A new study conducted by China Mills and Eva Hilberg in the UK carefully examines the mhGAP Intervention Guide technology launched by the World Health Organization (WHO). The paper reviews the development and implications of the WHO mental health technology alongside historical colonial practices and current-day movements for Global Mental Health. Mills’ and Hilberg’s analysis allows for entry into dialogue with the WHO and presents essential critiques about the mhGAP technology.
“This study aims to extend and somewhat disrupt the ‘official’ story that is told by the WHO about mhGAP-IG by making a first step in tracing its ‘social life,’ they write.
“The analysis throughout this study was written in the spirit of engaging in dialogue with the WHO. We argue the importance of paying closer attention to the epistemological underpinnings of mhGAP-IG’s algorithmic imaginary, in order to open the ‘black box’ of its production. An important element in this process is to take seriously the critique of mhGAP-IG both from within its own paradigm and from other epistemological standpoints, particularly the multiple perspectives of and critiques from what might broadly be termed user/survivor/ Mad, as well as situated, localized and indigenous, epistemologies.”
The WHO’s mhGAP Intervention Guide is an algorithmic, evidence-based tool designed to streamline detection, diagnosis, and management of common mental health disorders. The program from which it was based, the mhGAP program, was launched in 2008. Its overarching mission has been to close the “treatment gap” and promote access to mental health services, particularly in low- and middle-income countries. In 2010, the mhGAP Intervention Guide (mhGAP-IG) was developed out of this mission.
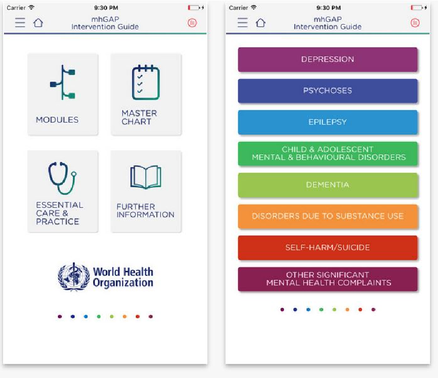
The mhGAP-IG is a tool designed specifically for the use of non-mental health specialists. As of 2016, this tool is available as a smartphone application. Proponents of the Global Mental Health movement have argued in favor of its usage in all countries and health sectors as the standard approach. The guide provides a flowchart for doctors, nurses, and other non-mental health specialists to conduct a “simplified clinical assessment” designed by an algorithmic protocol. Already, mhGAP-IG has been used in over 80 countries and translated into more than 20 languages.
Given its global significance, the authors explain their choice to delve further into examining how mhGAP-IG came to be produced, the methodologies and assumptions about mental health that form its foundation, how it is used globally, by various actors, and finally, its implications:
“As algorithmic tools become an increasingly common state of the art, and given the global significance of the mhGAP-IG, it is important to question the conditions of production of these tools and guidelines, their underlying theories and assumptions about mental health, and how the kinds of knowledge that they create have implications for the governance and experience of mental health globally.”
Importantly, the mhGAP-IG was designed for global expansion, write Mills and Hilberg. The consequences of this are explored by drawing from postcolonial and feminist analyses of technology, mainly how tools can be used to privilege some forms of knowledge while marginalizing others. They write:
“The mhGAP-IG does not operate in a vacuum and its historical conditions of possibility are ‘alive’ in the present. Therefore, these histories and the wider global assemblage of mental health in which mhGAP is embedded are woven throughout the analysis, which focuses on how mhGAP-IG is made and how it is performed across different sites.”
First, the production of mhGAP-IG’s and its value are built upon the notion that a treatment gap exists and requires closing. Yet, the sense of urgency to close this gap is constructed, argue Mills and Hilberg, and it is done so based upon disease burden estimates. Disease burden estimates are statistical calculations built around biomedical definitions of mental disorders. They attempt to quantify prevalence, mortality risks, and economic costs and returns associated with investing in mental health treatment. These estimates have been strongly critiqued. Mills and Hilberg summarize:
“Some critique the WHO’s ‘use of alarming statistics’ as being too heavily biomedical and overly focused on ‘treating individual conditions’, paving ‘the way for further medicalization of global mental health.’”
In addition, critiques have been made surrounding the cross-cultural validity of the diagnosis, overreliance on psychotropic drugs, marginalization of grass-roots approaches, and the construction of mental health as a “technical problem of delivery of services.”
Assumptions underlying the mhGAP-IG, therefore, include the view that mental “illness” is universal, commensurable and measurable, and measurable through metrics that understand distress as chronic, disabling, burdensome, and treatable through mental health intervention.
Notably, Mills and Hilberg highlight that the construction and development of mhGAP-IG occurred without service-user involvement. Priority conditions were identified first. That is, mental disorders “identified on the basis of high mortality and morbidity, high economic costs or association with violation of human rights within the area of MNS disorders.” These included depression, schizophrenia, and other psychotic disorders, suicide prevention, epilepsy, dementia, disorders due to the use of alcohol and illicit drugs, and mental disorders in children.
