Four years ago I dove into a deep and murky pond: the bottomless depths of medical databases that hold mental health research extracted from the bowels of journals from around the world.
I dove in, not as a career choice, but as a survival instinct, when a loved one entered psychiatric crisis. Above the water line, I found a disjointed and overburdened mental health system offering an array of psychiatric drugs that brought partial symptom relief with a debilitating array of side effects. Below the water line, I grasped for evidence of something better. My loved one needed options.
I inhaled everything I could find about non-drug options. As weeks turned into months, my initial desperation became rimmed with a band of hope. To my amazement, submerged in this research was a treasure trove: thousands and thousands of gold-standard trials that support the use of non-drug approaches for mental health recovery.
Research Says: Non-drug Options Work
After examining over 4000 studies, and hundreds of meta-analyses, I surfaced from my research and was hit with a startling “Aha” moment: non-drug approaches really work.
They generally offer significant symptom reduction, and in some cases, full remission. They have a side effect profile that is dramatically better than drugs: usually none, or quite mild.1 Unlike drugs, many non-drug approaches target known causes and influencers of mental health issues, not just symptoms. And these approaches help people achieve sustainable wellness.
Non-drug approaches, however, are no panacea. Some approaches work better than others. Some have very strong evidence, others suggestive. Some people don’t get any benefit from certain techniques, while others find them life-altering. Such is the nature of our individuality.
But non-drug approaches are also no fad. They are validated by disciplined peer-reviewed studies. They’re also more than theory. A growing number of practitioners embrace and heal with Integrative Mental Health — a discipline that uses the best of conventional psychiatry and non-drug options.
From Symptom Relief to a Wellness Continuum
Surprisingly, there are so many non-drug approaches that we need an organizing structure to make sense of them all. The U.S. Institute of Medicine and European Union of General Practitioners/Family Physicians2 offer such a framework — a wellness continuum with four categories of care:
- Preventive: Wellness practices that help avoid mental health issues.
- Restorative: Approaches that reinstate mental wellness by addressing root causes.
- Symptom Relief: Methods to minimize mental health symptoms.
- Over-Care Avoidance: Ways to avoid unnecessary and potentially harmful treatment.
Sorting the large basket of non-drug approaches and pouring them into the wellness continuum, the following picture emerges.
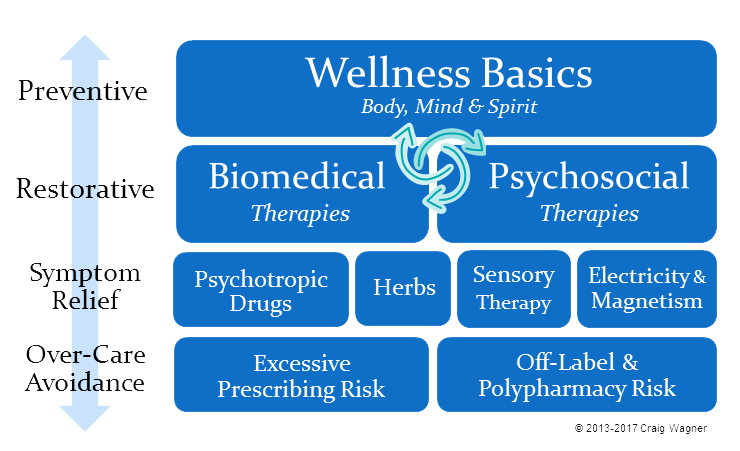
Viewing recovery approaches in this context broadens our perspective and helps us see the forest, instead of the trees. It helps us…
- Avoid drug myopia. Drugs are one piece of the puzzle, not a necessary centerpiece.
- Think wellness. Move from a narrow concept of symptom relief to a broad strategy of well-being.
- Choose from a broad menu of options. You and practitioners can select approaches to build an individualized recovery plan to fit your unique bio-individuality, history, and preferences.
Interestingly, the continuum’s last pillar — over-care avoidance — is a cautionary one. Since psychiatry has the powerful hammer of drugs, most mental health conditions, and many normal life situations, begin to look like nails. This pillar reminds us that hammers can both build and destroy.
A Large Menu: 27 Non-drug Approaches
Pulling back the covers of the wellness continuum reveals 27 broad non-drug options.3 These can be best understood by considering them in the following groupings.
Wellness Basics help minimize and avoid mental health issues. Exercise, a nutritious diet, healthy digestion, calm awareness, restful sleep, a safe home, inner grounding, meaningful activity, and social interaction are just a few important basics. Thousands of studies show that these fundamentals have a profound effect on mental health.
Biomedical therapies address many physical issues that impact mental health. These therapies are important since over 25% of mental disorders are caused by or significantly influenced by physical issues.4 For lower socioeconomic status individuals, the figure approaches one-half.5 Although a biomedical analysis is required in the psychiatric differential diagnosis process, it is rarely conducted thoroughly.6 Robust biomedical testing should be considered mandatory. It may allow precise targeting at root causes: food allergies, gut microbial imbalances, pathogens, hormonal irregularities, environmental toxins, inflammation, oxidative stress, and more.
Of particular promise is Walsh-protocol nutrient therapy. It looks deep into each umbrella diagnosis and identifies an array of different bio-types, each requiring a unique therapeutic response. Over 70% of people receiving individualized nutrient therapy gain substantial symptom improvement — sometimes complete remission — across many diagnoses, often accompanied by a significant reduction in psychiatric drug dosages.7
Psychosocial therapies address trauma, stress, emotional difficulties, unhelpful thinking, and more — all of which impact mental health. These therapies work as well as or better than drugs for depression, anxiety, obsessive-compulsive disorder, and post-traumatic stress disorder; and are helpful in avoiding bipolar relapse.8 Dialectic Behavioral Therapy is the go-to treatment for Borderline Personality Disorder.9 Open Dialogue offers great promise for first episode psychosis. And none of these have psychotropic side effects.10 Even though these approaches are effective, they are seldom used.11
Symptom Relief goes well beyond drugs. Every diagnosis has associated herbs that can provide relief. A variety of calming sensory therapies aid many diagnoses. And a set of new electrical therapies deliver symptom relief with micro-currents 200 times less powerful than electroconvulsive therapy, from cell-phone sized devices, with no cognitive side effects.
