It’s strange to think it’s been two years since everything changed. What began as a well-intentioned step toward healing became the start of something I never could’ve seen coming. On June 28, 2023, I went in for what was supposed to be a safe and effective treatment called Transcranial Magnetic Stimulation (TMS). I left with injuries that have since shaped every part of my life. TMS flipped my life upside down when it damaged my brain.
What TMS Was Supposed to Be
TMS is often described as a non-invasive treatment that uses magnetic pulses to “wake up” underactive areas of the brain, usually for people with depression or anxiety. It was painted as low-risk and cutting-edge and a final option for those who felt out of options. But here’s the thing: I hadn’t tried psychiatric medication. I wasn’t someone who had “failed” every treatment. I didn’t even test high on the depression and anxiety forms. I was just a person trying to improve my health and trying to make the most thoughtful, least invasive choice I could. I thought I was seeking elevated care when my talk therapist recommended I seek out a psychiatrist. I didn’t know it would lead to a brain injury.

The doctors I trusted made it sound like this could be the thing that helped me become a “better” version of myself. I was told I needed this treatment to improve as a person. To become a better partner. A better future parent. I’d watched the hopeful testimonials, read the success stories, and believed them. Why wouldn’t I?
And the real kicker? The psychiatrist told me that she helped a large military population with this treatment. My husband sat across from the psychiatrist in uniform and I didn’t see the manipulation. Instead, I believed the psychiatrist even more.
But nothing could’ve prepared me for what happened the moment the machine turned on. I still remember that first pulse. My eyes filled with tears instantly and not from emotion, but from pain. Something was wrong. I didn’t have the words for it at the time, but I told the doctor it felt like an 8 or 9 out of 10 on the pain scale. The pain was sharp, overwhelming, and deep. I thought that would mean we’d stop but instead, I was told to keep going.
The Pressure to Say Yes
Before starting, I’d made it clear to the clinic that I couldn’t begin treatment right away because I had a marathon planned and a family trip coming up. Their staff said that was totally fine. But when I arrived for what I thought was a basic mapping session, the technician seemed ready to begin actual treatment on the spot.
My husband and I were taken aback. We brought up the fact that the doctor had pushed for the importance of completing 60 sessions without any interruptions. The tech downplayed it, saying it wasn’t a big deal. Still, we said we wanted to talk to the psychiatrist first.
When she came in, we shared our concerns again. Her answer had changed. Now she was saying a short break was fine. As long as I didn’t go too long between sessions, it wouldn’t ruin the outcome. That wasn’t what she’d said before, but somehow, in that moment, we were convinced. I said yes.
I wish I hadn’t. I didn’t feel ready. But I also didn’t feel like I could say no. Not without disappointing the people in the room. Not without derailing what was supposed to be a hopeful path forward to being a “better” person.
The Mapping Setup: Something Already Felt Off
To find the treatment spot, they taped a piece of paper across my forehead with ribbon-like strips to mark the center line of my head. They were trying to locate the motor cortex which was ideally done by finding movement in my thumb, then placing the treatment coil five centimeters forward from that point.
But they couldn’t find any thumb movement. The only movement came from my ring finger. Even though that’s technically three fingers off from where they were aiming, they used that point anyway.
Day 1: June 28, 2023
I’d been told it might feel like a tap, or maybe like a rubber band snap. Unusual, sure, but nothing alarming. The mapping taps were not comfortable, but I thought if I endured that, I could make it through the next 19 minutes.
But when the machine started, it felt nothing like that. It was sharp and electric like something piercing deep into my skull. It felt like an ice pick slammed by Thor’s hammer. My whole body locked up. I couldn’t speak. My eyes filled with tears almost immediately.
They kept going. The psychiatrist said it would get easier over time. That day, they only used 50% intensity. She mentioned they’d slowly work up to 120%. I just sat there, stunned and silent, for 19 minutes.
When it ended, I barely made it to the car before I broke down. At home, I collapsed into bed. I didn’t eat. Couldn’t think straight. I was drooling, staring at the wall, unsure what had just happened to me. Something in my brain felt different. Not in a good way.
I barely made it through the next day until it was time for the appointment.
Day 2: June 29, 2023
We only went back because we decided we’d leave if they didn’t take me seriously. I explained how painful the first session was. The tech seemed confused, like she didn’t believe me.
They brought someone else in, someone more experienced, they said. She told us she had checked with the psychiatrist and that it was okay to move forward. She adjusted the angle of the coil, lowered the intensity slightly.
But the pain was still there. I sat still, breath held, bracing for each pulse. Afterward, I felt dizzy and disconnected. Like something was missing in my mind. I told my husband it felt like I’d had a lobotomy.
