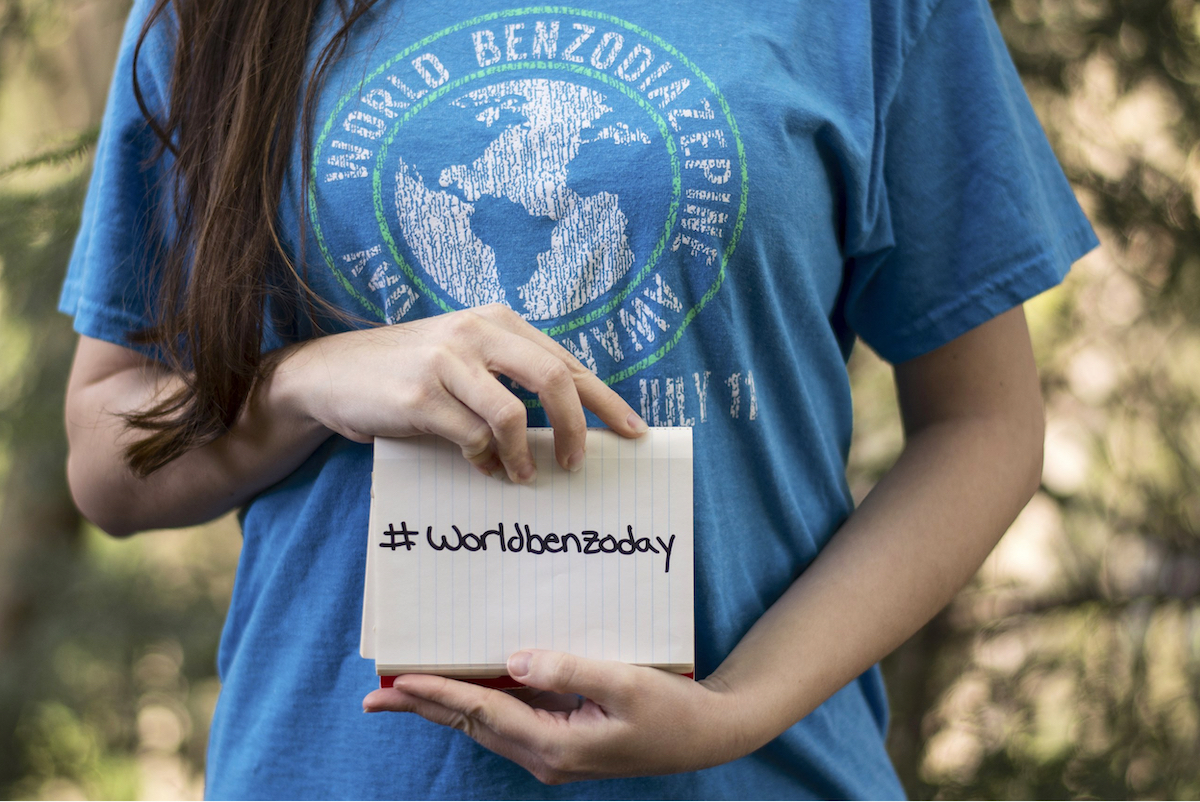
This week on MIA Radio, we present the second part of our podcast to join in the events for World Benzodiazepine Awareness Day 2020 (W-BAD). In part one, we interviewed Angela Peacock and talked about her experiences of taking and coming off benzodiazepines and also her involvement in the film Medicating Normal, which has a special screening and panel discussion on July the 11th at 1:00 PM EST.
And before we go on, I just wanted to say that these podcasts would not be possible without the efforts of W-BAD lead operations volunteer Nicole Lamberson, who goes above and beyond to make these interviews possible. Later in this episode, we will hear from Baylissa Frederick, who is a therapeutic coach and psychotherapist with over two decades’ experience working with clients affected by prescribed drug injury. But before we chat with Baylissa, I’m delighted to get the chance to talk with clinical pharmacologist Dr. Jim Wright.
 Jim is Emeritus Professor in the Departments of Anesthesiology, Pharmacology, and Therapeutics in Medicine at the University of British Columbia. Jim obtained his MD from the University of Alberta in 1968, and his PhD in pharmacology from McGill University in 1976. He is a practicing specialist in internal medicine and clinical pharmacology. He is also Editor in Chief of the Therapeutics Letter and he sits on the editorial boards of PLoS One and the Cochrane Library. Dr. Wright’s research focuses on issues relating to the appropriate use of prescription drugs, clinical pharmacology, clinical trials, systematic review, meta-analysis, and knowledge translation.
Jim is Emeritus Professor in the Departments of Anesthesiology, Pharmacology, and Therapeutics in Medicine at the University of British Columbia. Jim obtained his MD from the University of Alberta in 1968, and his PhD in pharmacology from McGill University in 1976. He is a practicing specialist in internal medicine and clinical pharmacology. He is also Editor in Chief of the Therapeutics Letter and he sits on the editorial boards of PLoS One and the Cochrane Library. Dr. Wright’s research focuses on issues relating to the appropriate use of prescription drugs, clinical pharmacology, clinical trials, systematic review, meta-analysis, and knowledge translation.
Listen to the interviews here. The transcripts below have been edited for length and clarity.
Part 1 – Jim Wright
Part 2 – Baylissa Frederick
James Moore: Jim, welcome. Thank you so much for taking the time to chat with me today for the Mad in America podcast. I’d like to ask a little bit about you and your background and what it was that led you to a career as a clinical pharmacologist?
Jim Wright: I got interested in drugs in medical school and I came to realize that a lot of the problems that patients had you could solve by looking at the drugs they’re on and what might be causing some of the problems. So often I found that I could solve people’s problems by stopping their drugs, not by starting new drugs.
When I went to Montreal and was doing my internship in internal medicine, I decided to get involved in a PhD in Pharmacology at McGill. So I was able to expand my understanding of pharmacology and keep my clinical skills going at the same time. There was a strong clinical pharmacology program at McGill at the time. So I’ve been interested in doing clinical pharmacology for the whole of my career.
