My personal + professional advocacy and mission work didn’t start with mental illness.
I Chaired the University of Washington’s Lesbian, Gay, Bisexual and Transgender student organization at 18 years old. I watched helplessly as friends faltered by an un-named plague. I learned advocacy and coalition building through participation with Queer Nation and ACT UP (SILENCE = DEATH) in Seattle and the State of California. A few years later, work with the California State Legislature during the late 80s, through the early 90s, with Assembly Member Sam Farr (28th AD, D-Carmel, CA) whose eventual ascendency into the vacated Congressman Leon Panetta’s 17th CD seat (Monterey/Santa Cruz, CA) introduced me to Dianna Feinstein, Barbara Boxer, Nancy Pelosi and Bill & Hill Clinton.
Leon was appointed to Bill’s cabinet as Chief of Staff nearly immediately after President Bill Clinton’s election and Sam did actually win the 17th CD in over-time in that special redistricting. While working with the California State Legislature, I represented Assembly Member Sam Farr on the Monterey County AIDS Project where I learned about HIV/AIDS and advocated for Gay, Lesbian, Bisexual and Transgender communities in the U.S.
The National Coalition for Lesbian, Gay, Bisexual and Transgender Health Announced a State of the Coalition Call for the scheduled and promoted “Come Out for Health – March 26-30” with further information available at http://lgbthealth.webolutionary.com/content/national-lgbt-health-awareness-week. Learn how the Coalition and its members across the country are advancing the four core principles of consumer empowerment, culturally-competent services, engaged communities and inclusive policy making. The Coalition staff will provide an overview of a congressional briefing scheduled in Washington, DC, and highlight resources available to support efforts across the country.
A February 29, 2012 call included reports about activities planned across the country from: Januari Leo – Public Affairs Field Specialist, Legacy Community Health Services, Houston, Texas; Chad Putnam – Board President, Rainbow Health Access Initiatives, Inc., Albany, New York; Justin Neisler – GHSU Equality, Georgia Health Sciences University, Augusta, Georgia. Contact Kaye Gooch at [email protected]
Other useful sites are:
Hearts and Ears – Baltimore, http://www.heartsandears.org/
GLBT National Hotline 1-888-THE-GLNH
The GLBT Hate Crimes Hotline 1-800-686-HATE
LYRIC Youth Talkline 1-800-246-7743
National Center for Lesbian Rights (NCLR) Legal Helpline 1-800-528-6257
National LGBT Youth Hotline 1-800-246-PRIDE
The National Runaway Switchboard1-800-RUNAWAY
National Suicide Prevention Helpline 1-800-273-TALK
Peer Listening Line for LGBT Youth 1-800-399-PEER
The Trevor Lifeline 866 4-U-TREVOR 1-866-488-7386 [http://www.theTrevorProject.org has a LBGT suicide prevention hotline Trevor Helpline For gay, lesbian, bisexual or questioning youth and can be reached at the 24/7 staffed 1- 800-850-8078].
In Brooklyn, The Rainbow Heights Club New York can be found online at http://www.rainbowheights.org. Rainbow Heights’ conferences occur annually and are called “E/Quality Care,” http://www.equalitycare.org.
In 2008 I had published the findings of my graduate work while at the University of Texas at Austin[9]. It is seminal in my public health work and I learned that Austin State Hospital has perhaps the finest Inpatient program of supports that I have seen to date. The education pilot program I developed was developed for the Department of Texas State Health Services Austin State Hospital Education and Rehabilitation Adult Psychiatric Services acute and forensic inpatient units. Individuals living with seriously persistent mentally illness are being hard hit with comorbidities and certainly, HIV isn’t a stranger to us. Homelessness, polychemical and substance abuse, high and at-risk behaviors make us prime targets placing us as a dangerously disparaged population. That public mental health recipients are dying on average 25 years earlier than the general population places an emphasis on wellness and whole health.