They told us the doctor would be there the next day. I held onto that, hoping for answers.
Day 3: June 30, 2023
The next day, neither the psychiatrist nor the experienced tech was there. A much younger tech ran the session. She barely looked at me.
They handed me a little silk cap, saying it might help with the discomfort. It didn’t. The pain was worse. I cried through the treatment again.
I left feeling angry and confused. I had tried to explain that something was wrong. I kept saying it hurt. But no one seemed to take it seriously. I even thanked them as I left, because I didn’t know what else to do.
Part of me still wanted to believe it might help. I told myself I’d keep going unless it interfered with my marathon or my travel plans.
Then it did.
I showed up to run the marathon that I’d trained for but had to stop. My legs were fine, but my head and neck felt like they were collapsing with every step.
I canceled my trip. The pain wouldn’t let up. I couldn’t even lift my head some days. Even blinking hurt. I stayed in bed, barely able to move, wondering what I’d done to myself.
That’s when it finally hit me: this wasn’t a side effect or a rough start. This wasn’t my body adjusting. Something was seriously wrong. And it felt like it might not go away.
What I Know Now
Later, I found out the psychiatrist wasn’t even in the building during my treatments. She was out of the state. She hadn’t reviewed my case. She hadn’t spoken to the techs.
They lied. She had no idea I was being treated.
This wasn’t just poor communication or a bad experience. It was negligent. It was unsafe. It caused real harm.
TMS injured me. I wasn’t warned. I wasn’t protected. And I wasn’t given the truth.
When Things Started Going Wrong
It wasn’t long after that third TMS session that things really started to go sideways. I had already pulled out of the marathon, and I was hoping things would get better with time. But instead, the symptoms kept piling on. And I honestly didn’t know what to think.
The headaches got worse, the exhaustion was crushing, and even basic things like forming sentences, tracking with my eyes, or walking in a straight line started to feel impossible. Those close to me noticed, despite me thinking I was hiding it. I tried to keep running because my body begged for movement, but with every step I felt like my head was going to explode.
This didn’t feel like a temporary adjustment phase. It felt like my brain was glitching. I slept for the majority of the day despite sleeping long hours each night.
I was in a thick fog. My thinking was slow, and trying to find the right words felt like fighting through quicksand. I didn’t recognize myself.
About two weeks after that last session, someone from the psychiatrist’s office called to schedule a follow-up. I hesitantly agreed to a virtual visit, hoping she’d at least acknowledge that something was wrong. But when the doctor got on the call, she greeted me like I had just finished a regular round of treatments. She asked, “So how are you feeling with the sessions?”
I was seriously stunned. I felt confused. I hadn’t been back since that third TMS session. I answered her questions as she asked and I filled her in on my symptoms and the pain.
Then she said maybe my reaction was just a normal part of the process and that it might “clear up in time.” That was the moment I knew something wasn’t right. It felt like she either hadn’t been told what had happened, or she was just trying to cover up my adverse symptoms.
My husband jumped in and explained everything. Only then did she admit she had no idea I’d stopped coming. She said the staff never passed on any updates and that she’d been out of town with a family emergency.
We chose to believe her. We thought maybe now, with the full picture, we could move forward. We agreed to come up with a plan together. We thought we would have unwavering support.
But in hindsight, that conversation was just the beginning of a much bigger mess. I felt like I was drowning in a sea of people that didn’t understand.
Dismissed and Left in the Dark
This was the point where things took an even more painful turn. I had trusted my psychiatrist to help me through this, but instead of support, I started feeling ignored and brushed off. She answered and checked in, but there was absolutely no urgency to find answers.