I think people don’t appreciate that most doctors don’t have a very strong understanding of pharmacology and even pharmacists don’t. Pharmacists are very good at classifying drugs and knowing all the drugs, but they don’t really understand the complexities of the effects of drugs in people. It’s a very complex field.
The more you know about a drug, the less likely you would be willing to take it and particularly not on a daily basis. That’s really where people get into trouble. It’s really just accepting and trusting and taking things. It’s amazing how people would research when they buy a TV or a car and look into it in-depth, but they’ll be willing to start taking a drug without learning much about it at all. I think that’s the big problem in medicine today is that the drugs that people are taking on a daily basis are having a permanent or at least a serious effect on their brain.
Moore: You used that phrase in some communication we had when setting up this meeting and I was intrigued because I haven’t heard many pharmacologists be willing to say publicly that the more they know about a drug, the less they’d be willing to take it themselves. I wondered if that was based upon your knowledge of the effects of the drugs on the body itself, or whether it’s from knowledge of people’s different experiences with some types of drugs or maybe a combination of both?
Wright: It’s really a combination. There’s no drug that has a significant effect in a person that doesn’t have potential harms. So we always need to be weighing the potential benefits versus the potential harms. When you start to appreciate the potential harms, they’re significant and often serious, but you can find that out by just reading the drug monograph and looking at the adverse effects. If people did that, I think there would be less people willing to just take drugs. You can cause a lot of damage by taking the drug on a daily basis, particularly.
Moore: I’ve experienced myself prescribers saying, “Don’t worry too much about all the listed side effects because they’re very rare and only a very small number of people get them,” but reading that list of adverse effects is quite important for informed consent, isn’t it?
Wright: Yes, it is, and they often are rare, but they can be life-threatening, so it’s not something you want to do lightly.
Moore: You are a member of the Therapeutics Initiative, so I wondered if you could tell us a little bit about that organization, what it does and how you got involved?
Wright: In the latter part of my career, I was convinced to become the Managing Director of the Therapeutics Initiative; this was in 1994. And that led me into a field of research, which is called a systematic review and I’m looking at the benefits and harms of drugs. And so I’ve been doing that and was either Managing or Co-Managing Director for 25 years. In addition to that role, I was the Editor in Chief of the Therapeutics Letter, which is published by the Therapeutics Initiative and is freely available on the website. Those letters come out every couple of months and they’re usually kept quite short and they’re primarily for prescribing doctors, but there’s a lot of good information for anybody who wants to read them.
In the Therapeutics Initiative, we have a rule that you can’t have any conflicts of interest. It’s been that way since the very beginning. So it’s people who are looking at the research, they’re completely independent and not conflicted and nothing to gain from the drugs or from any of the recommendations that are made.
In October of last year, after 25 years, I decided it was time for me to step down. I’m still involved with the group and still on the steering group, but I’m not Co-Managing Director anymore. That’s given me a bit of a break and I’m also not the Editor in Chief of the letter, which is also quite a big job and Tom Perry now is the Editor in Chief of the letter. In January of this year, I retired from the university and so I’m now Professor Emeritus, but I’ve stayed on as the Coordinating Editor of the Cochrane Hypertension Group. So I’m still doing systematic review research and I still see some patients on one day a week in the clinic.
Moore: I wanted to ask a little bit about the Therapeutics Letter, which I found really interesting. Obviously as a consumer or as a patient, when you do read the official information on the drugs, perhaps the package insert or information that your doctor has given you, you are never really sure of the provenance of it. It very rarely includes any information at all from people that have taken that drug; it tends to be from the manufacturer’s view of things.
The Therapeutics Letter I found interesting because not only does it present manufacturer-like information about drugs, but it also includes anecdotal accounts. I’ve not seen it before because certainly in the UK, and I guess in the US and Canada too, doctors sometimes tend to frown on anecdotal accounts of using drugs. To me, I think those accounts are a fairly fundamental and important part of a rounded understanding of what the effect of a particular drug or intervention might have. So I was really interested to see that you use anecdotal information in your Therapeutics Letter.
Wright: Not to a large degree, but when we were talking about withdrawal from antidepressants, there isn’t much evidence and there aren’t clinical trials in that area. So in that area, the best evidence is actually anecdotal evidence. When we get into adverse effects, you often can’t find very much good information in terms of the randomized trials. So then you have to go beyond that and look at observational studies and experience.
In general, what we’ve learned in the Therapeutics Initiative over the 25 years that I was there is that when you look into the evidence that is used by regulators to put drugs on the market and you get into the detail, we continue to be quite shocked by how weak the evidence is that the benefits outweigh the harms. Often it’s a small statistically significant difference between a drug and placebo, but not clinically very important.
So I’m often surprised that a particular drug is on the market and that we’re giving it to people based on such weak evidence. That’s the biggest thing that we learned. Then we also learned that the harms associated with drugs are often much more than we used to think because when we go into something, we have a sort of idea about it at the beginning. By the end of it, we appreciate that the harms are much greater than most people think.
Moore: I wondered why you thought it was that we don’t have this rigorous scientific understanding of adverse effects and the propensity for the drugs to actually affect people in a negative way? Is that because of the way that clinical trials are done on these drugs, or is it because we’re not really capturing adverse effect data in quite the way we should?
Wright: That’s mostly because there are very few long-term trials. So almost all the drugs get on the market with fairly short-term trials. So really there’s only evidence over short- term use. What happens in practice is people start to use them long-term and daily and there really isn’t any evidence in terms of the benefits and harms for long-term use. There’s no incentive for drug companies to do long-term trials, so we really need governments to be pushing for that and funding long-term trials so we can actually know what the benefits and harms are.
Moore: I guess long-term trials are technically difficult and probably very costly because it’s difficult to follow somebody for decades of treatment?
