophrenia and gray matter loss, that loss does not appear to be a cause of or caused by schizophrenia. Rather, the increased loss of gray matter is correlated with neuroleptic drug use that is known to cause brain damage; such increased loss has not been found in humans who were not exposed to significant amounts of neuroleptics.
There was no demonstration in the current study that the C4A gene was associated with a higher level of gray matter loss compared to those without the gene. Rather, because the C4A gene was associated with schizophrenic diagnoses and schizophrenia has been (misleadingly) associated with excessive gray matter loss, ergo the C4A gene causes greater gray matter loss.
An Alternative Interpretation of the Data
What the authors did not consider was the possibility that they had identified a genetic variant that is associated with increased interaction with a mental health system that frequently and forcefully administers brain damaging drugs. Such a tendency toward increased interaction with biopsychiatry that may be associated with the C4A gene is quite slight since the vast majority of those with the gene are never diagnosed with schizophrenia. Indeed, in the vast majority of cases, the tendencies that could cause a slight increase in association with mental health institutions are quite functional; almost all of those with the C4A gene do not develop severe mental illness.
Yet what adaptive personality traits might be associated with increased interaction with the mental health system? Keep in mind that, from an evolutionary biological perspective, a gene with only deleterious effects is unlikely to remain in the gene pool over many generations. So, what might be the adaptive effect of this variant of the C4 gene that has enabled it to remain fairly common, even if on occasion it can cause problems? Actually, it is not too difficult to think of quite a few that are not at all unusual.
Consider the Soteria approach to those who have experienced psychotic breaks versus standard biopsychiatry interventions. In the former, the individual is seen as being inherently healthy but under stress and needing support to find their own personal, adaptive manner of coming to terms with a problematic world. In the latter, the individual is seen as containing biological pathologies that make adaptation to a normal world difficult. While those with the C4A gene and a different pattern of brain development during adolescence may have a tendency to think and act in ways that are slightly more likely to conflict with their environment, such a tendency could be seen as either adaptive or pathological. The way such tendencies are understood depends on one’s perspective and the particular circumstances confronting the individual.
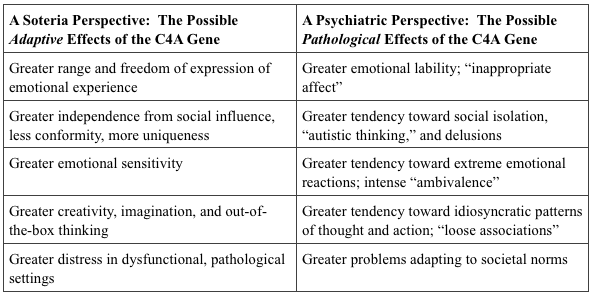
What the current study could be showing is that folks with the C4A gene are slightly more emotionally labile, slightly more likely to have problematic emotional reactions, and thus slightly more likely to come into contact with the mental health system. Once involved in the mental health system, if during a period of acute distress they get diagnosed with schizophrenia, they are quite likely to get pushed into the debilitating, lifelong neuroleptic exposure that dooms people to an ongoing diagnosis of schizophrenia. This could account for the tiny increase in schizophrenic diagnoses in those with the C4A gene.
Unfortunately, this “breakthrough” study is likely to be used to undermine the use of safe, effective psychosocial treatments and support a chemical intervention approach to all who’ve experienced psychotic episodes, most of whom will be irreparably and needlessly harmed.















Excellent post. Wish you would post more here.
Report comment
This article is an important community service; thank you for the real science!
It is frustrating that science writers have no memory of the history of past failed promises to temper enthusiasm for repeated “breakthroughs;” I wish that there was a directory of all the failed promises.
I thought that heredity theory proves that “schizophrenia” cannot be an inherited problem because it does not “breed true.” With the low (20%) reproductive rate of people diagnosed with “schizophrenia”, I understood that any heredity component would breed out of existence after a few generations. Is this a fair criticism of behavioral genetics?
Best wishes, Steve
Report comment
Steve, the 20% reproduction number is from developed countries where people labeled schizophrenia are heavily drugged, stigmatized, and not reintegrated into society. It is derived from following the most severely psychotic, most heavily distressed, most unsupported, most heavily drugged people from a few developed world mental hospitals. It therefore suffers from the clinician’s illusion in which severely troubled people appear to return to normal lives less frequently than is possible in better settings and without drugs. Drugs and mental hospitals often make people worse.