When AIDS first surfaced in the United States, there were no medicines to combat the underlying immune deficiency and few treatments existed for the opportunistic diseases that resulted. Researchers, however, have developed drugs to fight both HIV infection and its associated infections and particular types of cancers. The first group of drugs used to treat HIV infection, called nucleoside reverse transcriptase (RT) inhibitors, interrupts an early stage of the virus making copies of itself. These drugs may slow the spread of HIV in the body and delay the start of opportunistic infections. This class of drugs, called nucleoside analogs, include: AZT (Azidothymidine), ddC (zalcitabine), ddI (dideoxyinosine), d4T (stavudine), 3TC (lamivudine), Abacavir (ziagen), Tenofovir (viread), Emtriva (emtricitabine). Health care providers can prescribe non-nucleoside reverse transcriptase inhibitors (NNRTIs), such as: Delavridine (Rescriptor), Nevirapine (Viramune), and Efravirenz (Sustiva) (in combination with other antiretroviral drugs). FDA also has approved a second class of drugs for treating HIV infection. These drugs, called protease inhibitors, interrupt the virus from making copies of itself at a later step in its life cycle. They include: Ritonavir (Norvir), Saquinivir (Invirase), Indinavir (Crixivan), Amprenivir (Agenerase), Nelfinavir (Viracept), Lopinavir (Kaletra), Atazanavir (Reyataz), and Fosamprenavir (Lexiva).
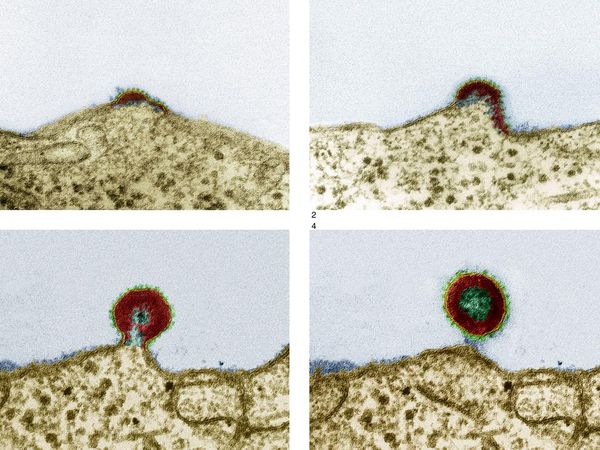
 The FDA also has introduced a third new class of drugs, known at fusion inhibitors, to treat HIV infection. Fuzeon (enfuvirtide or T-20), the first approved fusion inhibitor, works by interfering with HIV-1’s ability to enter into cells by blocking the merging of the virus with the cell membranes.
The FDA also has introduced a third new class of drugs, known at fusion inhibitors, to treat HIV infection. Fuzeon (enfuvirtide or T-20), the first approved fusion inhibitor, works by interfering with HIV-1’s ability to enter into cells by blocking the merging of the virus with the cell membranes.
This inhibition blocks HIV’s ability to enter and infect the human immune cells. Fuzeon is designed for use in combination with other anti-HIV treatment. It reduces the level of HIV infection in the blood and may be active against HIV that has become resistant to current antiviral treatment schedules. Because HIV can become resistant to any of these drugs, health care providers must use a combination treatment to effectively suppress the virus. When multiple drugs (three or more) are used in combination, it is referred to as highly active antiretroviral therapy, or HAART, and can be used by people who are newly infected with HIV as well as people with AIDS. Researchers have credited HAART as being a major factor in significantly reducing the number of deaths from AIDS in this country.
While HAART is not a cure for AIDS, it has greatly improved the health of many people with AIDS and it reduces the amount of virus circulating in the blood to nearly undetectable levels. Researchers, however, have shown that HIV remains present in hiding places, such as the lymph nodes, brain, testes, and retina of the eye, even in people who have been treated.
In 2008[9], HIV/AIDS among the seriously persistent mentally ill population exceeded the popular and commonly held belief that man to man contact leads the population most effected by HIV transmission by 10% to .02% . HIV was the leading type of and rate of transmission and infection placing an emphasis on high risk behavior management, education and testing as key in reducing the epidemic in psychiatric facility inpatient/outpatient populations (Padron, Psychiatric Quarterly Journal, 2008; Rothbard, Psychiatric Services 54(9):1240–1246, 2003). The Information-Motivation-Behavioral Skills Model (IMB), I referenced and utlized in my study, is an integrative framework to explain HIV risk reduction most often used and tested with the seriously, mentally ill population (Carey et al. Journal of Consulting and Clinical Psychology 72(2), 2004; Donenberg AIDS Education and Prevention 17(3):200–216, 2005; Meade and Sikkema Clinical Psychology Review 25(4):433–457, 2005; Rosenberg et al. Comprehensive Psychiatry 42(4):263–271, 2001).