Wright: Yes, but I’ve also argued that they are not that expensive if you do it, because we do track in administrative databases, we track hospitalizations and deaths. So you can do actually large long-term trials without having a huge budget and it doesn’t cost very much to randomize people. So that’s the key thing is actually to set it up so that you actually randomize people in order to be able to come to some answers.
Moore: Since this interview is being shared on World Benzodiazepine Awareness Day, we’ll focus in on benzodiazepines now a little bit. I know you have an interest in benzodiazepines, so I wondered what it was that piqued your interest in that class of drugs?
Wright: We did a Therapeutics Letter on benzodiazepines fairly early on, probably back in 1996. At that time, we had got an idea of how many people were taking them in British Columbia. It was quite surprising how many people were taking them on a long-term basis. Then as you get into it, you realize that the evidence for the drugs is fairly weak and that most people were taking it for insomnia.
The trials done in those people were fairly short and it seemed to help maybe a little bit in the short-term, but even by a week or two weeks, they’re probably not sleeping any better than the placebo group but they got on the market based on that. The monographs as a result of that say that they should only be used short-term. The problem with benzodiazepines is that isn’t happening and once you start to take it long-term, then you become tolerant. The drug is really not helping anymore. Over the long-term, we’re learning more and more about the toxicity associated with long-term use.
Moore: So what would you consider, then, appropriate use of benzodiazepines? I know there’s been some guidance that they should only be prescribed short-term, but I wondered in what situations you felt it was appropriate and then perhaps not appropriate to prescribe benzodiazepines?
Wright: The only way I prescribe them now is as rescue therapy, I think that’s the best term. So I explain to patients that if you take them regularly, they won’t work but if you take them as rescue therapy, they continue to be effective and can be useful for some people. So if a person is taking one for sleep say three or four times a month, they can find it useful. They need to know when that would be appropriate and so some people are able to use it in that way and don’t get into any trouble.
Moore: You mentioned that you’d identified withdrawal issues from antidepressants and benzodiazepines as a particular area of concern and one where there isn’t much scientific rigor. I believe that you’ve written about using methods of liquid titration to withdraw from benzodiazepines very slowly. So I wondered if you could explain a little bit about using that method to come off them and has it been more successful or less successful than other methods of stopping benzodiazepines, in your opinion?
Wright: I should just mention that in the last 10 or 15 years, partly through meeting Heather Ashton and learning about some of the problems and the class-action suit in the UK against benzodiazepine companies, that I have gotten more and more interested in helping people come off of benzodiazepines.
I’ve always used the Heather Ashton manual and I’ve been referring a growing number of patients with this problem to help them to come off. What I’ve learned is that it’s extremely difficult. Every patient that I’ve ever helped come off of benzodiazepines has described it as the worst thing that has ever happened to them in their life.
The principle is to do it slowly, 10% every two weeks, and one of the other principles that Heather Ashton promotes is that you should tailor it to the patient. So when I’m helping people we work out what works best for them. Some people need to do it extremely slowly. It was actually patients who have introduced me to the liquid titration method and they are the ones who’ve found it on the internet and have worked it out.
The approach is that you put a standard amount into a standard amount of liquid and you create a suspension. Then you can then pour off a certain amount and an increasing amount. So you can lower it at whatever rate you want over a period of time. People have to be careful and they have to be willing to do it very carefully in order for it to work. For some people that works and some people that doesn’t, so it’s not something for everybody.
Moore: Have you noticed a difference between people who may have tried to stop more abruptly and people that have used a gradual withdrawal method? Is titration a better option for people?
Wright: Titration is definitely better in terms of the success rate. If you do it slowly, you’re much more likely to be successful. The people who do it more quickly or abruptly very likely end up back on the drug. So they really haven’t accomplished anything. If somebody is off and they’re doing all right, obviously you want to support that and even independent of whether they did it slowly or not.
We don’t really have good evidence that any particular rate of decrease leads to less protracted symptoms after you get off. That’s something that somebody needs to be researching. We need to study this whole phenomenon of long-term adverse consequences of coming off these drugs.
Moore: Prescribers including general practitioners or family doctors often really do not seem to know very much at all about the need to gradually withdraw people from dependence-forming drugs, particularly benzodiazepines, but also antidepressants too. Many people I’ve spoken with have had poor advice to stop quickly, then they go back to their doctor in distress, and the doctor says it’s relapse. The drugs being at fault is the last thing they think of.
So how can we best approach the medical establishment to reinforce that certain classes of psychoactive drugs need to be tapered gradually and probably for the majority of people that take them? I think the default at the moment is advice to cut the drug by half or a quarter over a few weeks and that causes some people dreadful problems.
Wright: I agree. The need to taper benzodiazepines is now being more accepted. The College of Physicians in British Columbia actually provide the Heather Ashton manual on their website. There is a growing understanding of the problem with benzodiazepines. The Therapeutics Initiative could look at prescribing over time and we could see if there is some decrease in prescribing but it probably isn’t widespread, but there is some more appreciation that these are not good drugs to be taken long-term.
Moore: Are there practical difficulties for people in titrating off benzodiazepines? Is formulated liquid available for the more common variants and not for the others?
Wright: I am not familiar with convenient liquid benzodiazepine formulations. If you’re going to do the liquid titration, you have to do it yourself. There are a few compounding pharmacists that will prepare drugs in precise amounts in capsules, so sometimes people do it through a compounding pharmacist. The principle for benzodiazepines is to transfer to diazepam if it’s possible because it’s longer acting and there are smaller tablets available so it’s more convenient in terms of gradually reducing the dose. The main thing is for the person to become knowledgeable and find out what works best for them. There are some people who are very good at measuring on a jeweler’s scale and measuring small amounts and doing it that way. So there are a number of different ways that it can be done.
Moore: When I first became aware of this world, I was quite staggered to find out actually how much people had to self-support and do this for themselves because their prescribers were not aware of the need to taper gradually. They weren’t aware of any methods to do it. In some cases, they weren’t particularly supportive of the person trying to do it. I think that’s quite an indictment that prescribers are so in the dark about this.