For example, when Courtenay Harding did a radio show on this topic, many, many people called in to say they had been labeled schizophrenic as youngsters but never got caught in the system and therefore never were included in the so-called studies of illusory schizophrenia. Many of these people calling in had gone on to live essentially normal lives with jobs and families. These people should be included in the studies of “schizophrenia”, but they are not due to pervasive unscientific researcher bias.
In poor countries like India, people labeled schizophrenic return to community and have kids and families at rates close to the normal population rate. This is detailed in companion studies to the original WHO longitudinal studies in which young men and women given the schizophrenia label in rural India are followed for years after their “diagnosis”. So the 20% reproductive notion wouldn’t even hold up there. “Schizophrenia” should in theory persist in India, but die out within a few generations in the USA. This just illustrates what bullshit schizophrenia is if considered to be a disease.
The whole biological and genetic explanation of schizophrenia is a fantasy that psychiatrists cannot seem to give up.
In either case, whether the “developed” world or the poor world where outcomes are better, there is no proof there is anything biologically or genetically different ab initio in those who get labeled schizophrenia. Most likely they are mostly the unfortunate victims of much worse life experiences.
Report comment
I thought that it was a simple question; will an inherited disease breed out of existence in a few generations if those affected have a 20% reproductive rate?
Report comment
Well of course it would… but biological researchers don’t want to admit that their diagnostic categories are fraudulent, and that what is really happening is that people who have been through unbelievable trauma, are given no therapy, and are buried under drugs, have trouble with getting jobs, establishing intimate relationships and having kids… what a surprise.
Report comment
Always enjoy your comments, BPTD. Hope you’re writing your own stuff (articles) somewhere.
Report comment
Thank you. My articles are at http://bpdtransformation.wordpress.com
And I will soon be making a new site about how to heal psychotic experience and why there is no valid illness called schizophrenia. I will link to it from the BPD site.
Report comment
“Schizophrenia” considered as a medical illness is like a slowly sinking Titanic that already hit the iceberg and should be abandoned. Here’s a summary of Jim Van Os’ recent research on the concept’s flaws:
“Scientific evidence indicates that the different psychotic categories can be viewed as part of the same spectrum syndrome, with a lifetime prevalence of 3.5%, of which “schizophrenia” represents the minority (less than a third) with the poorest outcome, on average. However, people with this psychosis spectrum syndrome—or, as patients have recently suggested, psychosis susceptibility syndrome6—display extreme heterogeneity, both between and within people, in psychopathology, treatment response, and outcome.
The best way to inform the public and provide patients with diagnoses, therefore, is to forget about “devastating” schizophrenia as the only category that matters and start doing justice to the broad and heterogeneous psychosis spectrum syndrome that really exists.
ICD-11 should remove the term “schizophrenia.”
Here’s the manifesto from Van Os’ website, “Schizophrenia Does Not Exist” –
https://www.schizofreniebestaatniet.nl/wp-content/uploads/2015/03/Manifest_UK.pdf
As Van Os suggests, schizophrenia should be abolished from the DSM and ICD, and replaced with a concept of something like Psychosis Susceptibility Syndrome. This will do justice to the great variation between individuals, and to the fact that psychotic people are not psychotic all the time, and that we not know that psychotic states are caused by brain chemistry or genes (most evidence suggests they are mostly not).
The only reason to keep schizophrenia is if people want to drug companies to keep profiting from overdrugging and psychiatrists to keep their vaunted status as medical experts on an illusory disease. Few people want that outside of corporate CEOs, shareholders, psychiatrists, and the 1%.
Report comment
That’s already being done,but the folks doing it are generally regarded as quacks and crazies who haven’t regarded the DSM mode of identifying mental conditions as realistic and prattle about syndromes with multiple causes, as happens in general medicine.
Report comment
regarded as quacks by whom?
