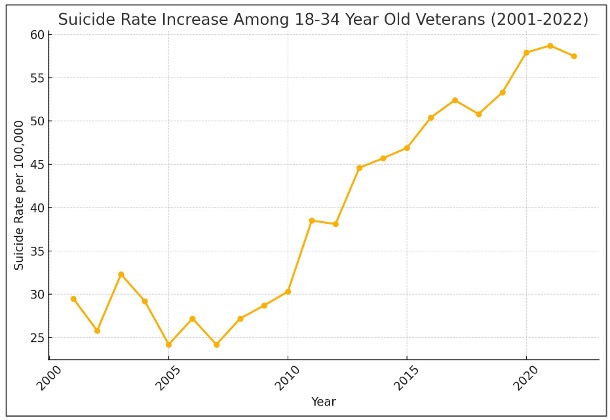
The veteran suicide epidemic has taken the lives of more than 155,000 veterans since 2001. Since 2015, an average of 6,500 veterans have died by suicide each year, with 2,400 (36%) occurring while under the care of the U.S. Department of Veterans Affairs (VA). Suicide numbers for 18-to-34 year-old veterans have more than doubled since 2001, while any progress towards decreasing the number of veteran suicides for all veteran demographics could be described as modest at best. These outcomes continue to frustrate veterans, families, advocates, experts, and lawmakers alike, in spite of the fact that the VA’s spending on veteran mental health and suicide prevention has steadily increased, with the VA spending $16.6 billion on mental health in 2024, including $559 million on suicide prevention.
To address this crisis, U.S. Representatives Gus Bilirakis, Jack Bergman, and Keith Self have introduced have introduced HR 4837, the “Written Informed Consent Act.” This legislation is supported by more than 17 national veterans organizations, which some believe could play a leading role in reducing the number of suicides at the VA by as much as 25%—potentially saving 600 veterans lives a year.

HR 4837 addresses deficiencies in informed consent practices, which have been identified by the VA’s Office of Inspector General (OIG) and which were detailed by the Wall Street Journal in a recent report on VA overprescribing: “‘Combat Cocktail’: How America Overmedicates Veterans.” This legislation will lead to safer and smarter use of psychotropic medications, while providing critical safety information to patients. Today, nearly 70% of all veterans under VA care are prescribed these drugs, many of which include FDA warnings of suicidal thoughts and behaviors—a risk that, as many veterans can attest, they were not warned about when they were prescribed these drugs.
While the problem of doctors not discussing the risks and benefits of drug treatments also exists outside of VA care, prescription rates for veterans treated at the VA are more than four times those of their civilian counterparts, and the VA is the setting where immediate and deliberate action can be taken to save lives today.
The Veterans Lost at Home
On November 13, 2022, Hunter Whitley, a U.S. Marine Corps veteran, shot himself to death in his apartment while attending college at the University of Alabama. Hunter was 23 years old. A month before his death, Hunter was prescribed the antidepressant mirtazapine, but according to an investigation by the VA’s OIG, the mental health nurse practitioner (MHNP) who prescribed the drug to Hunter “did not discuss mirtazapine’s boxed warning of increased risk of suicidal ideation or behavior for young adults.”
On April 13, 2023, five months to the day after Hunter’s death, Connor Brumfield, U.S. Army veteran, killed himself in his apartment while attending college at Montana Tech. Connor was 22 years old. Eight days before his death, Connor visited his local VA clinic for a vision test. While there, Connor was screened for mental health concerns, and the screening found that Connor had “moderate depression.” This was Connor’s first and only appointment, which lasted a little over an hour. During this short period a geriatric specialist nurse practitioner diagnosed Connor with a psychiatric disorder and prescribed the antidepressant bupropion (Wellbutrin) to treat it.
As was the case with Hunter Whitley, a legal review of Connor’s records found that the VA failed to discuss the FDA’s black box warning to monitor for suicidal thoughts and behaviors associated with the use of bupropion for young adults under the age of 24. Each of the antidepressants prescribed to Hunter and Connor had this black box warning:
“WARNING: SUICIDAL THOUGHTS AND BEHAVIORS: Increased risk of suicidal thoughts and behavior in pediatric and young adult patients taking antidepressants.”