Over-care avoidance works to avert the significant risk of three common psychiatric practices: off-label prescribing (using drugs in ways not validated by FDA trials), polypharmacy (using more than one drug for a particular disorder) and over-prescribing (giving drugs when not medically warranted). Remarkably, 94% of psychiatric off-label prescribing has little or no scientific evidence supporting it.12 Outcomes from antipsychotic polypharamacy,13 and overprescribing for the elderly,14 are particularly grim. Recognizing these risks, the American Psychiatric Association15 and multiple U.S. public health organizations16 work to curb these practices.
Good News, Bad News, and a Bit of Heresy
The good news is that there are practitioners today who are skilled in using non-drug approaches. They have many titles: integrative psychiatrist, functional medicine practitioner, naturopath, therapist, psychologist, neurogastroenterologist, endocrinologist, and more. In many ways, these practitioners form the leading edge of psychiatry. They hold a much broader menu of recovery options than conventional psychiatry. These practitioners respect the value of drugs, especially in crisis. However, they seek to enhance core wellness through non-drug approaches.
The bad news is that there aren’t nearly enough of these practitioners. Their care is often only partially covered by medical insurance, if at all. By necessity, they focus on only a subset of the total menu of options, requiring coordination of care across multiple practitioners. Additionally, many non-drug approaches aren’t valued in the DSM — the U.S. psychiatric bible — so using them may be at odds with conventional mental health practitioners.
Individuals with mental health challenges articulate a recurring theme, an urgent plea, and a critical demand: people need options. Drugs simply aren’t enough.
After swimming in this research, I submit a bit of heresy: we have a cornucopia of options. Although research must continue, the major task before us is not creating more options. Rather, we must…
- Understand and respect the benefits of the non-drug options already in hand
- Use robust biomedical and psychological evaluations to inform non-drug therapy selection
- Alter the DSM to elevate non-drug treatments based on their evidence
- Train practitioners on their use
- Eliminate the many barriers that curtail access
- Reorient our time, enthusiasm, and resources to make them available to those in need
Nobody said this was going to be easy.
Joining the MIA Tribe
The path ahead is long and crooked. To make progress, we must change our consciousness about non-drug treatments. They aren’t quackery. They are potentially life-altering tools. They aren’t perfect, but they work. Changing this consciousness is a part of MIA’s “rethinking psychiatry,” a prelude to the herculean effort of reconstituting psychiatry.
I’m excited and humbled to join the MIA band of contrarians with this, my first post. Let us be both a burr under the saddle and a beacon in the darkness. Both are required for progress.
I thank Robert Whitaker for being the galvanizing force of MIA and giving me a voice within it. Much good is being created here. I will work like hell to add to it.
Epilogue: Once I realized that non-drug approaches worked, my head reeled with cognitive dissonance. Why are so few practitioners using them? After all, good research, like nature, abhors a vacuum. Why wasn’t this research spreading like wild fire? Over time, the answer hit me. There are few nefarious bad guys, no lack of willing ears, and no paucity of smart people. Rather, there is an overabundance of the one thing that always seems to oppose good ideas: a mountain of institutional inertia.
Thankfully, we don’t need to fight all of that inertia right now. Instead, we must navigate that inertia with a little Sun Tzu indirection to enable our victory in the art of war that is personal recovery… But that, my friends, is a worthy subject for an upcoming post.














Regarding the answer of “a mountain of institutional inertia” for “Why are so few practitioners using them?(non-drug approaches)
I disagree. The answer is simply what would a psychiatrist-doctor be without medicine(drugs)?
What would distinguish them from a doctor of divinity?
“To distinguish himself from the doctor of divinity, the doctor of medicine could not simply claim that he was protecting people from sin, or vice as Rush put it. Badness remained, after all, a moral concept. As medical scientist, the physician had to claim that badness was madness, that his object of study was not the immaterial soul or “will”, but a material object, a bodily disease. ” Szasz http://jme.bmj.com/content/27/5/297.full
Drugs are ideal, as they have to be continually applied to the patient/prisoner/slave. Where with chains, the chains are only issued one time. http://www.bbc.com/future/story/20160612-heres-the-truth-about-the-planned-obsolescence-of-tech
Report comment
I agree, This goes well beyond inertia – there is active resistance to the very idea that non-drug therapies can ever be anything more than ancillary support. This is true because the drug and psychiatric industries DON’T WANT PEOPLE TO GET BETTER OR EVEN CONSIDER OTHER OPTIONS BECAUSE THEY LOSE CUSTOMERS! The medical profession in general practices similarly, but they are at least required to show some kind of physiological indication that the body isn’t working properly, whereas psychiatry has been allowed to simply invent “disorders” and re-define the entire field and control the terms of discussion in very self-serving ways.
And there ARE absolutely nefarious bad guys. There may not be that many, but they are in positions of huge power and influence, including the ability to spread dollars around to support their model of reality, despite all evidence for better ways of understanding the truth.
Consider the “Open Dialog” model. It’s been around since the 70s! It has much better outcomes than any other approach, even if you accept psychiatry’s subjective definitions of “schizophrenia.” But efforts to promote this approach led to nothing, even in Finland where the approach was well known. This isn’t inertia – they intentionally suppressed this information and removed the effective approach from most Finnish hospitals. Same thing happened to Loren Mosher. These are not benign forces. They actively suppress any attempt to redefine “mental health” in any way that cuts into their profits and their control of the “mental health” market.
Report comment
Steve, thanks for the comments. I think we are a lot closer in thought than it seems.
Yes, these are far from benign forces. They are powerful forces that resist change in many dimensions. There are forces in drug companies seeking profit, forces in insurance companies seeking to reduce cost, forces to keep the DSM symptom-based, forces in medical schools that resist providing meaningful training of non-drug training, professional forces that impact practitioner reputation if they step too far outside of the envelope of conventional care, financial forces that make it more lucrative to prescribe drugs than deliver psychotherapy, malpractice forces that keep practitioners fearful of doing things outside the guidelines of the DSM. And more.