Report comment
Here again is my critique of the McCarroll C-4A study:
———
Here are adapted excerpts from a letter I sent to four of the principal authors behind this research: ————–
Dear Professors Stevens, McCarroll, Barondes, and Lander,
I’m a member of the organization ISPS (the International Society for Psychological and Social Approaches to Schizophrenia, http://www.isps.org) and also a person who was once diagnosed with schizophrenia but fully recovered.
I am emailing you because I wanted to give you a window into our group’s discussion of this research. I thought you would find it interesting and perhaps useful. Below, I have put a long comment from our listserv that I placed there today. I expect you may find it disturbing and challenging to read (and I apologize, do not take my critique personally; it is possible that Benedict Carey oversimplified or miscommunicated some of your findings) – but I encourage you to read through it because it may broaden your perspective about schizophrenia in an eye-opening way.
Lastly, I’d like to also share with you some of our research into psychosocial approaches for psychotic states and schizophrenia. Some of the best psychosocial approaches to “schizophrenia” have been able to return about 80% of first episode-psychotic schizophrenic youth to full engagement with work and relationships, usually with no or minimal remaining psychotic symptoms. The recent RAISE, EASA, and PREP trials actually adopted significant aspects of the models we pioneered. However, this work, particularly the Open Dialogue approach and the 388 program, is little known in the United States due to the dominance of the biological model. Here’s a look:
The Open Dialogue Approach to Schizophrenia:
http://www.taosinstitute.net/Websites/taos/Images/ResourcesManuscripts/seikkula-OpenDialoguesWithGoodAndPoorOutcomes.pdf
http://psychrights.org/Research/Digest/Effective/fiveyarocpsychotherapyresearch.pdf
The 388 Program, A New Perspective for Treating Schizophrenics
– https://www.youtube.com/watch?v=mmqT-4W4Cvg Individual Psychotherapy for Schizophrenia, Lewis Madrona’s Approach
http://www.transpersonalstudies.org/ImagesRepository/ijts/Downloads/IJTS_33-1-07_pp_57-76_Mehl-Madrona_et_al_2014_Results_of_a_Transpersonal_Narrative_and_Phenomenological_Psychotherapy_for_Psychosis.pdf
Gottdiener’s Meta-analysis of Psychotherapy for Schizophrenia
http://psychrights.org/Research/Digest/Effective/BGSchizophreniaMeta-Analysis.htm
———————————— (My own comment on ISPS listserv)
I would like to offer a detailed critique of the Benedict Carey article reporting progress in discovering the “Cause of Schizophrenia” of January 27
(http://mobile.nytimes.com/2016/01/28/health/schizophrenia-cause-synaptic-pruning-brain-psychiatry.html?hp&action=click&pgtype=Homepage&clickSource=story-heading&module=second-column-region%c2%aeion=top-news&WT.nav=top-news&referer=&_r=0)
I took some time this morning to cut out quotes from the article and offer my responses. These are my opinions:
“(Scientists have) taken a significant step toward understanding the cause of schizophrenia”
Response: I cannot say it better than Brian K: “There is no entity called “schizophrenia.” It is a syndrome and heterogeneous. The New York Times article “Scientists Home in on Cause of Schizophrenia,” is misleading in its title. It is not a single category (nature is not “carved at her joints” and our genomes did not evolve to reify DSM categories), nor is there one “cause.” The research is correlational not causal.”
“insight into the biology behind any common psychiatric disorders”
This phrase presumes that psychiatric disorders are valid, reliable medical classifications. This is false: Mary Boyle, Richard Bentall, Jeffrey Poland, Paula Caplan, Stuart Kirk, and others have argued convincingly that these labels do not represent discrete entities that can be reliably identified by different outside observers. Therefore the “scientific” research on them is not truly scientific.
“drugs… blunt some of (schizophrenia’s) symptoms but do not touch the underlying cause.”
This mistakenly assumes there is one” cause of “schizophrenia” or psychotic states. But the research from the Adverse Childhood Experiences study, from John Read, etc. strongly implies that there are many complex causes that can lead to psychotic states (“schizophrenia”) in different combinations. For example, incest, child abuse, social isolation, illicit drug use, lack of sleep, all could lead to psychotic states of different kinds that get labeled “schizophrenia.”
