Recent claims about antidepressant effectiveness have been based on misleading statements and misunderstandings of science, according to a new article in Acta Neuropsychiatrica. The article was written by Michael P. Hengartner at the Zurich University of Applied Sciences, Switzerland.
Hengartner is responding directly to a commentary by Goodwin and Nutt, who recently wrote that despite numerous meta-analyses demonstrating a poor risk-benefit ratio for antidepressants, there is no need to question their usage. Although Goodwin and Nutt admit that antidepressants usually show only less than two points improvement (compared with placebo) on the Hamilton Depression Rating Scale, which is considered a clinically undetectable difference, any change at all should be viewed as a sign of future improvement (although they do not provide any data making this link).
Hengartner finds several misleading statements and misinterpretations of fact in Goodwin and Nutt’s commentary. For instance, Hengartner demonstrates that Goodwin and Nutt cherry-picked the data they used to make their claim about the Number Needed to Treat (NNT). This number is a measure of how many people need to receive antidepressants before one person improves.
When Goodwin and Nutt report that the NNT is between five and seven, they “selectively report efficacy from an arbitrary subgroup of ‘true benefiters’ delineated post-hoc in five escitalopram trials, and they ignore that the mean drug-placebo difference across all participants in SSRI trials is about two points, not three points. Thus, the NNT is not between five and seven, but rather between eight and 10.”
To justify the use of this cherry-picked group, Goodwin and Nutt argue that the data is bimodal (true benefiters vs. non-benefiters)—but conduct no statistical test to validate this claim. Hengartner argues that there is no evidence to interpret the data in this way; in some of the graphs, the data is “obviously not bimodal.”
Another misleading statement is Goodwin and Nutt’s use of the statistic of a “16% greater response rate” for antidepressants versus placebo (a statistic which Goodwin and Nutt selectively reported from an earlier study). Hengartner shows how, because of arbitrary cutoffs in what are considered “response rates,” this statistic could be used to hide what is actually the same mean difference. A change of 50% is often considered the cutoff for “response” to the drug (or placebo), but that means that people who improved only 49% on the depression scale are considered “non-responders.”
Hengartner makes the following example of a situation where a change of 10 points on the depression scale is considered “response” but a difference of 9 points is considered “non-response”:
“In the antidepressant group, 56 people improved by exactly 10 points, 24 had 9 points, and the remaining 20 had 8 points. In the placebo group, 40 people improved by 10 points and the remaining 60 had 9 points. So what’s the result? Response rate would be 56% for antidepressants and 40% for placebo, but mean change score would be 9.4 for both antidepressants and placebo. That is, mean improvement would not differ between drug and placebo arm!”
Hengartner also takes issue with Goodwin and Nutt’s misappropriation of abrupt discontinuation studies as indicators of the long-term protective effects of antidepressants. Hengartner writes, “These trials cannot provide information about the long-term efficacy of antidepressants, as they merely indicate that stopping antidepressants abruptly in patients who improved on them can cause considerable health problems that may qualify as depression relapse.”
These symptoms are most likely due to the withdrawal effects of the drug itself. So, according to Hengartner, it’s not that these drugs are protecting against depression returning, but rather that withdrawal from these drugs causes physical and mood symptoms, as with other drug withdrawal, that diminish when the person goes back on the drug. Hengartner concludes:
“Researchers should avoid inflating the apparent benefits of these drugs, and instead acknowledge that they may also cause various adverse events, including rare but serious ones.”
Meta-analyses have found that, when unpublished trials are included, only about half of the clinical trials show antidepressants beating placebo, and the risks of antidepressants outweigh questionable benefits. Data about the risk of harm “have been suppressed,” according to an article in Scientific American. Authors of a recent study wrote:
“SSRIs might have statistically significant effects on depressive symptoms, but all trials were at high risk of bias and the clinical significance seems questionable. SSRIs significantly increase the risk of both serious and non-serious adverse events. The potential small beneficial effects seem to be outweighed by harmful effects.”
****
Hengartner, M. P., (2019). Scientific debate instead of beef; Challenging misleading arguments about the efficacy of antidepressants. Acta Neuropsychiatrica. https://doi.org/10.1017/neu.2019.23 (Link)














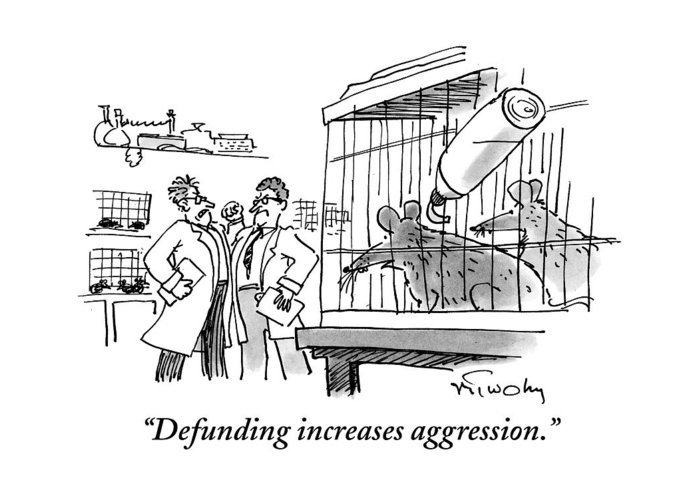
I like the cartoon. Szasz said there is a time to laugh at the powerful,“When a person can no longer laugh at himself, it is time for others to laugh at him..” and John Lennon also advocated for nonviolence, as once they have you (visibly) angry , they know how to handle you.
Report comment
One major problem… there is no such thing as an “antidepressant.”
Report comment
Hamilton Depression Rating Scale?
https://abuse.wikia.org/wiki/Hamilton_Rating_Scale_for_Depression
Under no circumstances should anyone ever be subjected to such a questionnaire, or anyone cooperate with such a questionnaire, or any paper be published based on the results of such questionnaires.
Report comment