I think the challenge here may be my use of the word “inertia” which may seem to be similar to “benign”. My use of the word “inertia” here was an effort to underscore the strong resistance to change in many major institutions. I would never call these forces benign (i.e. unharmful). I think we all see the combined harm they do.
In a comment down below, I speak a little to my belief that we need to change our collective consciousness and embrace non-drug solutions and flood the practices of practitioners who share this consciousness. At an individual level we can choose to simply walk away from the drug model. Yes, that is hard for a number of reasons, especially financial. But, is it easier to counter all of these huge forces, or simply start starving them of oxygen? I think the latter, though that too is a long and difficult road.
Report comment
Inertia to me implies continuing to move in a direction already selected due to lack of sufficient force to divert one from this course. It’s very passive. Whereas active opposition is a force that attempts to push the profession in a certain direction in opposition to other forces. Inertia certainly comes into play, but there’s a lot more going on. And yes, it sounds like we agree on most all points, which doesn’t surprise me at all.
Thanks for the response!
— Steve
Report comment
It takes at least 40 years for new medical paradigms to replace the old ones. James Lind figured out how to treat and prevent scurvy 40 years before the Royal Navy began to keep limes (remember the limeys?) on ships (it had to blockade France during the Napoleonic wars), and he was a surgeon in the Royal navy.
Report comment
Right, reminds me of Rudolph Semmelweiss, who cured childbed fever in the 1800s by having doctors wash their hands before before “helping” deliver babies (some apparently came straight from cadavers to the maternity ward!) He reduced the rate to almost zero and then was fired from his hospital for insulting doctors by implying that they were killing their patients with their dirty hands (which, of course, was 100% true!) He spent some time in the asylums of the time because it infuriated him so much to be proven 100% correct but to be stopped by convention, arrogance, and lack of concern for the patients’ welfare.
It’s not a new problem.
Report comment
What markps2 said.
Report comment
For therapists who actually want to help the emotionally suffering these would be great. But psychiatrists would be obsolete, because all these non-drug remedies could be applied by folks with MSW’s and PhD’s in psychology. No doctors necessary!
I have wanted to get my Master of Social Work and become a certified therapist. Then I could learn Finnish Dialogue therapy and one or two other methods that can actually help people instead of disabling them for life.
That would only be with their consent of course! 🙂
Report comment
You’re right about inertia. Cold canvassing for a complementary practitioner can easily become an exercise in watching otherwise distinguished practitioners making peculiar contorted faces when you bring the subject up with them. The Canadians have an advantage here. Their orthomolecular web site lists pages of them for every province.
Report comment
Amen. Canada, Australia and some of Europe seem to be leading the charge here. Interestingly, the legacy of orthomolecular does live on in the U.S. through the lineage of Hoffer to Pfeiffer to William Walsh (www.walshinstitute.org). There is a directory of Walsh-trained practitioners at their site. Walsh’s Nutrient therapy is based on earlier orthomolecular approaches: nutrient imbalances, food allergies, hormonal irregularities, gut/digestive imbalances, heavy metals, etc. Walsh extends that foundation to consider epigenetics, oxidative stress and more. In my personal situation, we live near the border and we ended up in Toronto to find an orthomolecular practitioner.
Report comment
I was mentally ill for 67 years. I was diagnosed with Bipolar 2, OCD, PTSD, & Anxiety disorder. Three years ago I got onto an orthomolecular site and have been taking the supplements. As a recovering alcoholic I read Bill W’s article Emotional Sobriety and related to it. I read Wayne Dyer’s book There’s a Spiritual Solution to Every Problem and used his meditation CD I AM. I cut sugar out of my diet using kefir. I have been free of mental illness for three years now. I had 35 years of thereapy including analysis. After a suicide attempt 7 years ago I got a new psychiatrist who saw me for 30 minutes a month untill I stabilized. he was kind and supportive, treated me like a peer rather than a patient and now I don’t see him at all as I’m well. It’s like a whole, new, wonderful world.
Report comment
PhoenixRising, Congrats on your three years! None of this is cookie cutter. We each have to find our way by experimenting with approaches that match our bio-individuality, history and preferences – most often guided by practitioners we trust. It sounds like you found the right combo that works for you. Hearing your story is a jolt of juice for me. It helps me retain my enthusiasm to continue doing this.
Report comment
PhoenixRising writes:
I was mentally ill for 67 years. I was diagnosed with Bipolar 2, OCD, PTSD, & Anxiety disorder. Three years ago I got onto an orthomolecular site and have been taking the supplements. As a recovering alcoholic I read Bill W’s article Emotional Sobriety and related to it. I read Wayne Dyer’s book There’s a Spiritual Solution to Every Problem and used his meditation CD I AM. I cut sugar out of my diet using kefir. I have been free of mental illness for three years now. I had 35 years of thereapy including analysis. After a suicide attempt 7 years ago I got a new psychiatrist who saw me for 30 minutes a month untill I stabilized. he was kind and supportive, treated me like a peer rather than a patient and now I don’t see him at all as I’m well. It’s like a whole, new, wonderful world.”
All those labels and mentally ill for 67 years huh. Looks like they did a good job of keeping you in the disease role (with the best and kindest of intentions of course) and you had to play along.
And as for that kind and supportive peer-treating psychiatrist, I’ve seen a few like them before. Their kindness is limited to being nice to you. They never ask “Why the hell did you have to do this for 67 goddamn years?”. That’s something that puts them in professional jeopardy.
I also wonder if they prescribed you SSRIs for “OCD” due to which you experienced mania and were subsequently labelled bipolar. I may be wrong about the last 2 lines though.
Report comment
I like this article, Craig, but your chart is wrong. On the line “symptom relief” (I dislike the word “symptom”) you have a number of possible solutions: psychotropic drugs, herbs, sensory therapy and electricity and magnetism. Unfortunately you haven’t included “psychosocial therapies” on this line. I suggest you take a look at the ISPS-US map on this subject, the Moving Forward map: debategraph.org/imfev. It might give some ideas. I also note from your bio. that you are employed by the American Psychiatric Association to communicate “alternative” mental health information. I must say I think of the non-drug therapies that have been proven to work for people in distress as *competing* therapies, not “alternative.” “Alternative” has that horrible overtone of “not-official” and I’m sure that’s not what you mean to communicate here.