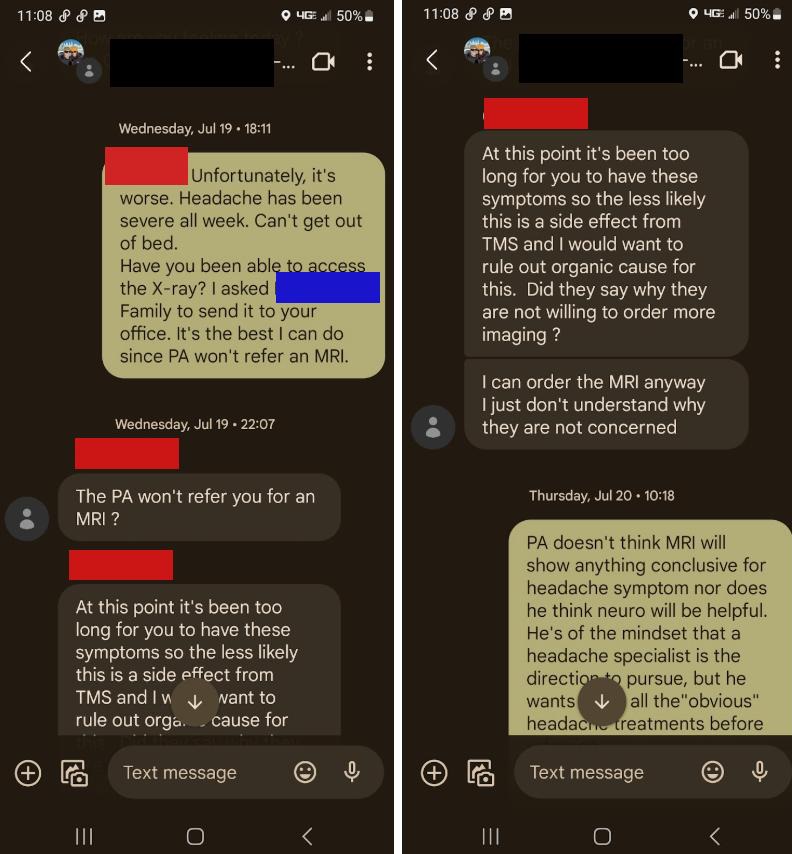
When I reached out to her about how much worse I was feeling, her replies didn’t reflect the type of compassion I hoped. On July 19, weeks after my last session, she told me it had been too long for TMS to still be causing symptoms. She said we should start looking into other causes. I was stunned. It felt like she was waving off everything I was going through, as if it couldn’t possibly be connected. She mentioned getting me in for an MRI, but nothing ever came of it and instead, she questioned my primary care manager who was only a physician’s assistant.
I asked over and over for my records. A month passed with silence. When she finally reached out again, I already felt abandoned. It felt too late for the amount of pain I had endured while she continued to market this treatment to others in the area.
I sent her a long message explaining everything I was dealing with. I told her how I couldn’t sleep, how the exhaustion and head pain forced me to nap every day just to function. I told her I had to cancel seeing family and stop doing the things I loved like yoga and running. My thinking had slowed down. Conversations were hard. I felt cut off from the world around me.
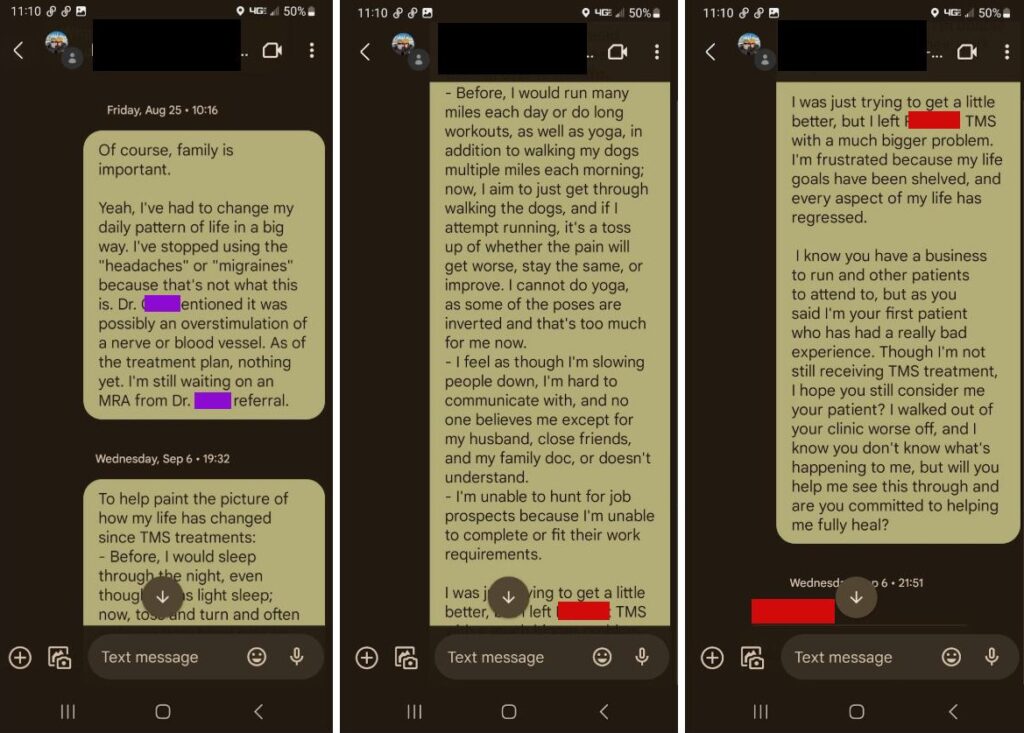
At first, it seemed like she might actually listen. She asked me to report what happened to the device company, NeuroStar, and suggested checking in with other specialists. But the longer it went on, the more it felt like she was pushing everything back onto me. I couldn’t even think about what to make for dinner, do simple math, or remember basic yoga poses that I had practiced and taught for 10 years. How would I know where to begin searching for answers? It felt like asking a young child a difficult, senior-level math problem. I was still trying to understand what had happened to my own brain, and now I was expected to chase down answers too. It made zero sense.
