A randomized controlled trial conducted at the Kurdistan University of Medical Sciences compared the efficacy of vitamin B6 to propranolol for the treatment of antipsychotic-induced akathisia (AIA). The study demonstrated that there was no significant difference between vitamin B6 and propranolol in reducing akathisia symptoms, suggesting that vitamin B6 may be beneficial for improving antipsychotic-induced akathisia.
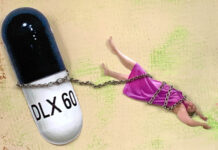
Akathisia is characterized by “restless movements and typical subjective complaints of restlessness referable to the legs, inner tension, and discomfort” and “is reported to be the most common reason cited by patients for discontinuing their medications.” First line treatment of akathisia typically consists of propranolol and can also include the modification of the antipsychotic dose.

The authors of this study highlight that the first line treatment (propranolol) is not effective in up to 70% of persons experiencing AIA and is not well tolerated in patients with bronchial asthma, diabetes mellitus, or hypotension. Second line treatments for AIA often include anticholinergics, benzodiazepines, amantadine, clonidine, and dopamine agonists. The authors of this study explored the efficacy of vitamin B6 for the treatment of acute akathisia. They draw on prior evidence has demonstrated that B6 can be effective in the treatment of movement disorders caused by psychotropic medication.
This study aimed to compare the efficacy of vitamin B6 and propranolol for antipsychotic-induced akathisia (AIA). Fifty-one individuals who had been diagnosed with antipsychotic-induced akathisia were recruited for the study; 17 patients were placed on 300 mg/12h or vitamin B6, 17 were placed on 600 mg/12 h of propranolol, and the remaining 17 participants were placed on 20mg/12 h of propranolol. The severity of akathisia symptoms was measured using the Barnes Akathisia Rating Scale. The items assess observable, restless movements, subjective awareness of restlessness, distress associated with akathisia, and global severity.
Patients included in the study were between 18-50 years of age, on antipsychotics, and had at least a mild rating of akathisia. A total of fifty-one patients were included, 17 on propranolol, 17 on vitamin B6 300 mg/12h, and 17 on 600 mg/12 h of vitamin B6. There were no significant differences on BARS scores at baseline, diagnosis (schizophrenia, schizoaffective, psychosis, bipolar disorder, or other disorder) at baseline, or adherence to medication throughout the study between the three groups. Data also showed that there was no significant difference in BARS scores between the three groups, suggesting that B6 was as effective as propranolol in mitigating symptoms of akathisia.
This is the first study which has shown support for vitamin B6 in reducing symptoms of akathisia. This is an important finding as typically the treatment of akathisia is done through other psychotropics including benzodiazepines, beta-adrenergic blockers, and anticholinergics. Moreover, this intervention has lower adverse side effects that the typical first- and second-line interventions for AIA.
****
Hassanzadeh, K., Shams-Alizadeh, N., Bakhshayesh, H., Rezaei, F., Ghaderi, E., & Shams-Alizadeh, N. (2018). Effect of Vitamin B6 versus Propranolol on Antipsychotic-Induced Akathisia: A pilot comparative double-blind study (Winter Special Issue 2018). Iranian Journal of Pharmaceutical Research. (Link)














Akathisia is an extremely serious condition involving toxic psychosis, not just a movement disorder.
Propranolol can not really treat Akathisia, but the biology says it’s possible B6 can help because it is a co-factor of glutamate decaboxylase required for the synthesis of gamma Aminobutyric acid.
http://www.worthington-biochem.com/GLDP/
The best way to deal with Akathisia is to correctly tapper off the neurotoxins, take magnesium which serves in tandem with B6 in correctly controlling the transmission of glutamate via the NMDA receptor. Also to avoid food stuffs that inhibit glutamate decaboxylase. The other very important thing that is necessary, is avoiding all the common food stuffs and herbs/spices that inhibit the metabolising enzymes: Cytochrome P450, some of them can be found here:
https://www.ebmconsult.com/content/pages/medications-herbs-cytochrome-p450-cyp-enzyme-inhibitors
Alpinia galanga – ginga inhibits CYP 2D6
Cinnamomum burmannii – cinnamon inhibits CYP 2D6
Piper nigrum – black pepper – inhibits CYP 2D6
Allium sativum – garlic – inhibits CYP 3A4
Naringenin compounds – found in grapfruit inhibits CYP 3A4
Others here:
http://www.todaysdietitian.com/newarchives/121610p26.shtml
Do a search for more.