Report comment
David, thanks for the link – interesting material there, and the interactive graphic approach lends itself to a much more nuanced representation than the 2D grid can represent… There are a lot of different ways to represent the mass of approaches. I strove for one as simple as I could make it without sacrificing too much nuance.
Certainly the psychosocial therapies reduce symptoms, and do it well. The distinction I was trying to highlight is that the psychosocial/biomedical therapies have a much stronger ability to strike at causes than do drugs. In the process, they relieve symptoms. In general, the diagram hopes to show that we should work as “high” in that diagram as possible. First, do as much tier 1 preventive as is reasonable. If symptoms, exist then look to tier 2 psychosocial/biomedical to strike at causes. If that isn’t enough, consider things in the tier 3 “symptom relief” category to address the residual symptoms not addressed by the restorative approaches. And all the while, avoiding excess tier 4 intervention. Realistically, we’re often doing things in all 4 levels simultaneously.
You raise the interesting point about “competition” between therapeutic approaches. In reading the literature, I do sense a “competition” between the two APAs. Hopefully we can evolve to a point where all of these therapies, including drugs, are seen as available options where the benefits, warts and unknowns of each are clear. I think that is the vision of integrative mental health..
I volunteer time to (not employed by) the APA caucus on Complementary, Alternative and Integrative Medicine (CAIM). These are talented psychiatrists working to mainstream many of these non-drug approaches. They use the three big terms for this body of therapies (“complementary”, “alternative”, and “integrative”). I think I agree with you, “alternative” is the one that carries the most negative overtone.
Good interaction, thanks for the insight.
Report comment
Craig,
This is a great post – nice to see a broad 30,000 foot view of options that can help with emotional distress. The key point I took away from this is that drugs are just one option among many, not the centerpiece of treatment necessarily – and this should include experiences that get labeled “schizophrenia” and “bipolar”, in my view. From reading most mainstream material, you would think drugs should be 70-80% of the treatment for serious distress… whereas really, they should probably at most be 10-20% (or sometimes 0%) of an integrative approach that addresses what can help a person in many spheres and on many levels.
One criticism – DBT may have more short-term research due to its branding, but it’s not necessarily better in any way over the long term for people labeled “borderline” (a meaningless, vague label anyway) than other approaches. A lot of survivors hate DBT because of its concretization of labels and its directive, simplistic approach. So I don’t think you should put it out there as the primary approach for a vague label like this. Here are a couple of ways to rethink this issue:
– Intensive Long-Term Therapy can have really good results for trauma that gets labeled “borderline” – https://bpdtransformation.wordpress.com/2015/02/13/22-proof-that-borderlines-are-motivated-for-psychotherapy-and-can-fully-recover/ – no DBT study has these kind of long-term results over years, that I’m aware of.
– BPD should be abolished as a label and replaced by a more continuum-based, non-stigmatizing way of describing serious distress: https://bpdtransformation.wordpress.com/2015/06/26/26-why-bpd-should-be-abolished-and-what-should-replace-it/
These links above are from my personal site about part of my traumatic experience.
Borderline Personality is not a thing people have, just a flawed label for experience people may have at one time and become free from later. These labels are a conundrum and most of the studies on them are, admittedly, biased in various ways by the observer’s input.
Report comment
Matt, cool, thanks for the links on BPD. Time for me to inhale more research.
You touch on a point that I think is vital here… “From reading most mainstream material, you would think drugs should be 70-80% of the treatment for serious distress”. The research supports using a much wider menu of options than drugs. Fortunately, the number of practitioners who are embracing non-drug approaches is growing.
Report comment
BPD should be abolished as a label and replaced by a more continuum-based, non-stigmatizing way of describing serious distress
Saying “BPD should be abolished as a label” implies that other labels are more legitimate. How about “serious distress” as a way of describing serious distress? Then again, maintaining “professional” status requires the mystification of no-brainer situations, and the reduction of thought, feeling and behavior to categories, “medical” or otherwise.
The idea that destructive attitudes and practices need to be replaced rather than eliminated is a fallacy.
Report comment
Oldhead,
There is a way of thinking about serious distress that goes from, roughly…
– a “younger”, more developmentally early, less mature way of thinking and feeling, sometimes called presymbiotic phase, and which involves seeing things as all-good or all-bad, and confusing what is oneself and what is other people
– through various phases up to an older, more mature, more integrated/ambivalent way of processing relationships and situations (called individuation / separate sense of oneself and other)
I think there is some reality to these continua in how people experience their relationships and lives, very generally speaking. Mahler, Stern, Schore, and others who’ve seriously studied mothers and children and what helps children grow up to be fulfilled adults, have done good studies of these ways of relating and not pathologized the problems as much.
The question is what to call these experiences, and how talking about it can not be destructive to label or discuss common experiences.
Report comment
Certainly not my question.
I think the answer is for those who want to make careers out of dissecting, analyzing and labeling others’ misery as a “specialty” to spend more time minding their own business, and pursue philosophy/psychology as a hobby, rather than a source of sustenance. The roots of almost all these problems are political, but there’s definitely no money in acknowledging that or actively trying to eliminate misery at its source.
Report comment
Every possible career have originally grown from the misery of others.
Report comment
Did you read the whole comment? Most careers are not based on fraud.
Report comment
BPD is one of those “diagnostic” terms for the- “I haven’t the faintest idea but it must be something” form of diagnosis that has the vital mission of determining insurance categories for payments and the even more vital one of lining the diagnostician’s wastebasket.
Report comment
Addiitionally, the BPD wastebasket is used to cast aside people in distress because “it’s too hard,” and “they don’t respond to regular treatment” (treatment being drugs and DBT).
I have known many people who got cast out of programs once this label was stuck on their file, left to their own devices and distress, with a pile of drugs to insulate them from suffering that nobody was willing to help with.
It is one of the uglier “diagnoses.” They are all ugly and fictional to be sure, but labelling someone as “Borderline” is a fast road to marginalization, suppression, and oppression.
Report comment
Borderline Personality is a label they pin on you for punishment for behavior they call “manipulative.” All psychiatric prisoners have to resort to manipulation from time to time. When you are trapped in a coercive relationship (especially an abusive one) manipulative behavior is a necessary survival skill.