Weeks passed without updates. No real follow-up. The only referral she gave was to a neurologist she knew personally. That appointment was disheartening and honestly led nowhere. The doctor smiled politely but clearly didn’t believe TMS could have caused any of this. She ran some surface-level tests and repeated them until I “passed.” Then she dismissed everything else as overstimulation, without ever explaining what that meant or documenting the rest of my symptoms, despite me asking her in a follow-up email.
Later, my psychiatrist messaged me with an update from NeuroStar. It felt like a direct and personal punch to the gut. They claimed they had never heard of side effects like mine and said most people just get a headache that clears up in a few days. The neurologist they consulted didn’t even think my case needed a closer look.
Reading that made me feel like I didn’t exist. Like everything I had been going through was invisible to them. Like I was no longer a shiny new client that could make them money. I started questioning myself. Was I exaggerating? Making it up somehow?
I kept trying. I saw other neurologists, but the story was the same. One said it sounded like stress and said I just needed to be patient and take some headache and migraine medications. One told me TMS couldn’t possibly cause a brain injury and gave me a vague diagnosis of an “untraceable migraine.” And a few others denied my referral, stating that they could not find the source of injury in my medical files. It led nowhere.
I felt like I was losing my mind. These were the people who were supposed to help, and instead I was being talked over, dismissed, and doubted at every turn. It was maddening. With every dismissal, I felt like I was ever sinking into a deep, dark hole.
Finally, Someone Believed Me
Months later, I got an appointment at the Amen Clinic. That’s where everything shifted. The brain scans confirmed what I had known deep down. There was clear damage in my left prefrontal cortex and my cerebellum. The very area where TMS had been targeted showed significant dysfunction.
I didn’t want to be right about this. I didn’t want to have a brain injury. But seeing it on the scan finally gave me something solid. I wasn’t imagining it. I wasn’t overreacting. I could now relate my sudden adverse symptoms that happened immediately after TMS to concrete evidence on a scan.
That validation didn’t fix everything, but it gave me back a little piece of myself. After being doubted and dismissed for so long, it meant everything to be seen and taken seriously. I was more confident in silencing my self-doubt and more confident in pushing to be seen by providers. These scans gave me the courage to keep advocating for the right care.
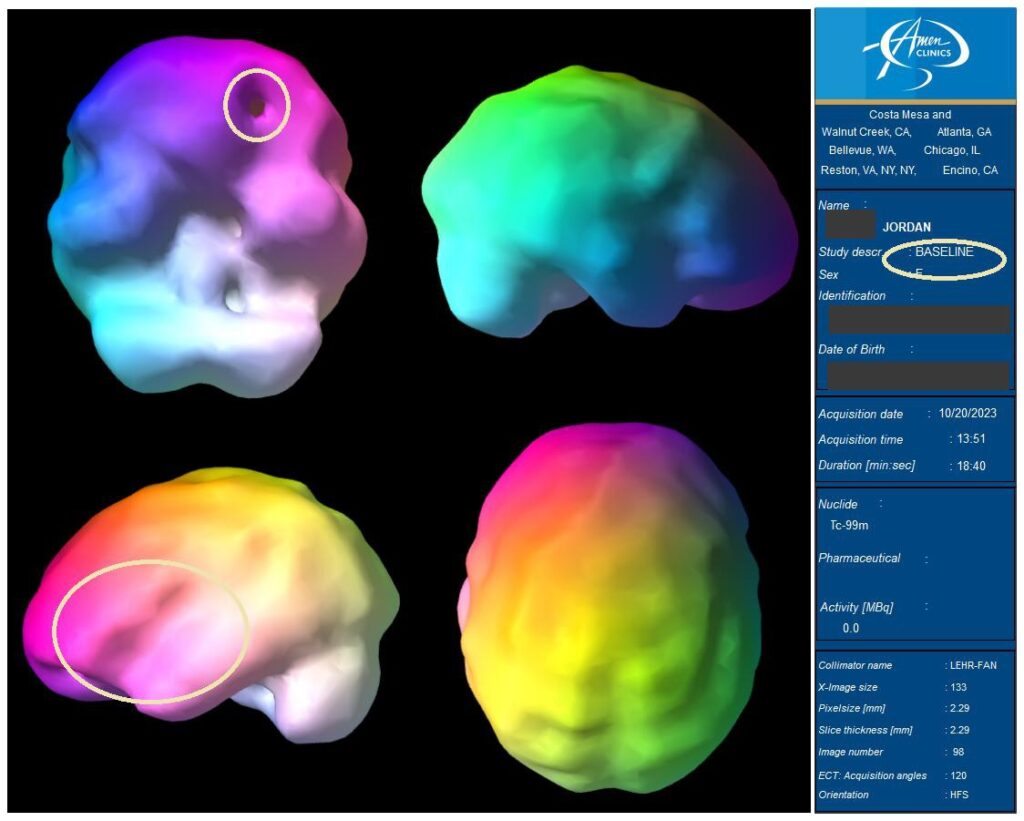
Still Searching for Answers
Even with my newfound confidence and brain scans showing clear injury, I kept running into walls. Doctors brushed off my symptoms, especially when I mentioned TMS. They called it stress or just headaches. But it was so much more than that. With one painful electromagnetic stimulation, my life drastically changed and I was not going to let others dismiss me anymore.
