A new report, published in the National Institutes for Health Research Journal, provides what the authors call “the most substantive evidence to date on acupuncture and its potential impact.” The studies included in the report provide compelling evidence for the use of acupuncture in the treatment of both chronic pain and depression. Their results address prior uncertainties regarding the practice as a medical treatment.
“The programme of research found that acupuncture was more effective than usual care and sham acupuncture for chronic pain, that it was one of the more clinically effective physical therapies for osteoarthritis and that it showed benefits in the treatment of depression.”
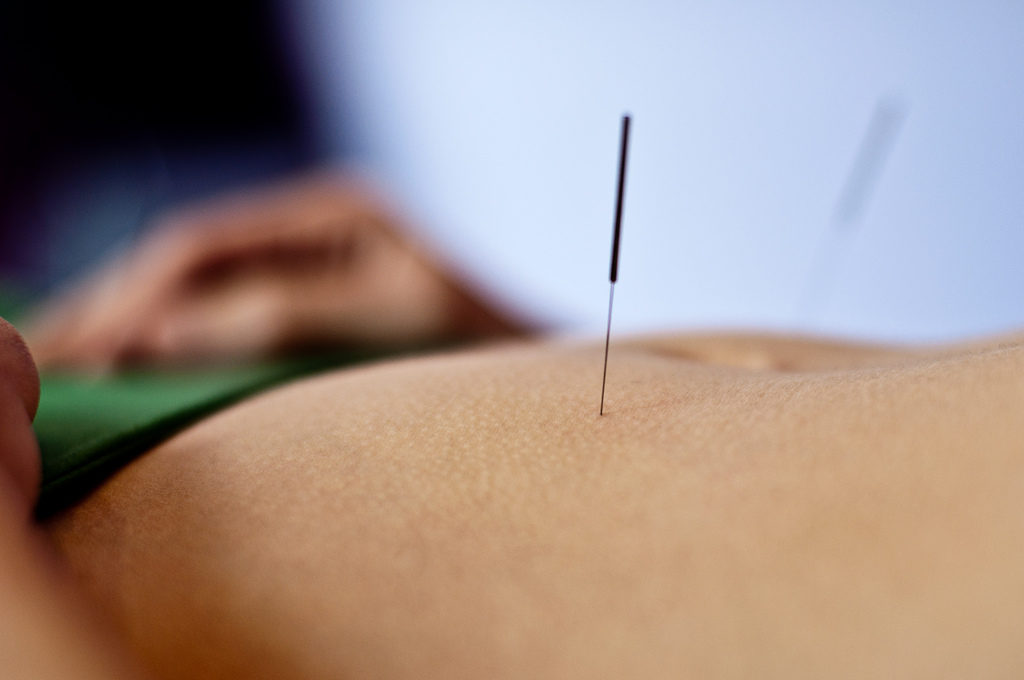
Acupuncture is widely used around the world, commonly for the treatment of chronic pain. More recently, it has been added to the list of non-pharmacological treatments for depression, for which it has shown some promise. Despite the common and widespread use for both of these conditions, researchers remain uncertain regarding the effectiveness of acupuncture, given poor quality or lack of evidence in both of these domains. Interest in acupuncture as a treatment for depression has surged, as the effectiveness of antidepressants has been questioned, and individuals have voiced concern about their side-effects.
One of the studies’ aims was to understand the clinical effectiveness of acupuncture for chronic pain. For this report the researchers conducted a systematic review of the literature, compiling data from twenty-nine trials, which had just fewer than 18,000 participants. In addition, the researchers conducted a randomized control trial (RCT) of acupuncture treatment for depression with 755 participants.
Overall, the researchers found that acupuncture was not only a suitable option for the treatment of chronic pain but that it was also significantly more effective than a placebo. In addition, it was more cost effective than other compared treatments. Acupuncture was found to be effective for chronic pain across different areas including head, back, neck, and knee.
“In an RCT of acupuncture or counseling compared with usual care for depression, in which half the patients were also experiencing comorbid pain, we found acupuncture and counseling to be clinically effective and acupuncture to be cost-effective,” the researchers wrote.
In their RCT the researchers found that those patients who received acupuncture experienced significant reductions in depression symptoms compared to those who received just standard care. They found the same with the participants who received counseling. However, those receiving acupuncture had similar gains with less associated financial costs.
The study not only provided robust evidence regarding the use of acupuncture for chronic pain and depression, it also quashed any doubts regarding the potential placebo effects of acupuncture. By furthering their research aims to include cost effectiveness, they also made a substantiated argument for potential discussions around policy and health.
