New research reveals that individuals seeking depression treatment may benefit from an explanation of depression as serving an important human function, as opposed to a disease arising from genetic and environmental risk factors.
The study, published by Hans Schroder and colleagues in Social Science & Medicine, investigates the effects of different messages of depression etiology on participants’ beliefs about depression, attitudes toward treatment, and self-stigma. Findings from the randomized controlled trial indicate that the message invoking the language of depression as serving an important function leads to more adaptive beliefs about depression and lower levels of self-stigma.
Messages that describe the chemical and genetic basis of depression, such as the disproven serotonin imbalance theory, have dominated clinical, public health, and popular discourses since the 1960s. Authors of the present research highlight multiple movements that have contributed to the pervasive popularity of biogenetic messages about depression, including direct-to-consumer advertising from pharmaceutical companies marketing SSRIs, public health campaigns showcasing depression as a medical disorder necessitating treatment, and technological advancements in research investigating the neuroscientific and genetic bases of mental health.
Researchers highlight a multitude of unintended iatrogenic consequences of biogenetic explanations of depression, including the implicit activation of biases and stigmatizing attitudes:
“For instance, biogenetic explanations exacerbate other forms of stigma, including reduced hope for recovery (prognostic pessimism), increased perceived dangerousness, and a greater desire to keep distance from those who suffer from mental health problems,” the authors write.
“Two studies of psychiatric patients in treatment show that biogenetic beliefs are uniquely related to poorer expectations… Experientially, invoking genetic and biochemical language undermines important aspects of recovery, including worsening some forms of stigma and reducing hope, curiosity, and introspection.”
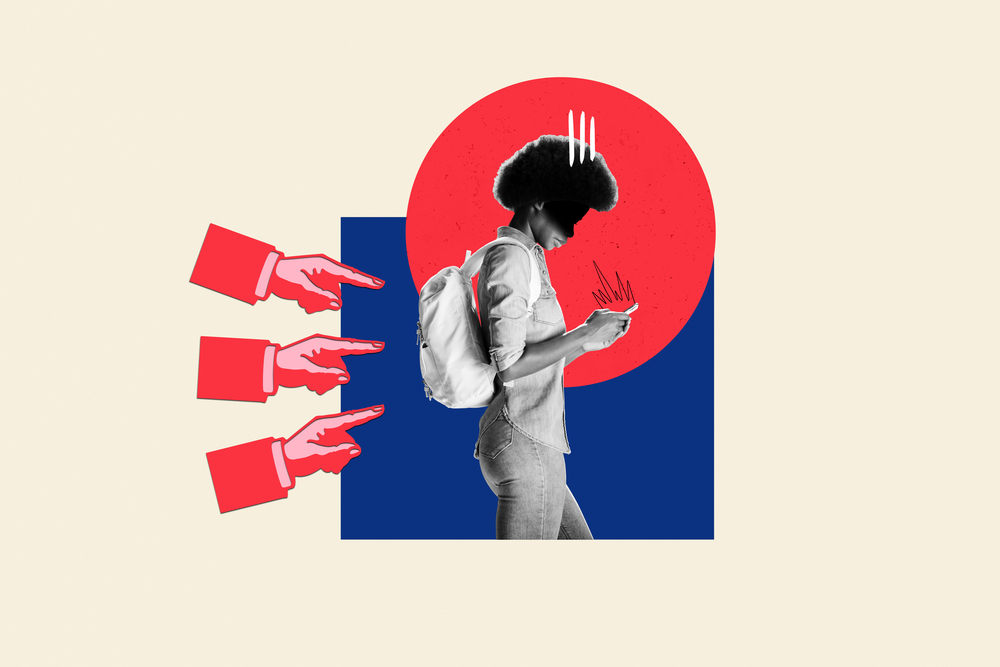 When we learn that a certain behavior or trait is linked to genetics or brain biology, we often fall into a thinking pattern known as genetic essentialism. This is the idea that the behavior or trait comes from a hidden, fixed, and unchangeable core within a person. This way of thinking influences how we see things, like whether we believe a person’s behavior can be changed. Such beliefs can also make us put people with depression in a separate group. This can lead to an “us versus them” mindset among patients, the general public, and healthcare professionals, making people more likely to stigmatize those with depression.
When we learn that a certain behavior or trait is linked to genetics or brain biology, we often fall into a thinking pattern known as genetic essentialism. This is the idea that the behavior or trait comes from a hidden, fixed, and unchangeable core within a person. This way of thinking influences how we see things, like whether we believe a person’s behavior can be changed. Such beliefs can also make us put people with depression in a separate group. This can lead to an “us versus them” mindset among patients, the general public, and healthcare professionals, making people more likely to stigmatize those with depression.