Wright: People do need support, they need people to help them along the way. The people who are successful are more successful if they have family support, a spouse, or somebody who is helping them. It is an extremely difficult thing and that’s one of the main messages. You’re right, a lot of physicians still aren’t knowledgeable about that.
Moore: In an article in the Chronicle Journal, you talk about how the brain has changed as a result of the drug in patients who have taken benzodiazepines regularly. You also talk about withdrawal effects, meaning that your brain is trying to heal and readapt. So can these issues of physical dependence, tolerance, and withdrawal be thought of as brain or central nervous system injury, especially in patients who go on to be protracted sufferers?
Wright: I’m convinced that that’s the case but we don’t have any measure of it. Maybe someday there will be a measure of it, then it would be possible to see why some people are having more trouble than others. But I’m convinced that all these drugs when you take it on a regular basis, so not if you take it intermittently, but if you take it on a regular basis, the brain does adapt to try and counteract the effect and so that it is standard that tolerance does occur to all drugs that have an effect on the brain. It includes alcohol and any drug that is taken on a chronic basis leads to tolerance. That tolerance is a change in the brain and so when that drug is not there anymore, then the brain… that change is still there, and so it leads to symptoms.
So I’m convinced that that’s the case and it’s a big problem for all psychoactive drugs. We know that it occurs and we also know that it probably can be relatively permanent because we know that with antipsychotic drugs, people quite frequently develop tardive dyskinesia. That’s a neurological phenomenon where they have involuntary movements of their tongue or other parts of their body. We know that can be relatively permanent.
So anybody who says that drugs can’t cause permanent effects on the brain are discounting that observation that is well-known and has been known for 20 years or so. So likely these other things that people experience are almost certainly due to changes in the brain as well.
Moore: Is there any merit in pharmacological intervention for someone struggling with post-withdrawal effects or does that just risk creating further complications?
Wright: I am frequently asked that and when I’m helping people to come off, they frequently say “Well, can I take something that will make this easier?” My answer is always no, and definitely don’t take anything that’s acting on the brain because that’s just going to complicate things more and there’s no supplements or anything. Maybe someday there will be something that might help, but for the most part, anything is going to just complicate things.
So you want to use exercise and getting the brain involved in mental activities to distract and healthy diet and good sleep patterns. You have to do all of those things and then psychotherapy is helpful, but you have to be with a psychotherapist who is not going to prescribe drugs. Most psychiatrists aren’t willing to only provide therapy.
Moore: There is a Vancouver benzodiazepine support group that lists you on their website as the only qualified doctor available in the Vancouver area who understands the implications of taking benzodiazepines and who understands and supports a benzo withdrawal program. Why do you think it is that so many benzodiazepine-affected patients have such a hard time finding knowledgeable providers such as yourself, especially after the problems with this particular class of drugs have been in the literature in some form since the 1960s?
Wright: I am frequently asked if I can find somebody but there are very few clinical pharmacologists in the world is one of the issues, and most clinical pharmacologists aren’t interested in this particular area. I don’t think there’s a lot of money to be made in helping people get off of drugs. So that is an issue. I’ve certainly exposed a lot of students to the problem and so I’m hoping that some of those will continue on and with an interest in this area. I guess that’s the main reason. It’s a difficult area to help people, but it’s certainly needed.
Moore: At the University of British Columbia faculty and staff page, one of your research interests is listed as educational strategies to improve drug prescribing behavior. In your opinion, can prescribing behavior be improved where benzodiazepines are concerned?
Wright: Yes, definitely, that’s the solution. So all doctors now should be warning patients and only prescribing for a short-term use or for a rescue therapy, and they should just refuse to prescribe long-term. There are more and more doctors doing that. In British Columbia, the College is working to try and encourage doctors to not prescribe long-term. So there is some movement in that regard.
Moore: In a 2007 article about the Therapeutics Initiative, you said: “Consumers should always ask physicians for evidence that drug treatments are effective, and that nobody should take anything unless they’ve been adequately convinced that the benefits outweigh the harms.” This seems like an information minefield, so how can consumers go about trying to get hold of the information that will allow them to make the best choice for their long-term health and wellbeing?
Wright: The sad thing is that if you asked most prescribers what the evidence is that this has a benefit and even more important, if you ask them what’s the benefit over the long- term, they wouldn’t know that there haven’t been any long-term trials for virtually any of these drugs: antidepressants, antipsychotics, benzodiazepines. So the answer is, no, we don’t know whether the benefits outweigh the harms. I’m growingly convinced that for many of these drugs, that the harms significantly outweigh the benefits.
Moore: Thank you, Jim, it’s so heartening to get to talk with someone who acknowledges the risks and takes such a careful and cautious route to prescribing and also someone willing to help and support those who have suffered iatrogenic harm even though they followed their prescriber’s instructions to the letter.
Wright: I’d like to just mention that I think Robert Whitaker is doing a great service to society through his book and his attempts to enlighten people about the whole problem. We need to encourage people like him as well. Anatomy of an Epidemic is a book I recommend to all my patients to read and I do think it is really an important epidemic that we need to be aware of and one that is almost certainly being caused by drugs. Not helped by drugs, but actually caused by drugs.
***
Now for our second interview for this World Benzodiazepine Awareness Day podcast and I’m so pleased to get the chance to chat with Baylissa Frederick.
 Baylissa is a psychotherapist, coach and author with two decades of experience working with people from all over the world. She holds a Master’s degree in therapeutic counseling and is involved in helping people affected by prescribed antidepressant, tranquilizer and opiate physical dependence and withdrawal.
Baylissa is a psychotherapist, coach and author with two decades of experience working with people from all over the world. She holds a Master’s degree in therapeutic counseling and is involved in helping people affected by prescribed antidepressant, tranquilizer and opiate physical dependence and withdrawal.