Short of removing medications from the market, the black box warning is the most severe action the FDA can take. But these warnings are protective only if doctors and nurse practitioners prescribing these drugs take the warnings seriously and have robust conversations with their patients not only about their possible benefits, but also their risks and possible side effects. The side effects are many, including drug dependence, aggression, paranoia, thoughts of suicide, persistent sexual dysfunction after discontinuation of medications (in some cases permanent), cardiac issues, and possible harm to the fetus when the mother takes a selective serotonin reuptake inhibitor (SSRI) while pregnant.
In spite of the fact that both Hunter and Conner were younger than 24 years old, it appears neither was warned of any of these risks. In Hunter’s case, investigators found that not only was there no documentation of informed consent, the prescriber failed to discuss the black box warning entirely. With Connor, no documentation of an informed consent discussion was recorded, which implies he too was not made aware of the FDA’s black box warning. Their deaths contribute to the doubling of suicide rates for 18-to-34 year-old veterans since 2001.
A Systemic Failure
On September 26, 2024, the VA OIG published the results of their investigation into Hunter Whitley’s death. Its report was titled: “Mismanaged Mental Health Care for a Patient Who Died by Suicide.”
“The OIG would have expected the MHNP to provide information about the mirtazapine boxed warning directly to the patient given the applicability of the warning for the patient. The MHNP’s failure to provide the patient education regarding mirtazapine’s boxed warning likely resulted in the patient’s insufficient awareness of the need to self-monitor for suicidal thoughts and seek supportive resources as needed.”
The conclusion to draw from this report is obvious: The prescribers’ failure to provide informed consent likely contributed to Hunter’s suicide.
The same day that the VA’s OIG published their findings on Hunter’s death, it also published the results of a “Mental Health Inspection of the VA Augusta Health Care System in Georgia,” which found that 27% of veteran electronic health records (EHRs) did not show any evidence that prescribers discussed the risks and benefits of medication treatments with their patients.
Six months later, on March 5, 2025, the VA OIG published results of its “Mental Health Inspection of the VA Central Western Massachusetts Healthcare System.” Investigators found that 30% of EHRs did not show documentation of discussions with patients of “risks and benefits of medication treatment.”
Three months later, on June 6 and June 26, 2025 respectively, the VA OIG published reports of its Mental Health Inspections of the VA Philadelphia Healthcare System in Pennsylvania and the VA Salem Health System in Virginia. In both cases the VA investigators found that “most EHRs did not have evidence of required discussions with veterans on the risks and benefits of prescribed medications.”
The OIG reports tell of a systemic failure. And as a veteran with experience of being treated in and out of the VA health system, I can attest to this failure. Two months ago, I visited my local VA clinic in Lansing, Michigan. I’d been struggling, and during our discussion the provider suggested we try an antidepressant. When I told her that I “suffered a horrific yearlong withdrawal from Zoloft,” she was shocked and seemed unable to believe me. The psychiatrist who’d prescribed me the drug had a similar reaction: “I’ve never had a patient who has had as many issues with these medications as you.”
As I described the panic attacks, brain zaps, paranoia, akathisia and a host of other symptoms, the psychiatrist seemed even more confused about my experience with antidepressant withdrawal. “I’ve never heard of this,” she said.
Now I was shocked. Today, in 2025, antidepressant withdrawal is a known problem. With all of the studies we now have, petitions to the FDA and awareness in pop culture, many prescribers of psychiatric drugs still do not know of the prevalence and severity many experience with antidepressant withdrawal, even though studies have found that for 40% of patients, “withdrawal symptoms had lasted more than 2 years and 80% were moderately or severely impacted by them. One in four were unable to stop their antidepressant.”
Not Just a Veterans Issue
On July 21, 2025, the FDA commissioner, Dr. Marty Makary, hosted a panel of researchers and clinicians whose task was to discuss studies and clinical experiences with patients who had taken SSRI antidepressants while pregnant, and the risks such medication use posed to fetal development. A common theme emerged throughout the nearly two-hour panel: patients are not being informed of the known risks of SSRIs. Whether the risks were suicidal thoughts, increased risk of miscarriages, developmental risks to infants exposed in utero to antidepressants, or withdrawal issues, the panel members all spoke of how patients are not being provided with informed consent, even when black box warnings may detail them. In addition, they spoke of how the FDA has not properly updated drug labeling to reflect known safety issues with psychiatric medications.
