A recent article, published in Healthcare, provides a framework to increase provider engagement in taking action against the overuse of low-value health care services. The authors identify conditions that are necessary for providers and patients to be able to have sense-making conversations and collaborate in order to reduce low-value care.
“Reducing the use of low-value services is not just doing less of what harms, it also creates opportunities to focus on doing more of what truly helps patients,” write the authors, led by Michael L. Parchman, director at the MacColl Center for Health Care Innovation in Seattle, WA.
Recently, many have addressed the overuse of medical interventions. Just last week a representative for the Office of the United Nations High Commissioner for Human Rights criticized the overuse of biomedical interventions for depression.
Despite increased attention on strategies that minimize the overuse of low-value health care services, de-implementation of existing practices is difficult to achieve. Therefore, the authors seek to “identify and describe essential operational actions necessary to support provider engagement grounded in social science theory, literature, and the experiences of leading healthcare organizations across the United States in their efforts to address low-value care.”
The authors assembled an 8-member multi-stakeholder advisory committee to assist in the development of an action-planning framework that can be used to engage providers in reducing the use of unnecessary services. This framework is based on a review of the literature on how to change physician behavior and strategies for de-implementation of existing behaviors. In addition, 23 healthcare professionals who led initiatives to reduce the overuse of low-value care were interviewed.
“Sustained behavior change is more likely if it is driven by providers themselves and if conditions that promote a new culture of medical practice are present,” write the authors.
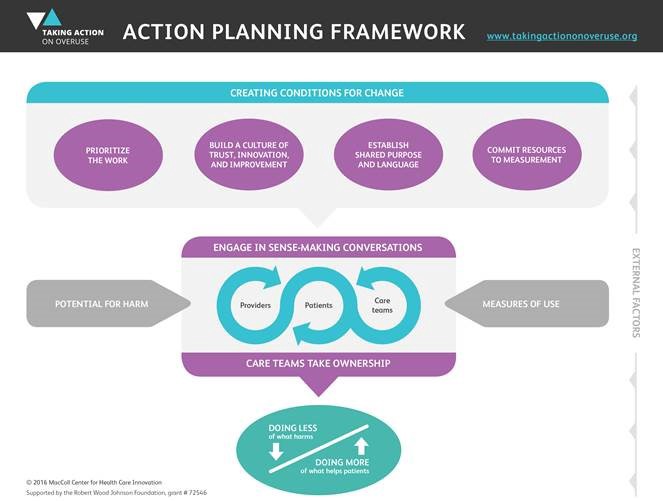
They identify four conditions they consider necessary among providers, care teams, and patients to create an environment where change can occur: “prioritize addressing low-value care; build a culture of trust, innovation, and improvement; develop shared language and purpose, and dedicate resources to data and measurement.” The authors highlight that the environment must be “non-judgmental and non-punitive” as it may be difficult for providers to confront ways they may be doing harm to their patients.
When these four conditions are in place, providers, care teams, and patients can engage in sense-making conversations, which the authors define as “exchanges through which individuals think together as a group for the purpose of making sense of non-routine problems and coordinating individual behaviors to achieve their goals.”
Conversations need to address how the overuse of low-value treatments may subject patients to harm, and these conversations must be grounded in evidence (e.g., peer-reviewed publications, data from the health care site, personal stories from patients). One interviewee highlighted, “It is not the data that changes people; it is the conversation about the data.” Lastly, providers and care teams should be encouraged to take ownership over the problem of low-value care and feel responsible for making changes.
The authors write, “engagement [in de-implementation] can be difficult when it requires changing behaviors, especially when a replacement service is not readily available.” Therefore, the authors developed “an action-planning framework for use as a roadmap to guide engagement efforts for providers, patients, and all members of the health care team in efforts to reduce low-value care.”
The framework focuses on changing the culture of a health care system to ensure both providers and patients feel empowered and comfortable to investigate where the system is engaging in treatment overuse, and develop strategies for change.
****
Parchman, M. L., Henrikson, N. B., Blasi, P. R., Buist, D. S., Penfold, R., Austin, B., & Ganos, E. H. (2016). Taking action on overuse: Creating the culture for change. Healthcare. Advance online publication. http://dx.doi.org/10.1016/j.hjdsi.2016.10.005 (Abstract)














The Atlantic published an excellent article in February on this subject.
https://www.theatlantic.com/health/archive/2017/02/when-evidence-says-no-but-doctors-say-yes/517368/
I don’t see how this will translate into fewer psychiatric interventions though when the prevailing thought is that the patients lack insight into their own ‘illness’. We’re not fully human in the eyes of healthcare providers, so how can we engage in ‘sense-making conversations’ with them?
Report comment
Low value “treatment” subjecting patients to harm-a perfect description of brain damaging electroshock used by ignorant “doctors”.
Report comment
The problem is, they are getting paid big money to provide “low-value treatment.” Stop paying doctors for committing malpractice and they’ll be more likely not to commit it!
Report comment