Baylissa is the author of the internationally successful self-help book Recovery and Renewal, the memoir With Hope in my Heart and two journals: Dearest Me and Dearest Friend. Baylissa was prescribed the benzodiazepine clonazepam, also known as Klonopin, for a form of dystonia, an involuntary movement disorder and she survived an intense withdrawal experience when coming off. She is now fully recovered and dedicates her time to helping and supporting others.
James Moore: Baylissa, welcome, thank you so much for joining me for the Mad in America podcast. To begin, I wanted to ask about your experiences of taking and withdrawing from clonazepam (Klonopin) and also then if those experiences led to the work that you do now in supporting those who are struggling with prescribed drug injury?
Baylissa Frederick: Thank you, James, thanks for having me. It is a privilege and an honor to be here.
Just to tell you a little bit about my experience, I have a condition known as dystonia. I’ve had it since I was age three and I was prescribed clonazepam back in early 1998 for it. My GP said, “it’s a child’s dosage”. I didn’t know that clonazepam was actually a benzodiazepine, it was under the brand name Rivotril which wasn’t familiar to me and we didn’t have the information we have now.
So I was excited and I took it and it did help with the spasms initially after about maybe three weeks. I think by then I had started developing tolerance because the spasms came back but more violently, more intensely. So I threw the medication away, I threw it in the bin and three days after I had what seemed like a grand mal seizure and I remember rummaging through the bin taking it out, thinking, oh my gosh, I’ve developed epilepsy.
When I went to my doctor, he just said: “oh no, you need to take this for the rest of your life” and so I took it for almost eight years. I eventually started losing my memory, being very spaced out and I had depersonalization and derealization and things started going wrong. I ended up in and out of the GP surgery, sometimes in and out of casualty with very weird, strange, complaints.
One day in Cardiff, Wales, I couldn’t find my way home and I kept driving around in circles, wondering where I lived. When I eventually got through the front door, I went straight to my computer and for the first time I typed in clonazepam rather than Rivotril and all these websites came up saying, ‘buy cheap Klonopin’ and I remember I just went cold.
I thought, oh my gosh, I’m on an addictive drug. That was the same day I found the Ashton manual and I cried with relief because that told me exactly what was happening. The following day, I took the manual that I had printed out and I took it to my GP and said look, I found what’s wrong, it’s called benzodiazepine withdrawal.
So he prescribed the Valium (diazepam) needed for me to taper off. I had two failed attempts because I developed very bad seizure-type movements and reinstated in order to go to work. In the end for the third attempt I gave up work and I did it to the end and I had a very intense withdrawal but I recovered.
Out of that came a book called Benzo-Wise because when I was going through it, I just didn’t find enough resources. So I decided to write a book that would help people with coping, that book is Recovery and Renewal. From the book, my practice as a therapist, supporting people in withdrawal evolved. It happened by default in that it was not my plan to take this course, but I have no regrets whatsoever and I’m happy to be recovered and to be able to encourage people.
Moore: Eight years on clonazepam, that’s quite a long time. Can I ask you how long it was that you took to taper off?
Frederick: Not long, I know now it was maybe too rushed. I think I took two and a half years for all three attempts and maybe a year and five months for the final, successful attempt. I completed it on December 17, 2005.
Moore: The question that people always want to ask anybody that is involved in the withdrawal world is when will I feel better, how long will healing take? That’s such an important, but such a difficult question, isn’t it? I’m guessing that you went through a period of healing after finishing your taper. So was it a linear thing and how was the healing for you?
Frederick: It was, but that’s because I went into acute during my taper, rather than at the end of the taper. I was in and out of hospital and I was very symptomatic throughout the taper and after. After the last dose, I was housebound and bedbound for parts of the time and on my own. I didn’t have the support of my doctor. He actually prescribed all the diazepam needed in one go. It was different back then as well. I had a razor blade that I used to use to snip the tablet in half and then quarter and it was just a nightmare compared to the sophisticated way people that taper now.
I just found ways of coping, ways of getting through each day. I did have waves and windows but the windows or the periods where the symptoms abated, it wasn’t that they all went away. It just meant that maybe the brain fog lifted a bit and I felt, oh my gosh, maybe I am going to get better. So I really relished those times.
Moore: Thank you for sharing that. When was it that you started to kind of support others struggling with similar things and did that start off informally?
Frederick: I vividly remember in March of 2006, I was still in the throes of withdrawal but I remember I was listening to Dr. Wayne Dyer on the radio. I think somebody with cancer called in and he said to her, “how best can I serve?” That just struck a chord with me and I thought, I know what I’m going to do. I’m going to get a blog online and just share with people. So I started this blog, at first I called it Benzo Blunder, then I changed the name to Lights in My Windows. James, it was the most airy-fairy blog you could ever imagine. Anyway, it soon became more serious than that and I would just sort of write, encouraging everyone to not give up.
What struck me as quite surprising and unusual was the response. In no time there were thousands of people writing back and they were going through the same thing. We didn’t know that there was this underworld of suffering. That evolved into the journals and the Benzo-Wise book and all that time I was emailing with people who were in withdrawal. After I healed, I never charged or had a practice formally, but I would until from early morning until about 11 at night, I would be speaking to people in withdrawal telling them, don’t give up, keep holding on and that went on until about 2010.
Then I started Recovery Road which was meant to be a charity, so I registered it with the charities commission and continued the work. I ran a helpline then Lady Caroline Montague got in touch with me and said she wanted to help. So she tried to get funding but we weren’t able to sustain it because we couldn’t get proper funding. In the end, I dissolved it and that was when I just had to start working as a therapist again. So in 2014, that was when I started back as a counselor, not just supporting people in withdrawal at the time I was working with Cardiff Met university also.
Moore: So aside from benzodiazepines, do you also work with patients who are having trouble with other psychotropic medications? If so, do you see similarities between the problems that people are having with benzodiazepines and those they might be having with maybe antidepressants or antipsychotics?