Following this, systematic review procedures and evidence-based interventions were drawn upon to form the basis of the mhGAP-IG technology. The authors draw on the work of Alice Cooper to discuss the ways that qualitative data and other aspects of social life are elided when inclusion, justified as rational and scientific, is based around reduction, standardization, and prediction of data. They write:
“By setting the parameters of what counts as evidence, and not including users and survivors in the early formulation of mhGAP, the makers of mhGAP-IG craft the epistemological parameters of critique for the guidelines, excluding alternative conceptualizations from different worldviews of distress (such as different cultural understandings and/or user/survivor/Mad epistemologies).”
Mills and Hilberg discuss to the explicit intention for mhGAP-IG to promote expansion via globalization. Author, China Mills, attended the 2017 mhGAP forum. Implementation and training were seen as a critical step toward the aim of expansion and scaling up.
Additionally, technologies such as mhGAP-IG provided a means with which to do this. Mills and Hilberg explain further that the features of the app:
“The app, like the mhGAP-IG, uses an assessment algorithm of yes/no answers to produce suggested treatment outcomes which vary from psychoeducation to psychopharmaceuticals. However, the app is not simply a digitized version of the IG, it also ‘adds value’ through a note-taking and feedback function, which tracks previous answers, meaning it can be used as a learning tool and has the potential to link to electronic health records.”
Yet, this prescriptive tool leaves little room for local understandings of distress. In this way, a tension between the local and the global underlies the mhGAP-IG. Although country-specific versions of mhGAP-IG have been constructed, they rely largely upon adapting and customizing the app’s functions to different health systems and training models. As Mills and Hilberg write, this adaptation does not take into account the way that localized understandings and practices might disrupt or diverge from the logic, particularly around universality, that lays the foundation for the app and its mission.
Furthermore, the mhGAP-IG is constructed around ICD diagnostic conceptualizations of distress, which were developed within the context of expansion and colonization, argue Mills and Hilberg. They write:
“… Expansionary logic (including the conceptualization of mental disorders as universal and the desirability of uniformity in usage globally) was built into diagnostic criteria from its early formulations, thus making mhGAP-IG thinkable and do-able. In fact, psychiatric classificatory systems, and the imaginary of what is now known as ‘mental disorder’ as being universal date back further than the beginnings of the DSM, ICD, and cybernetics. ‘Colonial political arithmetic’ was a critical component of colonial biopolitics, where invasive investigations of poor people, ‘lunatics’ and criminals carried out domestically were transposed to whole populations of the colonies.”
Finally, mhGAP-IG functions as an “inscription device,” the authors contend. Inscription devices are described as those that inscribe subjective decisions while simultaneously rendering the process by which they came about as hidden. In this case, the nature of mhGAP-IG’s development and its underlying assumptions, such as its reliance on diagnostic criteria, are concealed. A result of this is that these processes come to be viewed as a technical matter, and important considerations such as implications around discriminatory practices and the “funding architecture” of the project remain invisible. Mills and Hilberg write:
“This process of black boxing should be of importance to the WHO as it goes against its stated aim of eliciting feedback for its mental health products.”
Overall, this study has delineated that mhGAP-IG and its diagnostic underpinnings originate out of a history of measuring mental health, a practice developed within colonial and expansionary initiatives. Mills and Hilberg conclude:
“This study has marked a starting point in tracing the multiple ‘doings’ of mhGAP-IG – connecting questions of how it is ‘done’ and what does it ‘do’ – to the living histories and wider global mental health assemblages that make the tool possible and shape its global circulation.”
****
Mills, C. & Hilberg, E. (2019). ‘Built for expansion’: the ‘social life’ of the WHO’s mental health GAP Intervention Guide. Sociology of health & illness, 41, 162-175. (Link)















This isn’t, I’m afraid, a very helpful comment, merely a note about the use of words. Far too many studies, particularly those in the categories of psychiatry and mental illness, use the word “critique” instead of the correct word “criticism”.
A critique is a wide ranging review of something, usually by an acknowledged expert in the field of that something, who has a detached but informed overview.
A criticism, on the other hand, is a specific negative comment about a specific thing which the person making the criticism does not agree with.
(I do not include Literary Criticism in this, which is an entirely separate subject)
A well known film critic writing about a new release, for example, will write a critique of that film and it will be published in whichever journal he writes for. He has critiqued the film.
Whereas:
A qualified social worker, reading a draft report into adoption, finds a statement with which she wholeheartedly disagrees – and has evidence to support that – will make a criticism about the statement. She has criticised the statement.
Sorry about this. It is really important to use correct wording.
Report comment