Advocating for myself has taken a huge toll. It’s exhausting, emotionally draining, and honestly, sometimes feels endless. This isn’t just discomfort. It’s a brain injury. Without proper diagnosis and early treatment, it can turn into Post-Concussion Syndrome, where symptoms last months or even years. And because it’s invisible, people don’t see how much it affects every part of life. Feeling misunderstood and alone has been one of the hardest parts.
The Fight to Heal
Recovery hasn’t been linear. I deal with fatigue, memory issues, and vision problems that make even simple tasks feel impossible some days. Walking my dogs or holding a conversation with anyone can leave me wiped out. I even tried to get back into massage therapy for a little bit and after one client, I was in bed for days recovering. It was too much for my system to handle and sadly, I had to end that chapter of my life.
Still, I’ve found a team to support the healing process. I’m working with craniosacral therapists, acupuncturists, physical and speech therapists, neuro-optometrists, and sports medicine doctors. Each one helps a different part of my brain and body. It’s slow, but there are signs of progress. I’m also doing daily therapy exercises and taking supplements designed to support nerve and brain repair.
Some of what I’m dealing with includes:
- Eye movement problems that make reading and tracking hard
- Double vision from convergence issues
- Depth perception difficulties
- Dizziness triggered by visual confusion
- Chronic neck and mid-back pain
- Sensory overload
- Trouble focusing, remembering, and thinking clearly
- Difficulty with speech and finding the right words
Every day, I work to regain what I lost. And every day I wish that someone had listened sooner. If my symptoms had been taken seriously right away, I know this path could have looked very different. But I am hoping that by sharing my story it will look different for someone else.
Realizing I’m Not the Only One
One of the turning points for me was realizing I wasn’t alone. I started connecting with others who had been injured by TMS. One doctor even mentioned seeing another patient with similar damage after just a few sessions. Online groups and posts from others reveal thousands of people sharing similar stories. It’s eye-opening and heartbreaking.
TMS is still advertised as non-invasive and safe, but that’s not the full picture at all. There are real risks, and too many people are being hurt without any warning, support, or accountability. There is also zero education on understanding the adverse symptoms of TMS and when to stop or start taking them seriously, and I see too many people online leaving it to blind faith that they will improve and so, too, will their depression.
Where I Go From Here
I’m going to keep telling my story. Not because it’s easy, but because I know how many people are quietly struggling just like I was. If this has happened to you, please know your pain is real. You’re not imagining things. And you’re not alone.
Keep speaking up. Keep pushing for the care you deserve. You’re worth it. Thank you for being here with me. I’ll keep sharing updates as I fight for healing, answers, and the respect every patient deserves.















I’m sorry to hear of your significant injury- why didn’t you stop going when you were clearly having pain and you knew something was wrong?
Report comment
Thank you for your concern, Cathy. I truly wish I had never undergone TMS, but that’s part of what makes this so complicated and heartbreaking.
Like many others, I was told to expect minor side effects like headaches and that I might feel worse before I felt better. I reported the pain and symptoms right away like the extreme pressure in my head, vision issues, and confusion, but the staff reassured me it was “normal” and even suggested it meant the treatment was “working.” I trusted the clinic. I was also misled to believe the psychiatrist was monitoring my sessions, when in fact she was out of town and unaware I was being treated.