The biopsychosocial (BPS) model of depression is one alternative framing of depression that describes it as arising from the interaction of biological, environmental, and psychological risk factors. While this model is gaining popularity in clinical settings, it continues to emphasize the importance of genetics and, in doing so, may, at times, undermine the social and psychological components of depression.
Schroder and colleagues draw upon evolutionary-based perspectives and evidence from epidemiological data and social cognition research to support an alternative message that depression serves an important function.
The authors suggest that focusing on messages highlighting how traits, emotions, and skills can change and adapt helps people build resilience. This comes from research into how we think socially, which has identified some beliefs that help us adjust our attitudes and keep motivated when dealing with stress and challenges.
These ideas are especially noticeable when we look at ‘growth and stress mindsets.’ A ‘growth mindset’ is when someone believes personal qualities can be developed, not just stuck the way they are. A ‘stress mindset’ is when someone believes that stress can actually have some positive effects.
In their research, the authors found two main things. First, they discovered that people who believe that emotions can change and are helpful show differences in their symptoms, how they manage their feelings, and their choices for treatment. Second, when people are given messages encouraging them to see traits as changeable and valuable, it can lead to better mental health.
In this first attempt to examine the impact of the message of depression as a functional signal, 1698 individuals with a self-reported history of depression but no treatment history (i.e., no prescribed medication or psychotherapy attendance) were recruited via an online market-research firm and enrolled in a randomized, controlled simulation trial.
All participants were asked to imagine attending an initial telehealth appointment with a clinical psychologist for depression treatment. Participants were then shown a series of videos. All participants viewed the same initial video introducing the psychologist and describing the symptoms of depression.
Then, participants were randomly assigned to view three additional videos further explaining the etiology of depression as either a functional signal alerting an individual that something in their life needs attention (Signal condition) or a disease similar to cancer or diabetes resulting from the interplay of behavioral, environmental, and biological risk factors (Biopsychosocial Risk Factor; BPS-RS condition).
Lastly, all participants watched the same final video describing their depression treatment options. After viewing the videos, participants completed measures to assess their beliefs about depression, treatment-seeking attitudes, and self-stigma.
Participants’ data were excluded from analysis if they did not pass necessary attention checks to ensure that they watched all videos or if they completed surveys in less than 5 minutes. Therefore, the final sample included in the analysis consisted of 877 participants: 432 in the Signal Condition and 445 in the Biopsychosocial Condition. The sample was predominantly (71.2%) White or European American, and the majority (63%) female.
Videos in both conditions were closely matched across multiple elements (i.e., introductory and closing video, actors, video duration, sentence structure, and reading level). Additionally, given previous literature showcasing that biogenetic explanations of depression may be correlated with decreased patient self-blame, videos in both conditions included explicit statements of “depression is not your fault.”
Results of the present study indicate that participants in the Signal condition endorsed greater depression offset efficacy (i.e., sense of autonomy and agency in overcoming their depression), less self-stigma, and more adaptive beliefs about depression (e.g., “Experiencing depression can lead to new insights”) compared to participants in the BPS-RS condition. There were no significant differences between the two conditions regarding participant growth mindset, feelings of personal responsibility for depression onset, or attitudes toward depression treatment.
Researchers conducted follow-up exploratory analyses to examine whether the intervention had any differential impacts on male and female participants. Results indicated that amongst male participants alone, conditions differed only on the adaptive beliefs about depression measure, such that those in the Signal condition endorsed more adaptive beliefs than those in the BPS-RS condition.
However, amongst female participants alone, four measures were significantly different across conditions, suggesting that depression offset efficacy, growth mindset, and adaptive beliefs were higher, and self-stigma was lower amongst women after undergoing the Signal condition. Consistent with full sample results, there were no differences amongst women in the two conditions on measures of treatment attitudes and depression onset responsibility.
Exploratory gender analyses suggest that the Signal intervention had a stronger impact on female participants than on males. Authors suggest that women may be more receptive to the signal framing of depression as a welcome counterpoint to pervasive biogenetic messages that essentialize depression as inherently tied to female bodily experiences (e.g., menopause, childbirth, hormonal changes).
Findings from the present study provide preliminary support for the notion that a functional framing of depression may be preferable over the traditional disease-based biopsychosocial approach. Results point to the positive impact of a functional framing on enhancing one’s sense of agency in autonomy in overcoming depression without simultaneously increasing a sense of personal responsibility or self-blame. Moreover, findings suggest that public health campaigns aimed at reducing stigma may be more effective if they present depression as a normal, functional aspect of the human experience rather than a medical disorder.
The authors note the need for future research to expand upon present findings by exploring how signal-based messages about depression vary by sociocultural characteristics not captured or analyzed in the present study, including gender identity, race, ethnicity, socioeconomic status, and sexual orientation.