“By comparing acupuncture in an unbiased way with other ‘competing’ physical or psychological therapies, we are providing the very evidence on clinical effectiveness and cost-effectiveness that is of most value to policy-makers and commissioners.”
****
MacPherson, H., Vickers, A., Bland, M., Torgerson, D., Corbett, M., Spackman, E., … & Manca, A. (2017). Acupuncture for chronic pain and depression in primary care: A programme of research. National Institutes for Health Research. (Abstract)















It always amazes me the lengths to which “alternative therapies” like acupuncture have to go to prove their effectiveness, despite in many cases THOUSANDS of years of experiential data, while drugs are given a pass after two pre-screened 6-week trials show that they are slightly better than doing nothing at all. Double standard, anyone?
Report comment
I agree, it is a double standard. Massages are also nice, they actually help with pain, and they’re not yet covered by insurance.
There are lots of effective, actual cures for pain that the medical industry doesn’t want covered because doctors want to manage symptoms, rather than cure people, since this is so much more profitable.
Report comment
Excuse me, what experiential data?
Report comment
I have searched for “acupuncture” and I found a Cochrane review on its efficacy for treating “depression”. Here’s the link: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD004046.pub4/full?highlightAbstract=acupuncture%7Cacupunctur
These are the main results:
“This review is an update of previous versions and includes 64 studies (7104 participants). Most studies were at high risk of performance bias, at high or unclear risk of detection bias, and at low or unclear risk of selection bias, attrition bias, reporting bias, and other bias.
Acupuncture versus no treatment/wait list/treatment as usual
We found low‐quality evidence suggesting that acupuncture (manual and electro‐) may moderately reduce the severity of depression by end of treatment (SMD ‐0.66, 95% CI ‐1.06 to ‐0.25, five trials, 488 participants). It is unclear whether data show differences between groups in the risk of adverse events (RR 0.89, 95% CI 0.35 to 2.24, one trial, 302 participants; low‐quality evidence).
Acupuncture versus control acupuncture (invasive, non‐invasive sham controls)
Acupuncture may be associated with a small reduction in the severity of depression of 1.69 points on the Hamilton Depression Rating Scale (HAMD) by end of treatment (95% CI ‐3.33 to ‐0.05, 14 trials, 841 participants; low‐quality evidence). It is unclear whether data show differences between groups in the risk of adverse events (RR 1.63, 95% CI 0.93 to 2.86, five trials, 300 participants; moderate‐quality evidence).
Acupuncture versus medication
We found very low‐quality evidence suggesting that acupuncture may confer small benefit in reducing the severity of depression by end of treatment (SMD ‐0.23, 95% CI ‐0.40 to ‐0.05, 31 trials, 3127 participants). Studies show substantial variation resulting from use of different classes of medications and different modes of acupuncture stimulation. Very low‐quality evidence suggests lower ratings of adverse events following acupuncture compared with medication alone, as measured by the Montgomery‐Asberg Depression Rating Scale (MADRS) (mean difference (MD) ‐4.32, 95% CI ‐7.41 to ‐1.23, three trials, 481 participants).
Acupuncture plus medication versus medication alone
We found very low‐quality evidence suggesting that acupuncture is highly beneficial in reducing the severity of depression by end of treatment (SMD ‐1.15, 95% CI ‐1.63 to ‐0.66, 11 trials, 775 participants). Studies show substantial variation resulting from use of different modes of acupuncture stimulation. It is unclear whether differences in adverse events are associated with different modes of acupuncture (SMD ‐1.32, 95% CI ‐2.86 to 0.23, three trials, 200 participants; very low‐quality evidence).
Acupuncture versus psychological therapy
It is unclear whether data show differences between acupuncture and psychological therapy in the severity of depression by end of treatment (SMD ‐0.5, 95% CI ‐1.33 to 0.33, two trials, 497 participants; low‐quality evidence). Low‐quality evidence suggests no differences between groups in rates of adverse events (RR 0.62, 95% CI 0.29 to 1.33, one trial, 452 participants).”
I would be wary of the comparisons between meds and acupuncture given that Cochrane reviews of psychiatry are not as trustworthy, but I think that this already tells a lot about the efficacy of acupuncture for depression. Basically, evidence is of very low quality.
Report comment
While the trial on depression is indeed an RCT, the comparison was not between acupuncture, counseling and sham acupuncture, but between acupuncture, “treatment as usual” (I don’t know what this means in this case) and counseling. You can’t know whether either of those interventions beat placebo this way.
Report comment
Also note that, in the Acknowledgements of related funding section, it says that “The ATC [Acupuncture Trialists Collaboration] is funded by a R21 (AT004189I) from the National Center for Complementary and Alternative Medicine at the National Institutes of Health”
Report comment