By the time I realized something was seriously wrong, the damage had already been done. And once your brain is injured, it’s not like breaking a leg because you don’t always recognize how impaired you are until much later. I stopped after three sessions, but I still live every day with the consequences.
This is why I speak out now: because many people who are harmed are dismissed or blamed, when in reality, they weren’t given true informed consent or safety protocols. I hope my story helps prevent this from happening to others.
Report comment
DID FULL TREATMENT SESSIONS 27 I think. I experienced the same symptoms, then some. Short term memory non-existent, retrieving words is a problem, can’t ride my bike, ears ringing so intense I can cry at times, depression anxiety, reclusive, not social on most levels.
I’ve been complaining since 2018 in TMS Injuries since. Even the Mayo clinic(said FDA approved), not invasive. Bull Crap, I had no idea the problems are permanent and debilitating. Nobody can do anything, there is no help.
Report comment
Hey Sam, I’m so incredibly sorry you’re going through this. I can’t imagine how devastating it must be to have gone through 27 full sessions and be left with such severe, lasting symptoms. What you described about the memory loss, the word-finding issues, not being able to ride your bike, the intense ringing, and feeling reclusive, it’s heartbreaking.
Thank you for sharing your story and for being so brave and open. I know how hard it is to speak up when you’re in pain and feel dismissed or forgotten. Your voice matters so, so much and it helps others feel less alone.
As my story shares, I only did three sessions out of a planned 56 and still ended up with a serious, debilitating injury. It’s terrifying how quickly things can go wrong and how little help or acknowledgment there is when they do. It never gets easier to hear that the same has happened to others and again, I’m sorry it has happened to you.
And you’re absolutely right: TMS is not FDA approved, it’s FDA cleared through the 510(k) process, which doesn’t require thorough long-term safety testing. It was pushed through under a loophole. The Center for Research on Women and Families has raised major concerns about this:
https://www.center4research.org/statement-national-research-center-women-families-fda-advisory-panel-meeting-regarding-neurostar-tms-system-major-depression/
I’m just so sorry this happened to you. None of us deserved this and I hope you know that what you’re feeling and experiencing is valid.
The more we connect and share our stories, the more I truly believe we’ll start to uncover ways to heal. We may not have all the answers yet, but together, we can move through this even if it’s slowly, even if it’s messy. You’re not alone in this. If I have any resources to share further, I will certainly do so. I’m sure you know about VTAG and I hope you found understanding there. I’ve created a resource booklet that is ever changing as I learn more, but you’re welcome to explore it.
https://www.jordansartfulwellness.com/_files/ugd/d3ad28_087e9a0be61e4cdfb246d2669694c400.pdf?index=true
Report comment
Thanks so much for sharing your story Jordan. I’m so sorry you were treated this way. I really appreciate how you explain so clearly the way that patients are ignored, overridden and gaslighted and how that disempowers us and causes extreme and life destroying harms to be perpetrated without accountability. We go to these people with trust and belief that they are doctors and know what they are doing, this is what we are taught to do. When something goes wrong, very often we are disbelieved and blamed.
This sums up the entire history of psychiatry/mind doctoring for me – experimental treatments which destroy lives and are enabled to continue by a systemic inability to believe patient’s own words. It happens in medicine too, (I don’t believe psychiatry is a medical science) especially to women patients, but at least medicine has a history based in the scientific method and cannot gaslight so easily. Psychiatric treatment is little more than experimentation on systemically silenced people.
I hope and wish you all the best for your recovery.
Report comment
Freya, thank you so much for your thoughtful words. It means a lot. You’re so right. We go in with trust, doing what we’re taught to do, and when things go wrong, it’s like the system flips on us. Instead of care, we’re met with denial, blame, or silence. It’s devastating.
What you said about psychiatry and the pattern of disbelieving patients rings painfully true. The way people are experimented on, dismissed, and often left to pick up the pieces alone is a deep, systemic failure.
I really appreciate your compassion. Wishing you strength too, wherever you are on your own path. We need each other in this.
Report comment
First of all this is a beautifully written account of what happened to you. Its clear and it shows so many problems with what people are going through all over the world every day with this treatment. You described aspects that I never had, or even thought about really, even though I have run through my own experience countless times in my own head and in discussions with others. There is just no end to how many things are wrong with this treatment and how it is administered.