If you escape the coercion, no manipulation is necessary. BPD melts away like magic! Too bad the label doesn’t.
Report comment
First off, I don’t think over drugging an instance of ‘over care’. I don’t think people are drugged to excess because people ‘care’ for them. Now what is actually going on there, I leave to your own best judgment, as well as your imagination.
“After examining over 4000 studies, and hundreds of meta-analyses, I surfaced from my research and was hit with a startling “Aha” moment: non-drug approaches really work.“
One could turn this equation around, and say that after looking at all these meta-analyses one thing is clear: drugging doesn’t really work. What it results in, as a rule, are negative outcomes.
I would like to see ‘non-drug options’ applied, but my experience has been in the public mental health system, and there, any approach besides and beyond ‘drug, drug, drug’, still has a long way to go. The ‘learning curve’ is a steep one, and social factors, among mental health professionals, among others, are the big impediment here.
“Non-drug options” may not be a panacea, however mental health professionals still, and despite much evidence to the contrary, treat “drug options” as a panacea for so-called “mental disorders”. This has created a major physical health risk for anybody serviced by the public mental health system. “Over drugging” is the rule, and it’s maiming and killing people within that system.
I wish you luck when it comes to changing things within that system, I just want to point out that piece-meal changes aren’t likely to do a whole lot of good, not when what we need is a radical paradigm change of approach across the board, and that’s something that, at present, is very far removed from the reality.
Report comment
Drug “treatment” is quick and requires little effort for the prescriber and teaches the person taking the drugs nothing and certainly does not empower self-healing and self-efficacy. Healing is work and requires effort on both sides.
Dialectical Behavior Therapy is a great package of skill teachings using Eastern philosophy and cognitive behavior techniques for solving interpersonal conflict and emotional regulation difficulties.
It is a lot of work, too many acronyms and can burn people out. I like adapting it and incorporating parts of it in my practice. I agree with Matt about diagnosis of Borderline Personality Disorder and how the label has been used rather punitively by providers. We did a lot on training on adolescent psychiatric state hospital around empathy and strength based language for the staff. Just not useful nor kind. Certainly countertransference issues working with those who are in emotional distress but answer is good supervision, self-care and better training.
Eye Movement Desensitization and Reprocessing (EMDR) not mentioned in article is a good trauma therapy using cognitive reprocessing and neuroscience. Mediation and visualization uses hypnotic induction to create more relaxed states and used for increased productivity and goal setting. Expressive therapies including music, drumming circles, art therapy and writing are also beneficial. And of course having positive, nonjudgmental supports of family, friends and co-workers is needed. Meaning roles like being a good parent, caregiver, volunteer and paid employment are also therapeutic and make one feel a sense of purpose to their lives. We all need to feel loved and important.
Report comment
Knowledge is Power (like your handle)
Yes, EMDR, meditation, mindfulness, music, journaling, meaningful social interaction and many others are effective – they all have their place in that broad clustering of 27 non-drug options. A number of people have been helped with Emotion Freedom Technique as well. Good to hear your consensus with Matt on BPD – I had not heard that perspective before.
Report comment
Any knowledge or experience with transcranial magnetic stimulation? I remember being the in a seminar with a MD/PHD trying this out himself in 2001 when I was in training at Menninger. I had not have any clients yet it. It was touted as the alternative to ECT for those with depression.
Report comment
KIP, Overall the evidence is not compelling. Some studies show promising but inconclusive evidence for rTMS for depression, but it has not been shown to be effective for OCD, PTSD or SZ (2005, PMCID: PMC2993526). The 2002 Cochrane meta-analysis of 16 rTMS trials for depression found no strong evidence of benefit from using rTMS—“although the small sample sizes do not exclude the possibility of benefit.” (http://goo.gl/Ea9sBY). A 2015 Cochrane meta-analysis of 41 trials for SZ found insufficient evidence to support or refute the therapeutic use, noting that overall quality of evidence was very low, due to risk of bias (http://goo.gl/34zSX8).
Although not extensively studied, I think of greater promise are tADS (for OCD), tDCS (depression and SZ) and CES (depression and anxiety). All are inexpensive in-home devices.
Report comment
Thank you, Craig, very helpful. I wish you much success in your work and look forward to more posts at MIA from you. Susan
Report comment
Thanks for your contribution Craig. I am a psychiatric survivor. I also read Psychiatric Times. I have noticed that in the last few months there has been a noticeable shift there. Yoga, deep breathing, and other non-drug options are getting almost equal airtime to traditional psychiatric approaches. In fact, one such article discussed magnesium and zinc as being great for mental health. Two others discuss Omega-3. I am supplementing with these now.
Six years ago, I began my odyssey through psychiatry. The results are nothing short of catastrophic.
I applaud your efforts leading the charge to more integrative, non-pharmaceutical care.
Welcome to MIA.
Report comment
Randall, thanks for the comments and warm welcome. Yes, there is a paradigm shift underway toward integrative health as people begin to see the tremendous value of non-drug solutions. That is really good to see. Unfortunately, its not nearly as fast as any of us would like. But, as individuals, and as psychiatric survivors, we can seek out these alternative treatments even if conventional psychiatry does not.
You mention zinc… Zinc/Copper balance is really important for mental health and is one of the fundamental tests done in the Walsh nutrient protocol (see footnote #7 in this post if you are interested in his book). Yes, Omega-3s are important and so is gut health with probiotics.
Good luck on your odyssey. The good news is that you are grabbing the self-determination to make your own therapy choices. Hopefully you can find good practitioners who can help.
Report comment
This article is a healthy reminder of why I rarely visit this site now: the casual embrace of anything non-drug as benign, evidence-free endorsement of many of these “therapies”, and the continuing pathologization of human experience in new clothing. And yet another person trying to make a buck out of all of this.
Report comment
I can see your point, Sally, in naming and explaining overintellectualized therapies it appears and certainly has the potential to dehumanize. I do not espouse psychopharmacology or psychotherapy wholeheartedly. I hope for a time when people are just able to be present and care for another without ever the need for a paid professional. I pray that no one ever needs to be hospitalized or medicated. I can honestly say I did not become a clinical social worker and psychotherapist for the money. I wanted to understand and help alleviate human suffering. I did study many types of therapies with distinguished clinicians and psychoanalysts but just tools. When you sit face to face with a child who has been abused or an adult with delusions and hallucinations those theories and techniques are just that. The human connection is what heals.
