According to a recent study published in the journal Psychiatric Services, black patients are almost twice as likely as their white counterparts to be diagnosed with schizophrenia, while white patients are significantly more likely to receive a diagnosis of anxiety or depression. The researchers also found that the likelihood of receiving psychotherapy for any diagnosis (34%), regardless of race or ethnicity, was much lower than the probability of receiving a psychotropic medication (73%).
The researchers, funded by a grant from the National Institute of Mental Health (NIMH), looked at data on the diagnoses, psychotropic prescriptions, and psychotherapy records of over 7.5 million patients within the Mental Health Research Network. This study is an especially important addition to the literature as it uses health care records rather than surveys and self-reports, while also including a large, geographically and racially diverse representative sample of the population.
The data revealed that White patients were diagnosed with psychiatric conditions at a higher rate (19.8) than Black (13.5), Hispanic (14.3), and Asian (7.5) patients. Native American and Alaskan Native patients had the highest rate of any diagnoses (20.6).
The researchers also found that white patients were significantly more likely (77.8 percent) to be prescribed psychotropic drugs than non-white patients. There was also some evidence that black patients were over two and a half times more likely to receive psychotherapy for a schizophrenia diagnosis than white patients, but the overall rate of psychotherapy was so low that it’s hard to determine clinical relevance.
While the data from this study does not reveal why these racial and ethnic differences in diagnosis persist, the authors point to previous research that reports that health care providers presented with the same symptoms are more likely to diagnose black patients with schizophrenia or bipolar disorder, while white patients are more likely to receive a diagnosis of major depression.
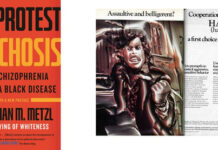
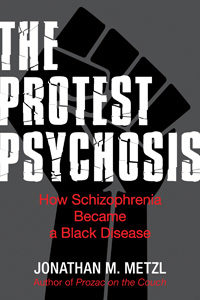 In 2010, the sociologist Jonathan Metzl wrote “The Protest Psychosis: How Schizophrenia Became a Black Disease,” detailing the dramatic racial and gender bias in people diagnosed with schizophrenia during the 1960s. In reviewing the charts from the Ionia State Hospital for the Criminally Insane in Michigan, Metzl found that in the fifties, schizophrenia was used as a label to explain why some women were unable to perform their expected roles as mothers and wives, but in the 1960s, during the civil rights movement, the diagnoses switched to apply to African American men from Detroit who presented with “paranoia against police.”
In 2010, the sociologist Jonathan Metzl wrote “The Protest Psychosis: How Schizophrenia Became a Black Disease,” detailing the dramatic racial and gender bias in people diagnosed with schizophrenia during the 1960s. In reviewing the charts from the Ionia State Hospital for the Criminally Insane in Michigan, Metzl found that in the fifties, schizophrenia was used as a label to explain why some women were unable to perform their expected roles as mothers and wives, but in the 1960s, during the civil rights movement, the diagnoses switched to apply to African American men from Detroit who presented with “paranoia against police.”
* * * * *
For more on racial biases in psychiatric diagnoses, see Twilah Hiari’s recent blog “Mental Health in Black and White.”
* * * * *
Coleman, K.J., Stewart, C., Waitzfelder, B.E., Zeber, J.E., Morales, L.S., Ahmed, A.T., Ahmedani, B.K., Beck, A., Copeland, L.A., Cummings, J.R. and Hunkeler, E.M., 2016. Racial-Ethnic Differences in Psychiatric Diagnoses and Treatment Across 11 Health Care Systems in the Mental Health Research Network. Psychiatric Services. (Abstract)















So has “schizophrenia” become the new “drapetomania”?
Report comment
All these labels have social purposes in terms of controlling and corralling people, similar to drapetomania.
Behavioral geneticists would probably suggest something racist like black people evolved to have more schizophrenia.
What a harmful word “schizophrenia” is when used to mean an incurable disease, i.e. when it’s used by psychiatrists.
Report comment
We should hope they aren’t racial, because the Irish have the world’s highest national schizophrenia syndrome rate. Does this mean that Celtic people whose last name begins with “O” comma are going to give us all schizophrenia through interbreeding?
Report comment
Don’t worry, the genetic connection is spurious.
Report comment
I hope the writer got that study right, because he got the hospital wrong. He’s talking about the Ionia (not Iona) State Hospital in the southwestern part of the state (between Lansing and Grand Rapids). Ionia is Michigan’s Prison City, it’s economy dependent on the activities of the state Dept. of Corrections, which has several facilities there. As far as I know, there is no Iona in Michigan, but then I’ve only lived there 70 years.
Report comment
Did we have members of the staff of the Serbsky Institute emigrate here in the 1960’s or did we just slavishly imitate that institution’s and the KGB’s diagnostic techniques?
Report comment
In both cases, ideological and public-political factors played a major role in the diagnosis.
Report comment
To me…”schizophrenia” is a way of saying: you’re not a member of the community. You are the Other. In my own life, I’ve been diagnosed as Bipolar I by doctors who had an interest in seeing me do things. “Schizophrenia” has been slapped on me by doctors who sought only to invalidate me and control me.
Not that being “Bipolar I” is ideal, but…I read “Bipolar I” as meaning you’re still in the human race, albeit barely. “Schizophrenia…” not so much.
My personal suspicion is that a lot of this is more social class than race per se. The lower status you are, the worse your diagnosis (and prognosis).
Report comment
We should also not overlook the finding that 73% of clients were offered drugs, while only 34% were offered psychotherapy. This belies the claim that drugs are only being used on “endogenous” conditions that are not based on external circumstances, as the figures on traumatized individuals with “mental health” diagnoses show the rate to be in the 80+% range at least. It shows that drugs have become the first-line intervention regardless of the cause of a person’s distress.
Report comment
What’s strange is that drugs were given more to white than to Black people. Seems like it would be the other way around.
Report comment
I think it’s because white folks, on the average, are more likely to grant that “s/he’s the doctor and must know what s/he is talking about” while black people are more likely to be suspicious of powerful white folk giving them drugs to make them more accepting of the status quo.
— Steve
Report comment
I believe that when it comes to involuntary treatment, the shoe is on the other foot.
— Steve
Report comment
Does anyone have a link to a study that gives info on racial, ethnic, gender, age, etc. statistics among treatment providers? Searches usually lead to info on patients, but there doesn’t seem to be any on treatment providers, so we have to guess and make assumptions. Seems to me like that info would be important.
Report comment
Issues like these need to be studied but it’s also important to keep in mind that the larger issue is that mainstream treatment of schizophrenia tends to be iatrogenic (i.e. makes things worse)…it’s not implicitly racist to diagnose African-Americans with higher rates of a mental disorder, every “demographic” lives under somewhat different conditions in general and therefore can be expected to respond and cope differently with their lives…if psychiatric care were truly enlightened, the subtext of this headline would be that blacks are *privileged* compared to other ethnoracial groups when they meet with a psychiatrist.
Report comment