It crushed me to read about what happened and how they treated you, I still cry every time I hear a new first person account from someone and yours is certainly no exception. It defies all reason, how it was handled and what you had to endure and why. It makes absolutely no sense you had to go through that, and it makes even less sense that, that was how it was handled. To hear a TMS clinic tell it, what you experienced isn’t even possible, and YET, I HAVE HEARD THE SAME OF EQUIVALENT THING HUNDREDS IF NOT A THOUSAND Time. How is this possible?! The Lying and the incredulous violence against our minds and bodies, it makes no sense, in a society where this runs unchecked and even encouraged, we live in a joke of a community.
You present a crystal clear picture of it.
I think its really interesting the doctor did a virtual follow up like everything was fine, my clinic actually called me to see if I would film a promotional video for them promoting TMS because I was so nice to them. Somehow, they did not remember, that I told them over and over again I felt drunk(cognitive impairment) and developed tinnitus during the sessions, and also that I was permanently disabled and lost my job because of the treatments. They kept just talking to me like I was fine despite everything I said and did. It makes no sense at all. The largest part of my mind thinks they have to be doing TMS themselves or using psych drugs so their own thinking, memory and connection to others is severely inhibited. It just makes no sense.
They literally ignored everything I said and did.
“Later, my psychiatrist messaged me with an update from NeuroStar. It felt like a direct and personal punch to the gut. They claimed they had never heard of side effects like mine and said most people just get a headache that clears up in a few days. The neurologist they consulted didn’t even think my case needed a closer look.”
This is hilarious, I have seen so many reports to the FDA as well as neurostar that describe exactly what you went through, which were reported to them starting about 5 years before you made the report. It is complete fiction that they did not have these reports. They are also public in the FDA’s MAUDE database.
I can’t thank you enough for sharing your story here and everywhere else you do. Neither of us can know how much of a difference it makes now and in the future for so many. No one should go through this horror alone, but it is survivable by anyone who believes that they are stronger than their injury.
You are absolutely crushing it. Hang in there, your doing everything right.
Sooooooooo happy to see this here.
Report comment
James, wow wow. I had to sit with this before responding. Your words are so deeply validating and painful and true, and I felt them all. Thank you for reflecting it all back. It means more than I can say.
You’re right. There’s just no end to how many layers of wrong there are with TMS and how it’s pushed, sold, and badministered. Reading your story, I had the exact same reaction. Moments where I went, wait, I’ve never even thought of that before, even though I live with the same injury. There’s something about hearing it from someone else that cuts deeper but connects to what, I think, we all experience. Like it gives permission to grieve what we couldn’t fully name.
I’m so sorry you went through what you did. The promotional video ask… I mean, what? It’s like they’re living in a different dimension. It’s surreal and enraging.
The gaslighting is so calculated. I’ve seen those same reports in the MAUDE database too. They knew. They know. And they’re still pushing it, still pretending. It’s beyond negligence. It’s a machine fueled by denial and profit and people who don’t want to see the truth.
Also, I just want to say. I came across your posts and your blog on Mad in America right after my injury. I think it was just the right Google search at the right moment, and I honestly don’t know what I would’ve done if I hadn’t found them. Your story helped me put words to what was happening, and it gave me the strength to keep looking for answers. I really hope that with more of us speaking out, it becomes even easier for others in crisis to find these stories and feel less alone.
Your words are a lifeline, James. Truly. I hope you know that your voice is helping hold up so many people, including me. None of us should be carrying this alone, and somehow, through the wreckage, we’re finding each other. That gives me hope.
Thank you for being here. I’m grateful for you.
Report comment
I agree entirely, badministration – I love that.
Thank you for your honesty and kind words and most of all thank you for being a part of the lifeline.
Report comment
Thank you, James!
Report comment
Thank you so much for sharing this. It is a horrendous story. I believe you will help many people by putting out this information. You are very brave. Daniel.
Report comment
Thank you, Daniel. That really means a lot. It’s been an incredibly painfully tough road, but hearing that sharing my story might help someone else makes it feel totally worth it. I really appreciate you taking the time to read and say something. Truly. Thank you!
Report comment
Thank you, Daniel. That really means a lot. It’s been an incredibly painfully tough road, but hearing that sharing my story might help someone else makes it feel totally worth it. I really appreciate you taking the time to read and say something. Truly. Thank you!
Report comment
I’m very sorry but not surprised that you were treated this way. If we have physical symptoms they are very often assumed to be delusions, psychosomatic, or attention seeking, or to be wholly acceptable because XYZ treatment is the “newest and best” and the supposed therapeutic benefits are deemed more important than actual outcome and quality of life.
You did nothing wrong. You didn’t deserve to be misled, harmed, gaslighted, and dismissed. I commend you for seeking out answers and for sharing your experience. I’m glad that you’ve found community where you are heard and understood by others who live with similar outcomes.