If enacted, the Written Informed Consent Act will do more than save lives for veterans under the care of the VA. It would be the first meaningful reform to prescribing practices and informed consent in the United States in the nearly 20 years since the FDA put black box warnings on SSRIs that these drugs could induce suicidal thoughts and behaviors in young adults. As such, it would be a reform that would benefit the general public as well.
The Bill
Though less than half a page long, the Bilirakis, Bergman, and Self bill will save lives. It does so by expanding to psychiatric drugs the written informed consent policy that currently exists in the VA for the prescribing of opiates for longer-term use, a policy established under the Obama administration in 2014 and expanded and updated under the Trump administration in 2020. The bill will require prescribers to obtain written informed consent for other classes of high-risk medications, including antipsychotics, antidepressants, anxiolytics (benzodiazepines), stimulants and narcotics. Many of the drugs in these classes already carry black box warnings for suicidal thoughts and behaviors, and the inserts regularly describe other possible serious adverse drug events. For U.S. veterans, passage of the Written Informed Consent Bill is one of the most significant lifesaving actions our lawmakers can take.
In 2010, the House Veterans Affairs Committee held hearings on “Exploring the Role of Medications in Veteran Suicides.” Though concerns were raised by national experts, the committee did not act, even to make simple reforms such as strengthening informed consent policies at the VA. If such reforms had been enacted, thousands of lives might have been saved. We can’t afford to lose another fifteen years and another 90,000 veterans. If you find this argument compelling, please contact your representatives and senators and request their support of HR 4837, the “Written Informed Consent Act” to make prescribing practices safer and smarter for our nation’s veterans.
Here are just a few of the endorsements of the bill:
“The VFW strongly supports the Written Informed Consent Act, to direct the Department of Veterans Affairs to require informed consent from veteran patients before starting long-term treatment with psychiatric and pain management medications. This is standard medical practice for commonplace procedures and anything requiring anesthesia. This legislation is a vital step toward ensuring that veterans are fully informed about the risks, benefits, and alternatives before starting treatment with these medications—enhancing transparency and empowering veterans with the knowledge they need to make safe, informed decisions about their health. The VFW thanks Congressman Bilirakis for introducing this important legislation, and we urge Congress to ensure its swift passage.”
—Meggan Coleman (Thomas), Associate Director of National Legislative Services for the VFW.
“The Written Informed Consent Bill is one of the most important and significant lifesaving actions our lawmakers can take in our time.”
—Steven Rogers, Executive Director, Association of the United States Navy.
“The Tragedy Assistance Program for Survivors (TAPS) is grateful to Congressmen Bilirakis and Bergman for introducing legislation to require “Written Informed Consent” for high-risk medications. Suicide loss survivors have shared with TAPS how these ‘black box’ medications contributed to their veterans’ suicide ideation and death. TAPS urges swift passage of this critical legislation to help save precious lives.”
—Bonnie Carroll, TAPS President and Founder
“For medications with black box warnings, especially those linked to serious mental health risks, written informed consent is vital. ROA thanks Congressman Bilirakis for championing legislation that ensures members of the uniformed services, veterans, their families, and caregivers are fully informed before beginning treatment. At a time when our nation is facing a growing mental health crisis, often tied to the conditions for which these medications are prescribed, this legislation is a critical step toward supporting resilience, improving outcomes, and protecting those who serve and support our country.”
—Matthew Schwartzman, Director, Legislation and Military Policy Reserve Organization of America
“Veterans deserve to know exactly what medications they’re taking and what the potential side effects are. Written informed consent is a simple, vital step to ensure they’re educated about their care and empowered in every treatment decision. AFSA strongly supports this effort to protect the health and well-being of those who served, past, present, and their families.”