“why the disorder often begins in adolescence of young adulthood” – This is because psychosis is probably not primarily an illness caused by biology, but primarily a social-psychological-experiential reaction to the world that is expressed in biology. The biggest risk period for vulnerable people is when they are in their teens or 20s when their parenting/social support is not adequate for the task of moving into adulthood and becoming independent. If they are overwhelmed by this transition, psychosis may result.
“provided researchers with their first handle on schizophrenia”
Again this mistakenly assumes that there is one reliable discrete entity called schizophrenia, that can be caught, like a fly in amber. But this is an illusion…
“That risk (of developing “schizophrenia”, another misleading description) is tied to a natural process called synaptic pruning, in which the brain sheds weak or redundant neurons as it matures…People who carry genes that accelerate or intensify that pruning are at higher risk of developing schizophrenia than those who do not, the new study suggests.”
I will quote Brian K’s wise words at length again:
“The increased expression of the complement C4A gene may be associated with other processes. First, it is important to rule out confounds like antipsychotic use. APs have effects on our immune system. There are dopamine receptors on immune cells. The MHC (major histocompatibility complex), referred to in the article is involved in cell-mediated immunity-MHC proteins bind viral or bacterial coat proteins, take the peptides to the cell surface where they can be killed by cytotoxic lymphocytes (which stops the cell from being a host to viral replication). There is a great deal of research being done on the role of neuroinflammatory processes (e.g., microglia) in psychosis, depression, etc.
Second, one must search for other correlations. In regard to the latter, Bronikowski et al (2002) found that inflammatory and stress response genes were most affected by physical inactivity and age. Twenty one inflammatory response genes were upregulated (increased) by age in a sedentary group, including complement C4 (which is invloved in immune function). I wonder if loneliness (and other chronic stressors) also can play a role, since it has significant effects on immune function. The NY Times article neglected to refer to the myriad of social factors demonstrated to play a role in the diagnosis, onset, course and outcome of “schizophrenia,” e.g., urban birth/living, migration, social defeat/social isolation, expressed emotion and communication deviance, childhood maltreatment, etc.”
I think it is particularly important to note that this article said absolutely nothing about childhood abuse and social isolation as causes of receiving a schizophrenia diagnosis. The ACE Research and John Read’s research implies that these factors are often much more important than any genetic contribution. Understanding these factors does not have to mean blaming the parents or the individual. Further, I wonder whether these researchers are using a model that is truly epigenetic and interactional, i.e. appreciating how much genes are modified by environment/experience after birth. Again, in this context the monolithic construct of schizophrenia is outdated and due for abolition.
“any step forward is not only rare and unusual, it’s just one step in a journey of a thousand miles” to improved treatments.”
This implies a narrative of gradual progress at improving treatments (and presumably outcomes) for people labeled schizophrenia. But that is a false narrative. The latest meta-analysis from Jaaskelainen (2013) clearly shows that outcomes for people labeled schizophrenic have been gradually worsening in recent decades, for both symptomatic and functional outcomes. Thus the continued biological and genetic research is not enabling a gradual movement forward to improved treatments. The narrative of psychiatry and schizophrenia is not one of progress and improvement, but one of increasing failure and chronicity.
“Some researchers had suspected that the pruning must somehow go awry in people with schizophrenia, because previous studies showed that their prefrontal areas tended to have a diminished number of neural connections, compared with those of unaffected people.”
Again, this research is only correlational, not causal, and suffers severely from the lack of validity of the concept schizophrenia. The researchers also neglect the possibility that adverse environmental experience (e.g. loneliness, abuse) could be the primary (epigenetic) influence driving the process of accelerated pruning.
“(this research) identifies the genes responsible (for accelerated pruning)”
This research appears to be reductionistically viewing genes, in a pre-epigenetic way, as isolated actors which “do things” to people’s development. But genes do nothing without environmental input and interaction. So the possibility remains that the real link could be to the environmental experiences and interactions that are driving those genes to prune the neurons faster.
“provides a showcase of biomedical investigation at its highest level.”
Perhaps it would be more accurate to say that they are investigating a disease which has not been proven to exist as a discrete entity, and which may well have no one clear biomedical cause, in one way of understanding.
“speculation that schizophrenia might be a kind of autoimmune condition, in which the body attacked its own cells.”
