A new study tracks the approval of the latest antidepressant, vortioxetine, by the Federal Drug Administration (FDA) and the European Medicines Agency (EMA). The analysis demonstrates how current regulations fail to protect the public from unsafe drugs and how “economies of influence” conspire to “produce evidence-biased—rather than evidence-based—medicine.”
“How could the FDA and EMA approve a new drug that appears to be less effective than other available antidepressants, and which failed to be more effective than placebo in a substantial subset of trials?” the study authors, led by Lisa Cosgrove, write in Accountability in Research.
“The short answer is that regulatory standards for efficacy are not as strong as prescribers, or the public may think…”
Cosgrove and her colleagues lay out a process of “ghost management” whereby industry-funded drug trials are written up by medical communication companies, endorsed by academic psychiatrists, and then published in highly regarded journals. The industry-funded trials are more likely to report positive findings than independent trials and academic physicians with financial conflicts of interest are more likely to offer favorable opinions.
This process, according to the new analysis, results in biased research findings and the “marketing of expensive new drugs with questionable risk/benefit profiles” to the public. This problem has been increasingly evident in studies of antidepressants. As we reported at Mad in America, a recent reanalysis of industry trials found that the antidepressant paroxetine (Paxil/Seroxat) is more dangerous for adolescents than previously reported.
“The relationships among academe, publishing, and industry can facilitate commercial bias in how drug efficacy and safety data are obtained, interpreted, and presented to regulatory bodies and prescribers,” they write.
To illustrate how this research bias occurs, Cosgrove et al. use the newly approved antidepressant vortioxetine (Brintellix™) as a case study. The analysis identifies several problems leading to this particular form of research bias. These include weak regulatory standards requiring only statistical and not clinical significance, design flaws limiting adverse reaction data, and a lack of comparisons to current treatments.
“Our analysis suggests that there is a complex interplay among three institutions: the pharmaceutical industry, the medical publishing industry, and the bodies that regulate medical commerce. The legal, accepted, and normative processes used by these societal agencies, when brought together, result in a perturbation that allows a product of questionable benefit to be marketed in several countries.”
Lundbeck/Takeda, the manufacturer of vortioxetine, submitted ten short-term randomized control trials and one long-term trial to the FDA and EMA in an attempt to establish the efficacy of the drug for major depression (MDD). After a review, the FDA found that only six of the short-term trials showed a positive result and then based its efficacy assessment on these six studies.
Cosgrove et al. point out that focusing on the subset of positive trials can inaccurately increase the perceived benefit of the drug and that this inflation of efficacy can be enough to “tip the balance” in the favor of the drug. Neither the FDA nor EMA required that the trials show clinical significance or improvements on functional outcomes, such as returning the work. They also failed to include any comparisons between the new drug and existing options, many of which are available as generics at a much lower cost to consumers.
The analysis is also critical of the methods used in the vortioxetine studies to assess the safety and tolerability of the new drug. Most of the adverse events (AEs) reported in the FDA and EMA reviews were assessed based on spontaneous reports, where patients would be asked “how do you feel?” rather than questioning participants about specific side-effects known to be associated with antidepressants.
For example, sexual dysfunction is frequently associated with antidepressant use and, as the researchers point out, “relying on spontaneous reporting of sexual difficulties is a good way to ensure that the number of AEs related to sexual dysfunction is low.” In the trials that did attempt to assess sexual dysfunction, the studies used a tool (the Arizona Sexual Experiences [ASEX] scale) that had questionable validity and yielded data from which it is “impossible to draw any valid conclusions about treatment-emergent sexual side-effects.”
All of the trials for vortioxetine were sponsored by the manufacturer, as is typical for new drugs, but, what is even more problematic, is that “every author in all of the published short-term RCTs, as well as one longer term randomized drug withdrawal study, had significant commercial ties to the manufacturer, well beyond research funding.”
According to Cosgrove and her colleagues, vortioxetine offers a case study that shows how “the design choices, interpretive strategies, and rhetorical devices employed by researchers with industry ties and published in journals with commercial ties give the reader the impression that a ‘new’ antidepressant is safe and well tolerated, when in fact the data were not collected or analyzed in a way that provides sound empirical support for this conclusion.”