Report comment
I agree. The human connection is indeed the healing part, and it’s the luck of the draw whether you get that from a professional. What’s more you don’t need to be a professional to provide it.
Report comment
Absolutely not, Sally. Let’s hope that each of us takes on the responsibility of creating a more just, compassionate and connected world. Much work to be done on many frionts. Blessings to you on your journey.
Report comment
Hi Sally, thanks for the comments. Like you, I don’t want to recommend anything that doesn’t have evidence. To do so would be fairly irresponsible. In the short space I had in this article, I couldn’t get in to all of the detailed evidence that exists for these non-drug therapies. Some have great evidence (e.g. Omega-3, Vitamin D, CBT, etc.). Others are weak. For instance, although many people swear by it, the evidence for the effectiveness of homeopathy is fairly weak, so I don’t recommend that as a starting place for recovery.
To try to get to the root of this variable degree of evidence, I propose non-drug solutions in three tiers: Tier-1 is well-proven with good meta-analyses, Tier-2 has a number of good studies, and Tier-3 is more suggestive. If you are interested in what that looks like, consider checking out the prioritized non-drug treatments for depression, anxiety, schizophrenia and bipolar (https://goo.gl/XwsgkZ).
Report comment
Wow all these italics are annoying. Anyway I think I agree, at first I thought you were coming from a pro-drug position but your comment about pathologizing experience dispels that notion. It’s the entire context that’s the problem; I think we’re on the same page here.
Report comment
I think you were responding to me, oldhead? Yes, we’re on the same page, for sure. Putting an end to drugging is just part of the problem, and probably not the biggest part. As you say it’s the entire context, the framework.
Report comment
Yes.
Report comment
Hi, Craig, thank you for clarifying that you volunteer to work with CAIM of the American Psychiatric Association and are not employed by them. I apologize for the error.
I read in other comments attached to your article that someone has seen that in Psychiatric Times lately: “Yoga, deep breathing, and other non-drug options are getting almost equal airtime to traditional psychiatric approaches.” This is a good sign. Perhaps more psychiatrists are now “woke” in the parlance.
But like that “woke” right-wing radio host, the history of mainstream psychiatry is recorded and is unescapable. You only have to read accounts of what are labeled “Psychiatric Torture” at the Center for the Human Rights of Users and Survivors of Psychiatry (chrusp.org), the Everyday Horrors of the Mental Health System (http://psychrights.org/horrors.htm) at PsychRights, and the personal stories revealed here at Mad In America and many other places. In fact, to bring it back to Mad In America, in a recent interview article, one psychologist identified two psychiatrists, one who did this:
“What was interesting was I saw a number of psychiatrists’ kids who were seriously troubled — it wasn’t always psychosis, also other diagnoses — because I was the only one in the area who didn’t use medication and the psychiatrists didn’t want their kids on medication. This included the children of a psychiatrist who treated kids and used medication for all the kids in his practice, but he didn’t want his own children on anything. So that was interesting.”
and another who moved away from psychotherapy for this reason:
“I found out later he stopped doing psychotherapy and was only prescribing drugs. I ran into him at a restaurant one day and asked him why he stopped doing therapy with patients. He said, “As a psychiatrist doing psychotherapy I can charge about $200 for a one hour session… if I medicate, I can see four people for 15 minutes each in the same amount of time, for $800 per hour. And if I shock people, I can charge $1500 a pop and it only takes 15 minutes. Do the math, do the math.” And he walked away while I just stood there. That’s the name of the game for most psychiatrists and most pediatricians.”
So, no, the problem is not one just of inertia. The bottom line is that mainstream psychiatry is now in very bad shape for lots of reasons. You have many hundreds of thousands (millions?) of people on powerful brain-altering drugs for no scientific reason and there doesn’t seem to be a way out for mainstream psychiatry.
But there is a way out. It’s Proposal (1) on the ISPS-US Moving Forward map and here’s a direct link in Outline View: debategraph.org/prop1sum. I will explain it briefly here and you can look at the detail if you’re interested. What is another major problem with mainstream psychiatry? It does not and never has cured anybody. Unlike any other branch of “medicine” mainstream psychiatry has never cured a single person. All it does is create patients. Now imagine that the reverse happens. A patient is put on drugs, is on them for a time and is then weaned off them, taking into account there may be withdrawal effects. They are re-examined and pronounced “symptom”-free. Is this not a cure? Is this not what mainstream psychiatry wants? To stress the obvious: I don’t believe in mainstream psychiatry at all, but if mainstream psychiatry wants a way out of the dilemma it’s in, here is one way. And perhaps we need a “Truth and Reconciliation Commission.”
Finally, I hope that your reading of the articles here at Mad In America convinces you to volunteer to work for a non-psychiatric organization. Communicators of your calibre are sorely needed. Blue is a great choice for the diagram, by the way. The color of the sky, an “over-arching” approach… Was that deliberate? I’m guessing so. (But I still, as I said in my earlier comment, disagree with the chart itself).
Report comment
I was the one that quoted psychiatric times. What will psychiatrists do with the new integrated and functional approach? You don’t need a prescription to attend a yoga studio. You don’t need a prescription to go to Whole Foods and get zinc and magnesium. Their heyday is coming to an end. Whitaker et al have exposed them
Report comment
David, thanks for the good thoughts. Like you, I think conventional psychiatry is horribly broken.
Like many on this site, I have struggled to figure out how to maximize my personal impact in a mental health environment where much is severely broken. Where to place personal bets? I think there are three primary options: 1) vigorously work to change these broken systems from the outside 2) try to change the broken systems from the inside, 3) ignore the broken systems and create afresh hoping the old systems will die from Darwinian disuse.
The existing mainstream psychiatric systems are entrenched, rich and strong. Sun Tzu will tell you that mounting a frontal attack against a stronger opponent is fraught with difficulties. We in MIA are experiencing that difficulty in spades as we hear from many people who post that people don’t see change despite our efforts. But I think we are at least changing the conversation and must continue.