Frederick: Yes, I do. I have people who contact me because of difficulties experienced when coming off the antidepressants, anti-psychotics, opioids, stimulants even. I’ve also had people affected by over the counter herbs such as valerian and St John’s Wort. The most surprising for me has been the number of people in withdrawal from magnesium and these are people who didn’t take a benzodiazepine or an antidepressant. I would say that in all the cases, the symptoms are very similar and the withdrawal experience maybe for antidepressants, benzodiazepines and antipsychotics that the withdrawal can last longer.
Moore: For anyone going through withdrawal and experiencing this, they can be extremely anxious, they can feel depressed, hopeless, completely inconsolable at times when they are suffering and in great need of support and reassurance. You’ve been supporting people for many years so how do you continue to do that without reliving that kind of stress yourself and getting burnt out?
Frederick: I think my training as a therapist has helped in terms of my own self-care and being able to empathize, but also detach when necessary. Also, my own healing from the withdrawal experience has helped. I would say that seeing witnessing people heal is what creates the balance. The most challenging part of my work is seeing the suffering and the ways in which people’s lives are devastated.
When I get that first call and the person is in shock and completely traumatized because he or she had to give up work or move back in with parents, in some cases seeing the breakdown in relationships or children taken into care, the, or the financial impact, people losing their homes or declaring bankruptcy. That’s always hard. I would say that’s the hardest for me, nothing is more challenging than witnessing the devastation and nothing is more rewarding than witnessing the healing.
Moore: Before I knew too much about this world, I was shocked to find out how much prescribed drug injury can affect a person’s entire life. You mentioned housing and work and family, and the drug injury affects all of those parts of a person’s life, doesn’t it?
Frederick: It does and I think the only other thing that’s challenging is seeing people being misdiagnosed and given inappropriate treatment, or being told the symptoms aren’t due to withdrawal, or sometimes that no one else has ever had such a reaction. Certain things are difficult to hear and because I’m not a medic and there are times I can’t say anything. That can be very challenging as well.
Moore: So what can someone expect who comes to talk to you about their withdrawal experience or prescribed drug injury?
Frederick: It always depends on what the person needs. Some people just want to talk to give their family and friends a break, they just need a listening ear. Others want to know what are the best coping tools, some want reassurance. Some people want to ask specific questions like ‘have I heard of a certain symptom’ or ‘have I ever seen a case like this’, things like that.
I don’t give tapering or medical advice, so the focus for me is always on the person’s emotional safety and wellbeing and coping as best as possible. I always give priority to the people who feel like giving up. So my way of giving back is to devote my mornings to the people who are most vulnerable and at risk. We have an arrangement where every morning they’ll check in to see they’re going to hold on for another day. So we’ll do that with them until they’re well enough or they feel safe enough.
Moore: That’s so important to provide that connection. One of the issues I’m aware of is when the person who’s struggling with prescribed drug injury has family members who may not take seriously what’s happening to them, or may or may not believe them. So I wondered if you come across that yourself in your work and if there are ways to address that?
Frederick: I think the best support someone in withdrawal can have is at least one family member or friend who is willing to find out everything there is about withdrawal, to really research the subject. Even if it doesn’t make sense to them and they can’t relate to what’s happening. You give the loved one the benefit of the doubt and you just be there for the person. You become that person’s safe person in terms of someone they can approach if they feel overwhelmed and you just give the loved one unconditional care. So doing your best to understand the complexities of the symptoms.
I’ll mention here the concept of emotional dysregulation because that really affects relationships and how support is given and received. That’s where emotions are magnified or they are extremely intense. Sometimes they can be inappropriate or they can just surface out of the blue. People describe them as being off the charts or unnatural or out of character. They’ll say “it’s nothing like me, but I’ve become so paranoid”, things like that.
I think it really helps when the family member or friend understands this and is able to accept that the loved one may be acting like a stranger but that it is withdrawal-induced and not to take it personally. Acknowledging that the healing process is not linear, I think that’s very important as well. It means that the person may find it difficult to commit to social events or any plans that are too far in advance. Some people in withdrawal will only know on the day or even maybe an hour before how well they feel.
Being pressured in this regard can be very stress-inducing. If a family member or friend cannot relate to the withdrawal experience, I always say, “please trust what you’re being told” because it’s easy to say “pull yourself together” or “why don’t you go back to work and stop hanging out with those people on the internet?” and “why are you so obsessed?”
The isolation that the loved one can feel, this is the very reason that people flock to the internet and go for validation from the online groups. So I find that the family members and friends who are more accepting may not have that problem as much as those who are against the person being supported online but aren’t able to relate to the experience or be open enough to learn.
Moore: There’s a similar question around prescribers. Dealing with prescribers who might be resistant or who reject any suggestion that the drugs could be a fault, preferring to blame the individual. Do you have any advice for clients in terms of approaching their prescriber about what they’re going through?
Frederick: This is a difficult one for me because as a psychotherapist, I have to be very careful. Even a simple comment like ‘that taper sounds quite rushed’ can result in accusations of practicing medicine. I actually know of one counselor in the US who was sued by a client’s doctor for that very remark.
So what I do, what works best is putting something in writing to the client. For example, a client might come to me saying, oh, my doctor has said: “I want you off the Prozac by the end of the month”, or “we need you off this Valium” that sort of thing. Of course, this person has been in the groups and has seen how they could end up with seizures or psychosis or they could die.
What I do then is write a letter paraphrasing the client’s concerns. Here are the NICE (National Institute for Health and Care Excellence) guidelines and I’d maybe quote what is relevant. Then the client would take that letter to the doctor and then it’s in the right context. What I find is that written communication can be most effective.
The other advice I give is to make sure that the person mentions the physical symptoms if there are any. The reason is that the minute you mentioned the anxiety and panic attacks and paranoid or obsessive thoughts, any anhedonia, any of those symptoms, of course, the risk arises of being labeled with a mental disorder, or your doctor taking out the prescription pad for an antipsychotic.