- AIDS T-Cell Process of Growth
To determine the strength of correlation between psychiatric symptomology and HIV/AIDS knowledge (Pearson r), McKinnon, et al. developed a prediction model using multiple logistic regression analysis, requiring dichotomous categorical variables. Variables (patient’s age, number of hospitalizations, GAF score, PANSS score, total level of HIV/AIDS knowledge) were dichotomized above and below the median level. The level of education was determined to be before and above high school graduation. Similarly, ethnicity was focused singularly between Caucasian and African American because at one site, HIV infection rates were found higher than average among African American patient populations. PANSS scores were divided among the cognitive abilities (conceptual disorganization, difficulty with abstract thinking, disorientation, poor attention, mannerisms/posturing); score ranges of 5–35, and psychiatric symptomological positive, negative, excited, or depressed/anxious behavioral attributes. Variables significant by chi-square test at P\.05 were tested for IVDU concurrently and five types of sexual behavior within the previous 6 months to study participation.
Males (64%) comprised the sample and the most prevalent SCID diagnosis was schizophrenia (49.4%), bipolar (11.8%), major depression (7.3%), and other Axis I disorders (2.3%). These numbers were asymptomatic upon examination. Ninety-two (51.7%) of 178 patients reported being sexually active in the previous 6 months. Of the sexually active patients, 44 or 47.8% of 92 had multiple sexual partners, 32 (35.2%) of 91 used drugs during sex, 27 (29.7%) of 91 traded sex for good or drugs, and 50 (58.1%) of 86 never practiced sex using sexual barriers (male/female condoms, dams) and 31 (17.5%) of 177 patients reported MSM/MSF and concurrent IVDU abuse. Comorbidity of schizophrenia and viral illnesses yield typically greater levels of coinfection of HIV and HCV[3]. Dinwiddie et al. [4] found that in a study of 1,556 psychiatric inpatients, 8.5% were positive for HCV, and a Rosenberg et al. [9] study on the prevalence of HIV, HBV, HCV in people with chronic, episodic SMI a higher prevalence of 19.6% of 931 patients reported. There are, to date, no data on HCV prevalence rates associated with any specific psychiatric DSM-IV, Axis I., Axis II diagnoses [3]. Effective means of clinically, medically necessary treatment of SPMI, HCV and HIV antiretrovirals for HIV lends credence to positive, proactive treatment methods to assist the SPMI population.
There is not mandatory screening of incoming psychiatric inpatient individuals. High risk factors—unprotected sexual contact without condoms and IVDU (shared needles, dirty needles)—associated with HIV transmission are the same with schizophrenia as in the general population [9]. The higher prevalence of HIV and the seriously persistent mentally ill population may be attributed to increased high-risk exposure via substance abuse factors, and cognitive, excited, or positive symptoms with high-risk behaviors ‘‘common among patients who are sexually active.’’
The cognitive and social determinants for health include information, or knowledge about transmission and prevention behavior and motivation to reduce risk, or personal attitudes about preventive behavior, perceived normative support for HIV prevention, and behavioral intentions. The behavioral component included developing skills to practice prevention, including perceived self-efficacy and the ability to negotiate AIDS prevention with a partner [5].
A 1996 study from the Columbia University College of Physicians and Surgeons, the New York State Psychiatric Institute, supported by a National Institute of Mental Health grant MH46251 and the New York State Office of Mental Health, with additional provided technical assistance from the Center for Mental Health Services, Substance Abuse and Mental Health Services Administration (SAMHSA) was completed on the prevalence of HIV/AIDS in the SMI population for inpatient psychiatric populations that examined the relationships between diagnosed psychiatric symptomology, HIV and AIDS knowledge and high-risk HIV behavior [7].
It was determined that the seroprevalence rate of HIV transmission in the seriously persistent mentally ill population of 10% compared to the general and man to man population of .02% exceeds the accepted opinion that man to man HIV transmission is the highest mode of transmission currently, and that further programming and education is recommended. AIDS knowledge appears to be relatively good among psychiatric patients yet knowledge alone has not been shown to influence risk behavior levels [6]. A more effective approach to reducing high risk behaviors is to include HIV risk education and skills training in sexual assertiveness, negotiation, problem solving, use of condoms, safe sex education and risk self-management. Risk self-management includes identify and learning to monitor personal risk triggers and developing an understanding of situations when risk behaviors are most likely to occur [6].
