A new study, published open-access in the latest issue of PLOS One, surveys German physicians concerning their understandings of the well-documented placebo and nocebo effects of antidepressant drugs. The study finds that most doctors endorse the effectiveness of antidepressants while acknowledging that placebo effects may account for a significant share – around 40% – of symptom improvement.
“Overall, the findings suggest that the majority of physicians is generally aware of placebo and nocebo effects in antidepressants caused by psychological factors such as expectation and experience from patient and–to a lower degree–physician,” the authors write. “However, these effects are given a subsidiary role when compared to pure pharmacological effects.”

In recent years, researchers have paid increased attention to placebo and nocebo effects in medical research. Placebo refers to the positive effects a drug has that are not directly related to its pharmacological properties. “Non-specific” factors, such as patient and doctor expectations, have been shown to have an important and measurable impact on different symptoms. These same factors can also have negative or nocebo effects on individuals, however, when expectations and contexts lead to unwanted side-effects.
Past studies have suggested that placebo accounts for up to 75% of antidepressant effects, but psychiatrists and other physicians attribute only 26% of their success to these nonspecific factors. It is perhaps telling, however, that in past surveys 38% of psychiatrists admitted to prescribing sub-therapeutic doses – or doses lower than believed necessary to have an effect – of antidepressants. The researchers suggest that the underlying aim in these instances would be to induce placebo effects.
To explore physicians beliefs about the nature of placebo and nocebo effects for antidepressants, the authors of this study recruited 146 doctors, and 87 completed an online questionnaire. The majority of these were specialized physicians, and about 40% of these were psychiatrists.
Nearly 90% of those surveyed reported believing that antidepressants to be effective and only one physician rated them as largely ineffective. Using a rating slider, each doctor was asked to estimate the percentage of total effectiveness they attributed to pharmacological effects, patients’ expectations, patients’ former experiences, the physician-patient relationship, physician expectations, and spontaneous remission.
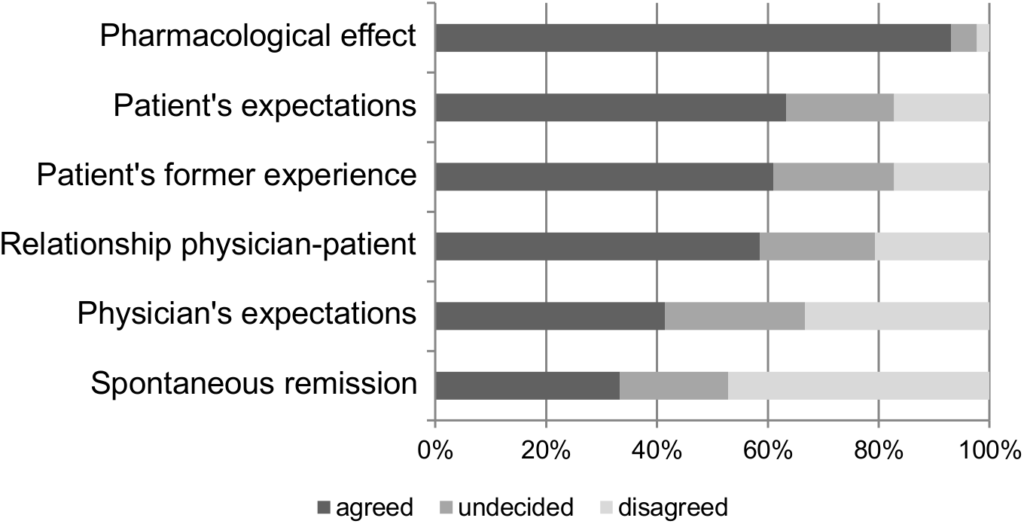
Depicted is the percentage of participants who agreed, disagreed or were undecided whether they agreed to the suggested mechanisms of efficacy for antidepressants
As the figure demonstrates, 93% of physicians believed pharmacological effects were most significant. Additionally, close to two-thirds felt that patient’s expectations and patient’s former experiences were important.
To a lesser extent, physicians acknowledged the various ways their own roles impacted antidepressant effectiveness. 58.6% recognized that the relationship between the doctor and patient played a role and 41.4% of the physicians knew their own expectations as a possible mechanism of effectiveness.
Only one-third of the physicians, however, reported that spontaneous remission of depressive symptoms could contribute to the perceived effectiveness of antidepressants. In contrast, a 2013 meta-analysis found that 23% of prevalent cases of untreated depression will remit within three months, 32% within six months and 53% within twelve months.
When comparing the relative importance of these different factors on overall effectiveness, “physicians’ endorsement of the pharmacological explanatory model succeeded nonspecific factors substantially, as the vast majority of physicians agreed to the pharmacological effect of antidepressants and attributed more than half of overall effectiveness to it.”
The researchers point out that doctors underestimated the placebo effect of antidepressants compared to results from research trials. They explain:
“[Antidepressant] contribution is rated lower than evidence-based data synthesis from clinical studies with placebo arms suggest (39% in our study vs. 68–75% in meta-analyses. Although these meta-analyses are based on placebo administration instead of placebo effects within the application of active drugs, we consider it a helpful benchmark to frame the estimation of nonspecific mechanisms of efficacy in our sample.”
The pattern for nocebo effects was similar. Physicians attributed unwanted side-effects primarily to the pharmacological properties of the drug. Patient expectations and past experiences also acknowledged, with close to 60% endorsing these factors.
In summary, the researchers write:
“Ninety percent of the participants endorsed the general effectiveness of antidepressants. Thus, this study documents physicians’ general belief in the benefits of antidepressant treatment. The physicians’ explanatory models for antidepressant effectiveness showed clear favors towards a pharmacological factor. Beyond this, the majority of the participating physicians were aware of the importance of placebo effects in antidepressant effectiveness. They stated their belief in psychological factors such as the patient’s expectations and prior experience, as well as the patient-physician-relationship. However, they did not equally acknowledge the importance of physician’s own expectations.”
****
Kampermann, L., Nestoriuc, Y., & Shedden-Mora, M. C. (2017). Physicians’ beliefs about placebo and nocebo effects in antidepressants–an online survey among German practitioners. PloS one, 12(5), e0178719. (Full Text)















We know that in some trials, sleeping pills or tranquilizers are available to patients who experience insomnia and anxiety while taking the antidepressant under investigation. Are relaxing drugs only available to the drug group, or do placebo patients get them, too? They would almost have to, or the double-blinding would break. If placebo patients have access to sleeping pills and/or benzos, of course they’ll feel better than they did before. And on the HAM-D depression scale at least, there are a lot of questions about sleep. If sleep is no longer a problem, HAM-D scores will improve, regardless of mood and motivation.
Report comment
So, what’s ironic is we know the medical community is deluded about the placebo and nocebo effects of the antidepressants, but we also know the medical community thinks all people who are “delusional” need to be defamed and tortured forever with the psychiatric drugs. Might this not be problematic for such hypocrites some day?
Report comment