*
Cosgrove, L., Vannoy, S., Mintzes, B., & Shaughnessy, A. F. (2016). Under the Influence: the Interplay among Industry, Publishing, and Drug Regulation. Accountability in Research, (just-accepted).
Disclosure: Justin Karter is a volunteer researcher in psychological ethics with Lisa Cosgrove at UMass Boston. His involvement in the research being summarized here was limited to citation management and manuscript preparation.















It’s shameful that his article is behind a paywall costing $41.00 to read the single article. Most new books don’t cost half that much.
If this information can benefit the public, the authors should make it available for free or at much lower cost – at most $5 or $10.
Ironically, Mad In America recently made their readers aware of an illicit website which allows internet users to illegally download journal article such as this one for free online. Now let me think… will I waste $41 on this article… or will I illegally get it for free…
Report comment
Wouldn’t want to leave fellow MIA readers high and dry..
http://bigthink.com/neurobonkers/a-pirate-bay-for-science?utm_source=Big+Think+Weekly+Newsletter+Subscribers&utm_campaign=781ca8a9c6-Big+Think+Newsletter+-+0217%2F1218&utm_medium=email&utm_term=0_6d098f42ff-781ca8a9c6-40808573
and the MIA article that linked to it…
http://www.madinamerica.com/2016/02/meet-the-robin-hood-of-science/
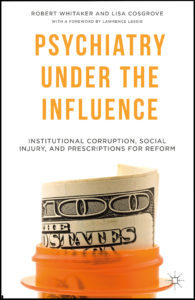
How ironic that the author of this massively overpriced journal article was the coauthor with MIA’s founder, Whitaker, on Psychiatry under the Influence…
Report comment
I agree, it is a shame we can’t read the article. Well, my library probably could get it for me for free, from a local university, but that is a hassle. And it is curious why this type research should not be made available to all for free, strikes me it’s information of import to all of humanity. Especially, since it’s my understanding the authors of the article don’t get paid for having this published, it’s just the publishers that reap the benefits of these pay per view articles.
Report comment
Well, now it appears that the MIA article has been rewritten to give more of a sense of what the full article is actually about… thanks Justin.
Nevertheless, these journal-publishing companies act like legalized cartels or highway robbers, controlling the flow and accessibility of information, and seeking to bilk universities, students, and the publics of massive amounts of money. This is why, if I am interested in reading something, I now only download such articles illegally (the preferred option) or if that fails, beg the researcher to give it to me for free, or if that fails, forget about it. This is the best response to Elsevier and their ilk; don’t buy from them.
I don’t know how the money flow works in terms of what the publisher gets vs what Cosgrove and the other authors get. In this era of increasing inequality, I suspect that much of the money from such an overpriced piece flows to the owners of the journal-publishing company, and relatively little to the actual authors.
Report comment
That’s my understanding. It’s so bizarre, I never expected to have, as enemies when I grew up, large corporations and industries. But our government, whose job it is to prevent and break up monopolies and oligopolies, has instead been taken over by people who seemingly have grandiose goals of global control. While neglecting to do the job they were actually elected to do, which is to properly manage this country. The monopolies and oligopolies need to be broken up, and we need to bring back competition to this world. Living in a world run by psychopathic corporations is not human friendly.
https://www.youtube.com/watch?v=Z4ou9rOssPg
Report comment
This is one more clear reason why we need to overturn Citizen’s United. Our government (and our science) has been undermined by the very corporate interests it must oversee. Bernie Sanders speaks about this frequently. We must insist in resuming control of our democracy and keep full integrity in public safety and science…we obviously no longer have real “science” or oversight we can trust!
Report comment
You know, it almost seems as if the drug companies don’t even try to hide the corruption anymore. “Every author had significant commercial ties to the manufacturer.” And then it says that these concerns are well beyond research funding. The drug companies just expect that the FDA will give them what they want and they’re right. So now GP’s will be pushing another useless so-called “antidepressant” on people who come in to see them. I wonder how much this one costs?
Report comment