A question to be begged in the CSX population is to essentially discover information and develop education, promotion and a hall-mark marketing effort to effect whole health and wellness in the high/at-risk behavior of the seriously peristent mentally ill population.
Citations
1. Carey MP, Carey KB, Maistio SA, Gordan CM, Schroder KEE, Vanable PA: Reducing HIV-risk behavior among adults receiving outpatient psychiatric treatment: Results from a randomized controlled trial. Journal of Consulting and Clinical Psychology 72(2), 2004. Retrieved from EBSCO Host Research Databases on April 11, 2006.
2. Cournos F, Mckinnon K: HIV seroprevalence among people with severe mental illness in the United States: A critical review. Clinical Psychology 17:259–269, 1997
3. Cournos F, Mckinnon K, Sullivan G: Schizophrenia and Comorbid Human Immunodeficiency Virus or Hepatitis C Virus. Journal of Clinical Psychiatry 66(Supplement 6):27–33, 2005
4. Dinwiddie SH, Schicker L, Newman T: Prevalence of hepatitis C among psychiatric patients in the public sector. American Journal of Psychiatry 160:172–174, 2003
5. Donenberg GR, Schwartz RM, Emerson E, Wilson HW, Bryant FB, Coleman G: Applying a cognitive behavioral model of HIV risk to youths in psychiatric care. AIDS Education and Prevention 17(3):200–216, 2005
6. Mckinnon K, Cournos F, Herman R: HIV among people with chronic mental illness. Psychiatric Quarterly 73(1):17–31, 2002
7. McKinnnon K, Cournos F, Sugden R, et al.: The relative contributions of psychiatric symptoms and AIDS knowledge to HIV risk behaviors among people with severe mental illness. Journal of Clinical Psychiatry 57:506–513, 1996
8. Meade CS, Sikkema KJ: HIV risk behavior among with severe mental illness: A systematic review. Clinical Psychology Review 25(4):433–457, 2005
9. Padron, JM: HIV/AIDS/STD/HCV, Coinfection, Seroprevalence and Education in Severe Mental Illness: Health Education Pilot. Psychiatric Quarterly DOI10.1007/s11126-008-9087-x, Spring Science+Business Media, LLC 2008
10. Rosenberg SD, Trumbetta SL, Mueser KT, Goodman LA, Osher FC, Vidaver RM, Metzger DS: Determinants of risk behavior for Human Immunodeficiency Virus/Acquired Immunodeficiency Syndrome in people with severe mental illness. Comprehensive Psychiatry 42(4):263–271, 2001














Why must you use such dreadful language in talking about this topic? Refrring to people with psychiatric labels as “the SPMI community” is incredibly offensive. Calling people who’ve been psychiatrized “seriously and persistently mentally ill” is bad enough – but referring to people by that disgusting acronym is just beyond the pale. There’s no evidence that extreme mental and emotional states are caused by an “illness” and you insult all of us by treating the politically charged and completely invented categories in the DSM as fact. I’m just appalled that your blog appears on this site!
Report comment
Thank you for using acronyms such as SPMI. We want the public to know that “mental illness” is now serious and quite persistent with worsening outcomes over the long term thanks to the use of psychiatric drugs!
Report comment
I skimmed this article. However I ran an LGBT group at my local day centre (great fun, very bitchy and rude in an amusing manner!) and I thought there was a lot of people attending considering the number of people who attend the day centre. I then researched the number of LGBT with serious mental distress – it is high – Mr Richard Bentall, psychologist and researcher into the social causes of mental distress, said the LGBT community had twice the rate of psychosis as the heterosexual community.
So I asked my group a series of amusing questions to break the ice and help people get to know each other, including, “How Queer are you?” and, “Have you had sex or a relationship with someone madder than you?” (well I was going for the outrageously provocative, I make no excuses, and it was amusing). I was expecting interesting and witty answers, which I got, but I also discovered that sex in hospital is not that unusual. I later discovered that sex in hostels and sheltered housing is not that unusual either. My conclusion was that safer sex materials (condoms, lube, educational leaflets) should be available on wards and in supported accommodation preferably distributed by in your face drag queens, just like there were on the doors of nightclubs at the height of the aids crisis. I also think that if people do not have individual bedrooms in hospitals that private, bookable areas for intimacy between residents should be available.
I hope this is provocative, but also realistic. People often meet partners in hospital and promoting healthy relationships, both psychological and physically, should be part of rehabilitation.
Report comment