I’m not saying lie or don’t mention them, but mentioning things like the muscle pain and digestion issues, tinnitus, numbness, headaches, the physical symptoms, this can create more of a balance. Don’t be surprised if you’re told that no one has ever had a reaction like yours and this is your underlying condition that has come back. They are famous for saying that or that you need to go back on the drug. See, you’re not doing very well without it. So the withdrawal itself is not acknowledged at all.
Moore: That’s so difficult to confront isn’t it. I like the sensitive, documented way that you approach a person communicating with their prescriber because the person can feel between two sets of advice quite easily and if they mention the internet, doctors get very unhappy with that.
Frederick: They do. Here we have our guidelines and the other thing would be of course to take the Ashton Manual as I did to the doctor. I do have people call me from the doctor’s office and I have spoken to doctors but usually, there’s a little bit of condescension. I’m seen as that overly zealous recovered patient.
The other thing would be to direct them to websites that are scientifically based such as the Council for Evidence-based Psychiatry or the Benzodiazepine Information Coalition or the W-BAD website. Maybe asking the doctor to please be open enough to check one of these sources of information so that doubt that what you’re saying is true or this ‘it’s all in your head attitude’ can be diffused.
Moore: I was also wondering, in your experience from the interactions that you’ve had, whether there are coping techniques for those withdrawing from benzodiazepines that you might recommend for people?
Frederick: I think that no one size fits all but the most important thing that everyone should attempt at least is acceptance. By that I mean not fighting the symptoms and acknowledging that knowledge and that whatever is happening needs to happen in order for the healing to take place.
For example, Professor Ashton used to encourage me to tell someone experiencing sleep difficulty to look at it as the body needing to be awake in order for some aspect of the healing process to work. That being awake is necessary to get to that point of healing. I’ve seen people with the same or similar symptoms have completely different withdrawal experiences based on then the non-acceptance or acceptance of the symptoms. So that’s very important. If the symptom is common and known to be a part of the withdrawal experience, then telling yourself that what is happening is normal can help.
It is important to see your doctor and to have diagnostic tests when necessary, especially if a symptom could be caused by a medical condition. I always say to people, any bleeding or abnormal growth, there are certain things we can’t just say ‘oh, it’s withdrawal’. If a person is experiencing something that is confirmed as withdrawal related, then normalizing is key.
There are other things like breathing exercises, it doesn’t work for everyone, but some people find them very calming. Grounding exercises, interacting with nature if you can and looking after yourself, eating healthily. If you’re able to go for a little walk, even if you can’t go out into nature but just moving the body in some way, for those who are able to that’s good. And then engaging in a hobby, some way of healthily distracting and definitely taking breaks from the online groups and from comparing notes. Distance from the information overload and the vicarious distress.
Moore: That’s really valuable for people out there listening. You are known in the online withdrawal community for your steadfast insistence and reassurance that everyone recovers from prescribed benzodiazepine withdrawal and injury. That struck me as such an important message because it’s one of hope which is perhaps one of the first things that people lose when they enter this world. So I wondered, is it, your experience in helping and supporting people through this difficult journey that underpins that message?
Frederick: When I started supporting people in withdrawal, I wasn’t as confident as I am now. At that time there was an online protracted withdrawal group, this was in 2006. There were people there who had been suffering from the late 1990s and others who were two, three or four years off. Some of them would write that ‘some of us don’t heal’ and I know people still write that in the groups.
What happened was back then I started to notice that one by one they all healed and they moved on with their lives. So that was when I thought ‘it looks like everyone eventually gets better’. Then in the earlier days, I would call Professor Ashton or Una Corbett who has passed on now, I would call them to ask if I had a really complicated case, all this has happened and so many drugs and ECT, and I would ask do you think that person will heal? Always, they would say ‘everyone heals, but they must give it time’.
Ian Singleton at the Bristol and District Tranquiliser Project said the same thing. Paul Entwhistle and Hilda from CITA, which was a withdrawal support charity in Liverpool, UK, they told me the same. So I’m not just the only one who says it but the longer I do this, the more I find it to be the case. I’ve seen people who were on six or eight, even 10 different meds who were cold-turkeyed, reinstated, all sorts of complicated scenarios. People who felt trapped and that they wouldn’t make it. I’ve seen people who were extremely protracted, who disappeared from the groups and who are still my friends but they would write to me privately and little by little I’d see them get better.
I’m not saying that everyone will heal from every single symptom but usually, people have residual issues. For instance, tinnitus is one that I understand some people have permanently. I haven’t had anyone who did but I hear this to be the case. They say that it’s nothing compared to when they were in withdrawal or they can live with it.
In terms of someone being stuck in withdrawal indefinitely, I’ve just never seen this. When you consider neuro-plasticity and the brain’s ability to form new neural connections and how the brain adjusts and adapts to changes and how it compensates when there is injury. This is what I’ve seen in withdrawal. I don’t think I could do what I do if I saw someone not heal. It’s just too cruel
Moore: Baylissa, thank you. That’s such an important message because I feel that while there’s hope, there’s always reason to get up every day and keep trying isn’t there?
Frederick: There is and I think it’s important, even if you’re not convinced and still doubt me, don’t give yourself that verdict. Give yourself a chance to see what your story will be. Don’t hold onto some story you’ve heard that you maybe don’t even have all the facts for. Wait it out.
Moore: We are sharing this podcast on World Benzodiazepine Awareness Day itself and it occurs on July the 11th in honor of Dr. Heather Ashton. You have mentioned her a few times and I know that you and she developed quite a friendship. So I wondered what was she like and what did she think about this whole issue of benzodiazepines and the way that prescribed long term and how people are left with so little support when they do try and come off?