It is incredible that this type of possibility is still seriously considered, in light of, 1) The lack of validity and reliability for labels such as schizophrenia, 2) The strong research that John Read has catalogued linking trauma to being diagnosed with schizophrenia. It speaks to the strong distorting influence that the drug companies’ money have on research and inadvertently on the minds of researchers.
“C4-A could mean too much pruning — which would explain not only the thinner prefrontal layers in schizophrenia, but also the reason that the disorder most often shows itself in people’s teenage years or early twenties.”
Like Brian, I am not purely or irrationally against genetic research. I think it’s possible that the overactive C4-A gene could confer a slightly increased risk for being overwhelmed by the stresses of life, all other factors being equal (in the statistical, aggregate sense). But that is very different from saying “this gene drives risk for schizophrenia.” Someone having an overactive version of this gene might never become psychotic due to other ameliorating factors. If I understand it right genes do not operate autonomously, but in concert with environmental influences which in turn can modify them throughout life. Further, it’s quite likely that this gene (and genes in general) might confer only a tiny percentage of the risk of “getting labeled with schizophrenia” (which is all it is, schizophrenia is not an illness someone has, but a label someone is given). Environmental-experiential factors may make up a far larger proportion of the risk of being so labeled, given the limitations of twin studies that Jay Joseph and Jonathan Leo have exposed (i.e. the notion that schizophrenia is 70 or 80% genetic is a myth; Brian Koehler is also working on a new model of this research).
“Having such a variant, Dr. McCarroll estimates, would increase a person’s risk by about 25 percent over the 1 percent base rate of schizophrenia — that is, to 1.25 percent.”
This is an admission of how small the influence of any one gene or group of genes is likely to be, and why genetic research into “schizophrenia” is unlikely to ever yield significantly improved outcomes, given the complexity involved in genetic-environmental interaction. Further, this sentence mistakenly assumes that there is a “1 percent base rate of schizophrenia”. But that is not a reliable average – “schizophrenia” is more common among poor people, certain ethnic groups, in inner cities, in certain developed countries, etc.
“That is not nearly enough to justify testing in the general population,”
Again, there would be little point to such testing because schizophrenia is not one coherent entity that can be reliably identified.
“The researchers hope that the at-risk genetic profile, once it has been fleshed out more completely, will lead to the discovery of biomarkers that could help clarify a prognosis in these people.”
This appears to me to be similar to the hopes of developing cold fusion or gold alchemy. The genetic environmental interaction that leads to individual psychotic states of greater or lesser severity is too complex to be reduced reliably to biomarkers, I think.
“Developing a drug to slow or modulate pruning poses another kind of challenge.”
Such a drug would probably not work because pruning must be subject to myriad internal and external genetic and environmental factors; I cannot imagine a pill that could precisely influence such a process, effectively reversing human pathological mind-body development from a biological level. Such a pill would almost have to be a “reverse time travel” pill or an “entire environment influence” pill that would do what human/environmental/biological curative influences together can do. Mind boggling.
“But I’m not ready to call it a victory until we have something that can help patients.”
I do not feel very optimistic about this, and would note that very effective social-psychological approaches that work such as Open Dialogue, 388, and intensive psychodynamic psychotherapy for schizophrenia already exist.
As Noel said, it is sad to see that strong research on trauma, abuse, and social influences contributing to “schizophrenia” (below) is totally ignored while this research, which is actually very weak in its effect size and embryonic in its stage of development (if it ever progresses further), gets highlighted.
https://www.researchgate.net/publication/282043036_Impact_of_childhood_adversities_on_specific_symptom_dimensions_in_first-episode_psychosis
Furthermore, biological-genetic research continues to correlate with increasing rates of psychiatric disability:
http://www.madinamerica.com/2016/01/what-disability-benefit-trends-tell-us-about-psychiatric-treatments-and-the-economy/
Feel free to comment on any of these opinions. ——————–
Report comment
As previously noted, the researchers behind this study are like paper tigers or emperors without clothes, totally unable to engage in a meaningful dialogue with their critics. Instead, they must respond with denial and avoidance, since actually facing our criticisms would expose their work as fraudulent bullshit.
Their entire study rests on false assumptions about “schizophrenia” being a unitary, brain-based disease. And therefore all of their work is extremely vulnerable to attack. It must suck to be a so-called doctor in a profession (psychiatry) which is afforded so little respect because people can sense that its foundations are rotten and spurious.