May we all live in well being, dignity, and bodily autonomy.
Report comment
Hi Song,
Thank you so much your words really moved me. It’s validating to be met with that kind of understanding, especially after so much gaslighting and dismissal. You’re so right when physical symptoms follow a psychiatric treatment, they’re too often written off as psychosomatic or somehow less real. And when a treatment is marketed as cutting-edge or “safe,” any harm becomes almost untouchable, like we’re not allowed to question it without being labeled as unstable or ungrateful.
In my case, the psychiatrist even falsified my records claiming I was on Zoloft when I wasn’t. We now believe she did that to get my treatment pushed through insurance faster, so I could be approved and put into the machine without delay. That kind of deception just to streamline a process is terrifying. It robbed me of informed consent and contributed directly to the harm I experienced.
I didn’t want to become a cautionary tale, but I also couldn’t stay silent when the harm was so real. Finding others who get it who truly see what’s happening has helped me start to reclaim pieces of myself that were lost in the process.
Thank you for holding space, for naming the bigger issue, and for reminding me that this isn’t just personal. It’s systemic. I hope we all keep raising our voices until dignity, honesty, and bodily autonomy are non-negotiable in care.
Sending warmth and deep respect All the best.
Report comment
I am so sorry this happened to you! I feel like TMS is pushed so often for people with depression. I am very grateful to you for sharing your story; I’ve been recommended this “treatment” and have been researching it before I commit (now I am not going to!). I already suffer from migraine and fatigue, and my concerns about those symptoms worsening was dismissed by my doctor. I hate that the significant risk of severe symptoms and injury is downplayed by doctors. I wish you continued healing, and really appreciate the bravery it took to share your story.
Report comment
Thank you so much, Heather. I really appreciate your kind words and support. It means a lot to know others are questioning and researching before committing to TMS, especially with symptoms like migraines and fatigue that could be worsened. It’s heartbreaking how often concerns get dismissed or downplayed, and that’s exactly why I felt compelled to share my experience to help others avoid harm and to push for better awareness and safety. It means the world that my story made an impact on you to keep questioning and putting your health first. Wishing you strength and healing on your journey as well.
If you ever want to connect or learn more resources, feel free to reach out. We’re in this together.
P.S – If you do not mind, I did have a thought about your migraines and fatigue and wondered if you looked into methlyation?? I’m not a doctor, but learning about methylation really helped me understand some of my symptoms related to fatigue (before TMS). Methylation is a natural process in your body that affects how your genes work and helps with things like energy, detox, and brain health. For me now, it is now even more important to my current healing for my brain recovery.
There are 12 common markers that show how well this process is working, and I found out I had issues with about 10 of them. After making some changes like adjusting my diet and supplements, I noticed improvements. It might be worth exploring??
Report comment
Thank you so much for sharing! I haven’t heard of methylation, but I will definitely look into it and see if there are any improvements I can make to my diet or any supplements I can add. I appreciate you letting me know!
Report comment
You’re so welcome and I really hope it proves helpful! Methylation can definitely feel like a deep rabbit hole at first, but even small steps can make a big difference. I actually wrote a simple intro blog about it that doesn’t get too far into the weeds (there are over a dozen types of methylation ), but it might give you a good starting point as you explore: https://www.jordansartfulwellness.com/post/understanding-methylation-my-journey-and-why-it-matters
Feel free to reach out if you ever want to chat more about it. It’s been such a key piece in my own healing.
Report comment
Sue them!!!
Report comment
I hear you so much! The urge for justice is strong, especially when the harm is so real and lasting. It’s a complicated road, but speaking out and connecting with others who get it has been a powerful first step. Thank you for reading my story and speaking out!
Report comment
I struggled with depressive episodes for 20 years, and it appears my distrustful and independent nature has kept me from harm’s way, as I never went to a psychiatrist for help. Instead, I went to Jesus and did repeated deliverances. Worked beautifully — no need for meds, counseling sessions, electric shocks, etc.
Report comment
Thank you for sharing your journey. I’m really glad you found a path that worked for you and brought relief. I totally understand the instinct to be cautious; if I had trusted mine more, I might have avoided what happened to me with TMS. I think your story shows how personal and diverse healing can be and how sometimes, it’s the systems we don’t go through that end up sparing us harm.
My piece was really about speaking up for those of us who did seek help through psychiatry and got hurt in ways that were deeply preventable. I wish that kind of harm wasn’t even possible in a system meant to heal. Your comment reminds me how important it is to trust our own sense of what’s safe and right and why we need to keep shining light on practices that carry risk, especially when people are vulnerable and just trying to get better.
Report comment