The present study was the first to test the novel framing of depression as a functional signal rather than a disease in a randomized controlled trial. While preliminary findings show promise in the impact of the alternative frame on reducing self-stigma, promoting a greater sense of agency in overcoming depression, and increasing adaptive beliefs about depression, more longitudinal research is needed to determine whether these positive outcomes persist over time.
Researchers leverage the present study findings to advocate for more expansive and nuanced approaches to discussing the causes and treatment of depression and to developing public policies:
“From a public health perspective, viewing depression as a signal, rather than a biogenetic disease, may spur a call to action for more funding for preventive actions that deter the signal of depression from occurring in the first place. Of note, despite increases in psychotropic medication usage, the prevalence of depression has not reduced, and in some circumstances, has increased over the last several decades.”
“Implementing policies designed to address income inequality and racial disparities in achievement, housing, and employment would most certainly reduce depression rates in meaningful ways, particularly if depression is viewed as a disease of modernity. Viewing depression as a functional way for the body to face unsustainable environmental stressors may also encourage agencies such as the NIMH to direct some of their funding to these larger-scale issues.”
The present study extends previous literature that has demonstrated that patients who adopt biogenetic theories to explain their depression are more pessimistic and self-blaming and have worse depression outcomes. The current research findings suggest that framing depression as a functional part of the human experience may be a welcome antidote that promotes hope and reduces stigma.
****
Schroder, H. S., Devendorf, A., & Zikmund-Fisher, B. J. (2023). Framing depression as a functional signal, not a disease: Rationale and initial randomized controlled trial. Social Science & Medicine, 115995. (Link)















Depression was more or less invented with ‘Prozac’ in the 1980s. Before Prozac a person would have been ‘laughed’ at for claiming depression.
When a person signs up with a doctor in the UK they are provided with a checklist, regarding possible symptoms of depression. It’s the only nonexistant ‘illness’ that I know of that’s treated like this.
Report comment
In the States, a woman cannot walk into an emergency room – with merely a pulled muscle, albeit right over my heart, so I thought I should just double check – without a random doctor asking, “Are you depressed?”
My response was, ‘No, and I’m allergic to the anticholinergic drugs.’ Thankfully, that aptly named doctor, did run quickly away.
“Findings from the present study provide preliminary support for the notion that a functional framing of depression may be preferable over the traditional disease-based biopsychosocial approach. Results point to the positive impact of a functional framing on enhancing one’s sense of agency in autonomy in overcoming depression without simultaneously increasing a sense of personal responsibility or self-blame. Moreover, findings suggest that public health campaigns aimed at reducing stigma may be more effective if they present depression as a normal, functional aspect of the human experience rather than a medical disorder.”
… statements based upon common sense. But that this is such a great revelation to you, or even needs to be pointed out, Julia, only goes to shed light on how literally brainwashed the future “mental health” workers are, in the universities. And just an FYI, what you call “self-blame,” should be more accurately called psychiatric and/or psychological stigmatization.
Forgive me for being older, hopefully a little wiser, and pointing out common sense … Of course, defaming someone with a “lifelong, incurable, genetic disorder” – with zero proof – is going to lead to poor outcomes. It steals hope from the client and destroys marriages, which honestly, is just downright evil.
And we should never forget, “It is no measure of health to be well adjusted to a profoundly sick society,” since we do live in a “profoundly sick society.”
https://www.wildmind.org/blogs/quote-of-the-month/krishnamurti-measure-of-health
https://www.amazon.com/Pedophilia-Empire-52-book-series/dp/B07THDK6MV
Report comment
This is a step in the right direction but I really think we need quit thinking about mental and physical health as separate entities. What we currently call mental illness is usually just a symptom of your immune system responding to a threat. Just like your body responds to a virus with a fever or a cut with inflammation the same immune system responds to psychological stress with a physical reaction that may include depression, anxiety, or hallucinations.
Report comment
This is where Internal Family Systems really takes things to the next level in my view. It’s wonderful to view depression as some kind of signal rather than being due to a mysterious gene, but the obvious question then becomes “What is it signaling?”. Odds are most people will go right back to cognitive-level talk therapies or simple behavioral changes in an attempt to hunt down the apparent cause.
With IFS however, we work things from the bottom-up by unraveling what’s going on in the unconscious that is bringing on symptoms like depression. The proximate cause is almost always going to be stuff from the past (trauma) rather than anything happening in the present. (Although things in the present can of course exacerbate it.)
Report comment
Well, remember that depression isn’t a disease unto itself, but a syndrome that can come from one or more of mulltiple origins that don’t all have the same treatment. All the treatments in the world aren’t going to be helpful unless they’re matched with the origins that induced the depressed mood(s).