Also, idealistically, a person should have a Cytochrome P450 test. People in the US should all look into this, see if it is covered by your insurance. This is the type of thing, should point out I have nothing to do with that company, just posting it, so as to describe the relevance:
https://www.youtube.com/watch?v=JnNI6JEFf38
Report comment
Should say that B6 (active form PLP) is more likely to be effective with benzodiazepine withdrawal akathisia, because people are toxic on glutamate. A truly despicable crime, because it can and usually does last a long long time. Implement the above and use liquid titration to slowly come off the benzo. Been and did done it, live to tell you.
Report comment
Hey, I have a low chance of getting responses here for my own issues with psychiatry but I need some more info on this and you seem to know more so I’m cross-posting my reddit submission here:
https://www.reddit.com/r/Badpill/comments/9g6bsk/hey_i_need_some_quick_rundown_on_akathisia/
No need to click on the link, I don’t need upvotes I need information. This is the content:
So I have my own issues which is why I’m not doing a longer run around with looking for actual professionals regarding this issue but I need some fast background (non-cliff notes preferably) with how this can mess up the spine and the neck to possibly help a guy.
Reddit isn’t showing up lots of replies and I only found this because I did a search on it and saw this link and this sub:
https://www.reddit.com/r/Badpill/comments/6omi20/this_will_be_an_exhausting_but_important/
Can’t go into any more details because the person hasn’t given me much to work with yet but here’s some context of why I need this info fast:
https://www.reddit.com/r/Portland/comments/9f8qed/could_be_urgent_some_guy_from_facebook_is_asking/
Report comment
Thank you.
Report comment
The psychiatrist who weaned me off the antipsychotics, after he stopped listening to a child abuse covering up psychologist – who did not know me – and stopped seeing me, thus finally stopped defaming me to the psychiatrist.
He did recommend both Vitamin B6 and Magnesium, as he weaned me from his akathisia inducing drugs.
Report comment
I had never heard of the Barnes Scale. It seems to focus on an inability to keep still? I suffered akithisia so frequently as a young person without my doctors understanding, that I trained myself to override it and hold very still. Because if I didn’t, I’d get even more medications. I would physically feel like I was in a maelstrom though.
Report comment
Thanks for letting people know about your childhood experience. There is something called mild akathisia that is sometimes experienced as remaining motionless. (Not saying yours was mild, by the way.) I had some kind of hellish neurotoxicity that meant the most miserable two years imaginable, or worse, and towards the end spent a great deal of time sitting motionless. My mind would be running at full tilt but I couldn’t conjure up a will to move. Heartbeat and breathing, probably some blinking, were the extent of my physical activity, and only because they have wills of their own.
Report comment
Did you finally get better, BL? Sounds like paralysis–only worse.
Report comment
I’m surprised they didn’t try, for example, doses of propranolol that are usually used in clinic–40-80 mg/day. That would have made the results more relevant and believable. As of now they seem far-fetched and not very useful, scientifically speaking. What a waste.
Report comment
From both personal and professional experience as a licensed clinician suffering from an iatrogenic injury caused by Vitamin B6 neurotoxicity, I would highly advise being extremely cautious in supplementing with anything in excess. In the case of vitamin B6 toxicity, there has been a case study showing someone taking even just 1.4 mg daily led to neuropathy. There has also been a published study demonstrating cerebral damage in rates from vitamin B6 neurotoxicity.
If you browse through the FB peer support group, Understanding B6 Toxicity Using Western Research, you will see that in addition to the known and established small fiber polyneuropathy damage caused by vitamin B6 neurotoxicity (and subsequent withdrawal), among many members there are also reported symptoms very similar to benzo withdrawal including: akathisia/chemical terror, depersonalization/derealization, intrusive thoughts, sensitivity to stimuli, agoraphobia, anhedonia/chemical depression, and many more. It is a horrifying, torturous, and prolonged journey to recovery for many people lasting months to years and beyond.
As vitamin B6 is a co-factor in the synthesis of GABA, serotonin, dopamine, and norepinephrine, similarly just as withdrawal of benzodiazepines leads to glutamate excitotoxicity, it might be that withdrawal of vitamin B6 also leads to a cascade of disruptions and imbalances in neurotransmitter systems that can take years to heal from. This is even less well known, understood, and accepted both in the medical community and mainstream culture.
Given the overlap in B6 and benzo toxicity and withdrawal symptoms as well as the waves and windows as part of the nature of recovery, the term benzodiazepine-induced neurological dysfunction feels very apt and applicable.
All that said, if you are supplementing with vitamin B6, please do so with extreme caution including having regular serum B6 tests done and closely monitoring yourself should you develop any symptoms. For some, those symptoms might be the classic sensory and neuropathic ones like tingling or burning sensations. However, for others, they might be neuropsychiatric symptoms like anxiety, hypervigilance, insomnia, depersonalization/derealization, or brain fog as the first presenting symptoms.
Report comment