I’ve decided to straddle options 2 and 3. For option #2, I’ve looked for the good within NAMI and the APA and tried to make that good better. I think it is short-sighted to fully demonize both organizations. If we do, we become as close minded as those we hope to change. For instance, the NAMI family-to-family training puts a heavy focus on drugs as the therapeutic solution, but offers good material on self-care, communication, the downsides of drugs (yes, they spend ample time talking about that) , etc. I’m not in a position to change the courseware to reduce its drug-centricity. It will continue to be taught regardless of what I do. What I can do is respect the people in the local NAMI affiliates who are trying to help (I would go to war with some of them), respect the parts of the training that doesn’t talk about drugs (which is most of it) and gain their trust so that they allow me to augment their training with non-drug information. So that is what I do. And that non-drug part of the material is always very well received. If I screamed at NAMI for their drug-centricity, I couldn’t get in the door because I refused to respect what they do. My screaming would result in harm – in the form of not getting information to people in need – to the very people I’m trying to help.
For the Psychiatric APA, I volunteer with the caucus on Complementary, Alternative and Integrative Medicine. These are psychiatrists who are vigorously trying to help people with non-drug options. They are trying to change their flawed organization. These are admirable men and women who have found their chosen profession in dramatic disrepair and are trying to do something about. I’ll support these contrarians.
But my major focus is #3. We need talented and caring people who can simply define and execute in a new way and don’t give a hoot about all the flaws in psychiatry. A great example is Open Dialogue. They have found a strong solution for first episode psychosis and they are just doing it. They are healing at a dramatically impressive rate. They are publicizing their success. They are moving their success around the world. They are ignoring mainstream psychiatry and mainstream psychiatry can’t do anything about it.
The end game that I think is possible is this. We as mental health “consumers” must shift demand. We need to understand that alternative practitioners (psychologists, naturopaths, integrative psychiatrists…) are where the healing is at. We need to flood their practices with people. As we do this, they are going to hire more PAs and talented practitioners to expand their practice so the supply of the right kind of practitioners increases). To the greatest extent possible we should simply ignore mainstream psychiatry (unfortunately, you can’t under court ordered treatment and if you go to the ER).
In order to get people to ignore mainstream psychiatry, we need to change their consciousness, helping them understand that there is a far better answer. So my goal is to change that consciousness and shift demand. You bring down the wrong thinking of the Psychiatric APA not by overpowering it on a frontal assault, but by starving it of oxygen.
David, as you suggest, it is important to work outside the mainstream. At Safe Harbor, we focus on primarily the proven biomedical (food allergy, nutrition, toxicity, pathogens…) that can cause mental health symptoms and are decidedly un-mainstream. My book is decidedly un-mainstream too. So we’re birds of feather there.
At a larger level we need to shift the balance of power between the two APAs. From an outsider’s perspective, the Psychological APA has the right solutions, but doesn’t have the power of the Psychiatric APA. The Psychological APA lacks the badge of MD, so people think practitioners of the Psychiatric APA are the true “experts”.
Report comment
People seem to miss the point entirely. The answer is to disqualify psychiatry as a field of medicine, prosecute those who practice it as such, and address the socioeconomic/political issues which create such suffering in the first place.
Psychiatry has a choice of “ways out” — it can use either the front or back door.
Report comment
Also, we are once again subject to the notion of psychiatry being “broken.” I shudder to think of the consequences if it were “fixed.”
Report comment
Craig Wagner, your 27 non-drug options are all based on the same lies.
https://sites.google.com/site/onwardmentalhealth/27-non-drug-approaches
You are saying that if you just fix things in the present, then everything is fine. Well that does not restore a survivor’s biography, it does not vindicate them.
So the lie is, you can live a good life without having to redress historic abusers and others like them. All it amounts to is converting angry abuse survivors into abuse survivors in denial.
You are either helping abuse survivors to get justice and be vindicated, or you are taking advantage of them by pedaling a dangerous set of lies.
Nomadic
Report comment
In a funny little ‘twist of fate’ irony, I edited a NAMI newsletter for a couple of years. I was a working, professional medical editor and fell into it as a volunteering-in-my-community gig. I had no personal connection to the organization and had never heard of it.
Fast-forward, two cities and over ten years later I had a child who was poised to be diagnosed as ‘IED’ and ‘ODD’ (I don’t even think those so-called ‘disorders’ existed when I was editing for NAMI). Knowing what I did about NAMI and its families – a sort of pay-for-play organization, hand-in-glove with psychiatry, with some well-intentioned people and some less so – sent me running the OTHER way.
Every single intervention I’ve used to help my child develop over the past ten years has been non-drug and outside the purview of the medical and psych establishments. Many are listed above, some not, and some age-appropriate ones I concocted as I went along. I never once considered using pharma drugs. (On a child’s developing brain? Obscene.)
It’s by no means easy to go the no-drug route in a society where families like mine have no support, but it’s the only responsible and conscious choice.
Liz Sydney
Report comment
Liz,
“It’s by no means easy to go the no-drug route in a society where families like mine have no support….”. Absolutely. It is hard on many levels: emotionally, financially (most are not covered by insurance), logistically (traveling out-of-town to find supportive practitioners), even conceptually (who and what information do you trust?). It’s easy to think, “the doctor says drugs, what do I know”? I admire your clear-headedness to question a drug solution and experiment with non-drug treatments.
Report comment
Dr Wagner. I was told that I cannot go off the antidepressants I’ve been taking for 20 years as my brain won’t function without them. Any comment?
Report comment
Phoenixrising, I’m not a doctor, so I can’t give you individual medical advice. What I can offer is a perspective from a number of researchers on antidepressants.
1) There are many studies that show antidepressants are only a little bit better than placebo in relieving symptoms with a difference so small, that most people won’t even notice it. MIA education has a great video on that (https://goo.gl/qYBa0S). Especially given that many people have significant side effects, in general, I personally believe that attempting to get off of antidepressants is a good idea.
2) Getting off of antidepressants isn’t easy. The latest numbers I’ve seen are that 55-63% of people will have withdrawal symptoms, for some individual antidepressants, I’ve seen higher numbers. So, if you work to get off of antidepressants, understand that you may well have withdrawal symptoms and that is a common occurrence. Be prepared for that.