Report comment
When did being human become a disease? When psychiatry began publishing the DSM.
Report comment
I agree that depression–suffering and despair–is part and parcel of what it means to be human. It may even be true that we cannot grow as individuals without such experiences, for better or worse.
That said, I do think there is a point of demarcation between “acceptable” suffering and “pathological”. I do think it probably in some real sense can qualify as a ‘disease’, that is, a physical condition that is ailment not per se axiomatic to existing as a human (that’s a totally shoot from the hip definition of disease, please don’t nitpick!!!). I am not claiming to know where the point of demarcation lies, by any means, but I do think it exists and that treatment can aid in ameliorating it. As for what the ideal treatment is, well, in my experience the only thing that’s ever been helpful–and I’ve tried just about every pharma option on the market (that we must get them on the ‘market’ is an entirely different but important issue)–is therapy with a provider who is knowledgeable, sympathetic and with whom you have a rapport.
I suppose I’m rambling now, but my primary point is: Suffering is part of being human, but there’s a limit its intensity in terms of being normal and not pathological.
Report comment
The question is, how can anyone POSSIBLY determine where such a “line” lies, or if it even exists? And if we DON’T objectively define what it is, then we get arbitrary and subjective rules, leading to “diagnostic drift” toward whatever makes more money for the providers and less trouble for those in control of society’s institutions.
And why do we need to define such a line anyway? Why can’t we simply say that “those who suffer need and deserve support” and provide it without pretending there is something physiological going on? Now, if there IS something physical that is off, like low thyroid, anemia, sleep problems leading to depression or hyperactivity, or whatever, then THAT is what should be treated, not “depression” or “anxiety.”
I’d really be interested in knowing why you think such a line can be and/or needs to be drawn to be able to provide full support to those who are suffering?
Report comment
I will try for a more comprehensive/thoughtful reply later (I’ll probably forget, that’s the nature of the beast) but I just want to quickly say that we should absolutely give full support to anyone who is suffering. I did not mean to suggest otherwise.
Report comment
I agree with you completely. I’m not sure I didn’t know you agreed with me already!
Report comment
What I find depressing is how so many people believe they need “therapy” when all they really need is someone who understands and is willing to listen without judging.
Report comment
Oprah Winfrey has had a book published titled What Happened to You? Conversations on Trauma, Resilience and Healing (along with co-author Bruce D. Perry, MD, PhD). This (or What is happening to you?) is the question people seeking mental health counseling should be asked, in my opinion.
As a piece of graffiti I once saw said, “If you’re healthy and normal in this sick society, just what kind of a person are you, anyway?”
Report comment
The answer lies in reclaiming the narrative away from psychiatry’s destructive “medical model”. And it’s good knowing the right information is getting around.
Report comment
ADAPTIVE RESPONSES are not mental illnesses.
(And way WAY past time to redefine or toss the term “mental illness”.)
As a physically (sleep-deprived) and emotionally stressed (with GREAT insurance!) human being…I found THIS-below- to be the explanation of my ‘state’ when psychiatry & Pharma targeted & exploited ($)
me.
I was wounded; they shaped that suffering into a revenue stream.
“ALLOSTASIS AND ALLOSTATIC LOAD: Implications for Neuropsychopharmacology”
Bruce S McEwen Ph.D
Neuropsychopharmacology
NATURE.COM
MCewen & Stellar’s book is older, longer & more granular….and for the APA members-EVIDENCE-BASED!!…..their fave ‘go-to’ describing the excuses for psychopharma “treatment” and the damages that result. (‘The price of stability, dont’cha’ know”.)
It’s not clear to me why McEwen & Stellar are not cited more often on this forum….particularly their LATER papers published in NIH, NIMH, JAMA, BJM, et al.
As someone who was compelled to understand HOW a malicious entity smothered my life-force like a baby in a crib….THIS was the information that helped me re-build my ‘self’ …. re-asserting my humanity, understanding the organism that houses it….& their relationship.
Report comment
“…re-asserting my humanity, understanding the organism that houses it…& their relationship.”
That’s what true psychic healing is all about.
Report comment
I sometimes (but not always) view depression as the winter of the soul. In winter things crystallise as I retreat into my heart’s cave, things I don’t have time for in the busy-ness of summer. In spring many new beginnings shoot forth, of which only a few make it to summer. And remember even the ice age had it’s thaw.
Report comment
Psychiatry is unable to appreciate emotional nuance. It’s medical model is too anal retentive.
Report comment
What is anal retentive? An extreme need to control the environment or situations.
What is psychiatry? An extreme need to control people in its environment or situations.
Report comment