—Keith A. Reed, Chief Executive Officer, Air Force Sergeants Association
“Veterans have the right to understand the full impact of the medications they are prescribed, especially those affecting mental health and long-term quality of life. This legislation takes an important step toward strengthening informed consent within the VA by ensuring veterans receive clear, consistent information before starting treatments such as antipsychotics, stimulants, antidepressants, anxiolytics, and narcotics. The Fleet Reserve Association strongly supports this effort and urges Congress to move quickly on its passage.”
—Theodosius Lawson, Assistant Director, Legislative Programs, Fleet Reserve Association
“Veterans deserve to be fully informed about the medications they take, especially those with potentially dangerous side effects. DAV is proud to support the Informed Consent for Long-Term Opioid Therapy for Pain Act, which requires clinicians to inform veterans of medications that pose serious safety risks and provide them alternative treatment options. We applaud Rep. Bilirakis for his leadership on this critical issue to ensure transparency, promote veteran-centered care and safeguard the health and well-being of our nation’s veterans.”
—Joy Ilem, DAV National Legislative Director
“AMVETS proudly supports this legislation to ensure veterans prescribed high-risk medications are fully informed before starting treatment. Written consent creates a clearer understanding of potential risks and alternatives, and our veterans deserve that confidence when making decisions about their care.”
—AMVETS National Executive Director Joe Chenelly
“Informed Signatory Consent is not just a legal checkbox, it’s a moral obligation. Veterans deserve to know exactly what they’re being prescribed, what the risks are, and what the alternatives might be. When we remove informed choice, we increase dependency, confusion, and risk of harm. Giving veterans real consent is one of the most critical and overlooked tools we have in preventing suicide.”
—Tim Jensen, Combat Veteran & Chairman, Grunt Style Foundation
Here are the VSOs supporting Written Informed Consent with resolutions:
The American Legion
Veterans of Foreign Wars (VFW)
Disabled American Veterans (DAV)
Jewish War Veterans (JWV)
Reserve Officers Association (ROA)
Additionally, other VSOs and MSOs have agreed to support this issue and legislation:
Association of the United States Navy (AUSN)
Special Operations Association of America (SOAA)
Military-Veteran Advocacy (MVA)
Fleet Reserves Association (FRA)
Marine Corps Reserve Association (MCRA)
Navy Seal Foundation (NSF)
Vietnam Veterans of America (VVA)
Air Force Sergeants Association (AFSA)
Grunt Style Foundation
American Veterans (AMVETS)
Military Order of the Purple Heart (MOPH)
Tragedy Assistance Program for Survivors (TAPS)
Together, these organizations are simply asking for the VA to provide more information for patients and doctors to make prescribing practices at the VA safer and smarter. If you agree with these calls to action, please contact your representatives in Congress and urge them to co-sponsor and support this legislation to require written informed consent about the benefits and risks associated with antidepressants, antipsychotics, and other classes of psychiatric drugs.












Too cool, Derek. I hope this becomes a legal requirement for all doctors, if it technically isn’t already?
As a psychopharmacology researcher who found the medical evidence that the antipsychotics can create psychosis, and other “positive symptoms” of “schizophrenia,” via anticholinergic toxidrome; as well as the negative symptoms of “schizophrenia,” via neuroleptic induced deficit syndrome.
Please do include my medical research findings in the informed consent forms for the VA. And if you need a contact at the Cleveland VA, my son used to work there, and still has “Presidential managerial fellowship” friends who do still work there.
Report comment
Excellent from http://www.ablechild.org happy to support this legislation.
Report comment
The confessions of Senator Patty Murray and Rep Bob Filner, “This is disgraceful! This is a crime against our Nation, our Nation’s Veterans!” and the coverup of 1000s of Veterans Suicides prescribed by VA Mental Health over the past 35 years, is documented on page 110 of “The Truth About Veterans’ Suicides” 110th Congressional Hearing 21 Apr 2008.
Beverley Susan Melampy
Veteran’s Suicide Advocate
Survivor H.R. 841 (1991)
Report comment
Thank you for providing the following resource of information regarding Veterans Suicide and the tools to help combat this fatal medical condition.
Adam’s Story
Report comment