3) Although there is little literature on how to withdraw from psychiatric drugs, those who do it successfully, seem to do it through a very slow taper. The worst results seem to come when people cut cold turkey. Since your doctor is telling you that you can’t get off of antidepressants, I would suggest you consider getting a second opinion from a practitioner who respects the downsides of antidepressants. To find such a practitioner, consider the list of directories found in this document (https://goo.gl/MvYj8s) on non-drug approaches to depression.
4) The recovery statistics from using the Walsh-protocol nutrient therapy is fairly stunning for depression. 70% of people are able to get symptom free and off of antidepressants. Nearly all of the rest can get symptom free with a significant reduction in antidepressant dosages. You may want to consider a Walsh-trained doctor as your second opinion (Walsh-trained doctors can be found from a directory mentioned above).
5) Changing drug dosages should be done under the care of a practitioner that understands it and that you trust. Personally, in looking for a second opinion, I would ask the prospective doctor the number of patients they have helped get off of antidepressants and what their experience was. There is also information on the web, but I’ve not looked at it closely so can’t really weigh in on it.
6) Self-determination and making your own decision on your personal health is important. It can aid recovery. At the end of the day your practitioners are your guides, not your boss. This is your choice to make. I wish you well with your choice. With a handle like PhoenixRising, I’d guess that you believe in your gut that you can bring the change you need. That is a good thing.
Report comment
Have you checked out http://survivingantidepressants.org/
Report comment
Oldhead, Thanks for the link… Can you or others weigh in on what you think of these resources: 1) Rxisk Guides and techniques for psychiatric drug withdrawal. (https://rxisk.org), 2) MIND, Making Sense of Coming off Psychiatric Drugs, (http://bit.ly/yPjusy) and 3) Harm Reduction Guide to Coming Off Psychiatric Drugs (Will Hall). https://goo.gl/yuRHOO…. Thanks.
Report comment
Lists with each type of non drug practitioners and new age psychiatrists all over the world would be very helpful.
The lists should be from within a trustfull network like MIA and not online gathered …
In Romania there are only few options and very expensive and difficult to access and not professionally delivered, not to mention not accepted by families compared with prescribed drugs.
Report comment
I am glad for finding and reading this article. It is value added for entire community.
In my case, it is difficult to evaluate the riskeness of each non drug method. I say so as my main issue is I am unofficially labeled with bipolar mania. There are maybe other labels too for which some of the risk free methods are in fact caring some risks but anyhow these are probably less riskier than the drugs. One point is that methods like certain meditation methods or certain coaching methods or psihoterapy even behavioral can be trigeres and the symptomatology of so called severe disorders to come at the surface. The one more point is that another risk free option should be the temporary or even for life help in living without prescribed drugs. Even for mania and schizofrenia the choise of the option of treatment or self management should be facilitated, instead of nonvoluntar practices.
Report comment
Lidi,
To help you with non-drug options with bipolar you might want to consider this paper I wrote that offers a high level perspective (https://goo.gl/Dbf1od). I agree, a centralized trusted list of all non-drug practitioners would be very valuable. One doesn’t exist yet, but the paper includes links to a number of directories from fairly trustworthy sources.
Report comment
Thank you for link.
Report comment
Welcome, Craig! I feel you are a great addition to the MIA team, but with some reservations.
First, you failed to mention peer support (see the article in this issue of MIA) as a valid alternative, although there are studies of its effectiveness.
Second, your associations with groups supported by Big Phamra bother me. I guess I am one who belies that the creation and promotion of alternatives will overtake the mainstream. All one needs to do is follow the money.
I asked supporters of our current president how they can believe that this man of the 1% is going to help the 99% when it goes against his personal fortunes. Just ’cause he’s a nice guy does not stand, to me, as an answer.
As a former member of the drop-in Rap Center in Berkeley, back in the early 1970’s, when I was still “psychotic,” I remember the prevailing the ideology as borrowed from the “Radical Therapist:” The cause of all “mental illness” is capitalism. Can’t say I fully agree but I think the point is important.
Here is a reference to over 600 methods of complementary and alternative medicine:
https://www.amazon.com/Codex-Alternus-Complementary-Schizophrenia-Drug-Induced/dp/0692532439/ref=sr_1_1?s=books&ie=UTF8&qid=1473613072&sr=1-1&keywords=Codex+Alternus
Report comment
Don, thanks for the welcome and frankness over your reservations.
Yes, I value peer support too. The “been there” credibility is irreplaceable and can be a remarkable gateway to recovery. The risk I take in an article limited by space like this is giving a partial list in each category of care, always leaving important things out.
I can understand your perspective about my associations with NAMI and APA. Many on this site testify to being harmed by these organizations. What I can tell you is that although both organizations are heavily drug-oriented, there are people within them that are diligently working to expand the adoption of non-drug treatments. It isn’t happening at a rate anywhere near what we want, but it is moving. I think my net impact on both organizations is to push them ever so slightly toward non-drug treatments, and in my mind, that is good.
I’m glad you mention Codex Alternus, I was a contributing editor to Dion Zessin’s impressive work and I pulled some interesting therapies from the book that I include in my work.
Report comment
although both organizations are heavily drug-oriented, there are people within them that are diligently working to expand the adoption of non-drug treatments
They should cut their losses and resign in that case. NAMI is a sinister force with which there should be no cooperation whatever.
Report comment
Craig, you still think mental illness is real, and that people need to be healed of it.
Send my web address to your clients. I’ll find them a good lawyer.
http://freedomtoexpress.freeforums.org/index.php
Nomadic
Report comment
Hi again Craig. I have red the current article and also the article addressing bipolar disorder. From a usefull point of view, these articles deserve to be more structured or splitted by symptoms and specific states within diagnosis, so those in need easely access the information they need. Also, another structure could be function of the drugs and doses one try tappering. These restructurings of initial articles in fact are usefull in different periods of those with heavy diagnosis in special. It is for sure a need of passing through extreme states with minimum prescribed drugs and if there is no clear alternative procedure then all other options won t be implemented.
Report comment