Report comment
Dear Dan Kriegman, PhD:
Thank-you, sir. I KNEW there was HOPE, over 20 years ago, when I last signed myself out “a.m.a.” from the local psych ward. I haven’t been back to the pseudo-science drug racket of psychiatry since. I will not EVER go back. I wish I’d heard of Soteria before Pharma & the LIE of psychiatry got their hooks in me. It’s called “iatrogenic neurolepsis”. And it gave me PTSD. Prison, jails, homeless, group homes, and DRUGS. That’s what psychiatry gave me. God only knows where the HOPE came from….
etc., Please email me. I WANT to get my story out there. But yes, I AM still disabled, and impoverished.
(c)2016, Tom Clancy, Jr., *NON-fiction
Report comment
This is an excellent discussion of an overly hyped study. I read the NYT article on the study and thought it was inadequate and misleading. I’m so glad you posted this analysis in MIA.
Report comment
Thank you, Dan, for helping to expose what I believe should be called psychiatric propaganda. And I’d like to point out that the “gold standard” treatment for “schizophrenia,” the neuroleptic drugs, do indeed, all by themselves, create both the negative and positive symptoms of “schizophrenia.” And point out that the doctors are not able to distinguish between the adverse effects of the neuroleptic drugs, and the symptoms of “schizophrenia.”
The neuroleptics can create the negative symptoms of “schizophrenia,” via neuroleptic induced deficit disorder, as discussed in this blog from yesterday.
http://www.madinamerica.com/2016/02/researchers-call-for-reappraisal-of-adverse-mental-effects-of-antipsychotics-nids/
And the neuroleptics can create the positive symptom of “schizophrenia” via the central symptoms of neuroleptic induced anticholinergic intoxication syndrome, aka anticholinergic toxidrome.
https://en.wikipedia.org/wiki/Toxidrome
Given the reality that the adverse effects of the neuroleptic drugs are indistinguishable from the symptoms of “schizophrenia,” I do believe it’s highly likely that most so called “schizophrenia” today may actually be a completely iatrogenic, rather than genetic, illness.
Report comment
Thanks Dan,
“..The differences between the three groups were consistent with a correlation of gray matter loss with neuroleptic exposure…” Of course; and this is typical.
Report comment
This spurious pseudoscience is being used to prop up the ECT industry as well as big pharma. It smacks of attempts to shore up and find new markets for failed drugs (Prozac for menopause and Impulsivity?), and an old-fashioned destructive procedure that should have joined its contemporaries in the museum 40 years ago. Consequently there is a constant stream of jargon-filled, problematic nonsense masquerading as `science’ that can be taken apart by a 15 year old high school student, defending its use. What is concerning is that the perpetrators manage to publish without question. Surely this reflects on the publications as much as on the authors. It is one thing to offer questionable, if not overtly fraudulent, work to a publisher, but the publisher is then responsible for offering this to the public. Of course there are many who can critique this stuff but unless the publications present that too, the critics are merely `ratbag anti-psychiatrists’, sadly misinformed, non-scientific, ignorant, raving mad, sick and/or those with other vested interests. So, critical thinking not being a common attribute, the public at large believe what they see in the `reputable’ journals presented uncritically by DOCTORS, who have a reputation of being not only scientists, but intrinsically honest, well educated, ethical, morally sound pillars of the community. Mad in America is not seen in that light by the man in the street. Mainstream psychiatry constantly maligns MIA and publishes articles and rebuttals with impunity. How to overcome this? I wish I knew. I want establishment psychiatry to agree to a face to face debate like the Mausdsley Debate, about the proliferating use of ECT, but of course they won’t because, like the recent one on drugs, they will lose, and they know it. I would be ashamed to be a psychiatrist right now, but as Mary Maddock quoted: `It is difficult to understand something when one’s livelihood depends on not understanding it.’
Report comment
Again any conclusions of such studies must be considered irrelevant since they are based on the indemonstrable assumption that schizophrenia exists and that the subjects “have it.”
What people should be focusing on is the way such convoluted reasoning will be used politically, i.e. to further concepts such as “anosognosia” and “legitimize” forced psychiatric procedures.
Report comment