Frederick: Happy birthday dear Heather! It’s a little bit emotional for me but Heather was just a remarkable human being. I first met her when I contacted her to ask her to vet the medical information in my book and she was just lovely. Somehow we formed a special bond then and that continued and I did have the privilege of meeting her in real life as well. Sometimes we’d speak three or four times per week and I would run everything by her in terms of the advice I was giving. She was really a good mentor to me.
In terms of the community, she was just always a hard worker, she was a pioneer but she never relented in her support for Barry Haslam and Mick Behan and all the people who were working very hard at the time. Some people who aren’t here anymore, like Colin Downes-Grainger who passed away, Reg Peart, there many who have gone on ahead who worked really hard. She did everything she could to support them and to support our cause. I think we’ll always be indebted to her for not having turned a blind eye and for her sense of strong sense of justice.
She was just selfless, dedicated, she helped anyone she could. Personally, she was just so much fun and she had the best sense of humor. She wrote lovely, very engaging short stories and she was also quite good with her artwork, watercolor painting and so on. Tennis too, she wouldn’t miss her Wimbledon. She was just good fun and a good person and I miss her dearly.
Moore: She has a quite incredible legacy doesn’t she and I have to say that the work that you are doing, the work that W-BAD does and the Benzodiazepine Information Coalition and Barry Haslam and so many other people, you are the ones keeping her legacy front and center and I’m so grateful for that.
Frederick: Thank you, James, it’s not comparable what I do but I always try to keep my integrity.
Moore: As we come towards the close, I wondered if there’s any message that you’d like to give to anyone listening who might be in the middle of the maelstrom of coming off benzodiazepines?
Frederick: First of all, I would love you to acknowledge that what you’re going through is by no means easy. People in withdrawal can be hard on themselves, not acknowledging how heroic they are, that there are many people who start this journey and they can’t do it. They reinstate and they disappear because it’s just too difficult. So, please acknowledge and validate your courage and your strength and know that yes, you will get better. Even if you don’t believe me, you will still get better in time.
Do everything you can to protect yourself whether it’s from overload of negativity, please take breaks from everyone else’s story because sometimes it becomes too overwhelming and it can make you lose sight of the fact that this is a healing process. So this is you healing, this is what it takes to heal. If you hold on and just keep going, find a way to get through the days, you will make it to the other side.
You are talking to someone who was convinced she was dying and here I am today, as happy as a Lark, annoyingly happy, but happy nevertheless. This too shall pass.
Moore: That’s wonderful, thank you Baylissa and I just want to say that your work and your support to people in the most terrible situations is so deeply appreciated. Thank you.
Frederick: Thank you, James, thank you very much for your work as well.
Moore: I want to say a huge thank you to Baylissa for taking the time to chat and you can find out more about her work by visiting her website.
I also want to thank all our W-BAD guests, Angela Peacock, Jim Wright and Baylissa as well as Nicole Lamberson for all her help and support in making these podcasts and for everything she does in support of World Benzodiazepine Awareness Day. Finally, thank you to you for listening.
****
MIA Reports are supported, in part, by a grant from the Open Society Foundations



Thank you James and Nicole for your hard work.
And thank you Jim Wright. Glad to see “anecdotal reports” as evidence. That really should be the only evidence, since the doctors and researchers refuse to ingest these poisons.
And yes, they are ALL informed as to the dangers, the clients tell them so. Besides, there is no test and no measure in any scientific way as to the damages. They are too numerous and many occur over time and the body being so intricate, it’s impossible to understand. So it behooves the most rational as to why create something dangerous without actual knowledge and why, for something that they do not understand in the first place.
I would like Jim to go to my appts or my emergency visits where I am treated like a criminal for refusing to ingest poisons, for a physical condition. Where if you do not agree to labels you don’t even have, you are treated as if you do.
Jim is canadian so I am sure he knows the depth of abusive garbage.
I also know that for Jim to keep his job, it is impossible for him to become “radical”.
I’m sure he’s disliked enough for the valuable role he plays.
So thanks Jim for going the extra mile. It’s not helping any of us at each of our hospitals and providers. That is only ever solvable by stripping the ordinary GP and shrinks of their power to do what ever the hell they want as long as they pass the “college of physicians and surgeons”, which are just part of the abuse.
And thank you so much Baylissa, wonderful work you are doing, saving lives in a real way and supporting people in positive ways. Thanks to everyone who worked hard in your organization. These efforts are beyond valuable as education to the public and can act as a prevention and warning.
Report comment
I’ve wondered for some time if niacinamide would be useful in benzo withdrawal because both classes of neurochemical use the same receptor sites. Its close family member, niacin (nicotinic acid for you pharmacology types) safely speeds up alcohol withdrawal to within a few days- I’ve used it in a withdrawal at an individual’s home (!!!?) successfully, though I wouldn’t recommend it for self-withdrawal.
Report comment
bcharris
I don’t know how many times I’ve told you…and others too.
Those of us who have successfully d/cd benzos remain very very very sensitive to many substances…B vitamins jack up our nervous systems! Not your cure-all!!
Check out the forums on BenzoBuddies–they will validate what I’ve been trying to tell you for YEARS now. We cannot handle B vitamins!! I am just now, 6 1/2 years later, finally being able to handle a bit of supplemental Methlyfolate. Yep. Have that genetic klinker MTHFR factor thing-y, as do many of us who end up with PAWS.
Report comment
furies-
I’ve yet to hear of a method that works for everybody: b vitamins, yoga, pharma, ect, neo-Freudian psych, retreats, et cetera. I’m glad you are mindful of your sensitivities, and we perhaps both agree/hope that your new trial B9 for MTFHR will be beneficial. Apparently it has not triggered & jacked upped your nervous system? I think it’s possible taking niacin and flushing for years gave me rosacae, too high dose niacinimide gave me liver damage, then eventually headaches though I took it for years at lower doses without a problem. But I continue to take inositol hexaniacinate, in high doses, and wouldn’t go without it. Even the niacin did a number of profound things for me. B vitamins can have undesirable effects too, but personalizing it and adapting is part of it. I’m trying to be comprehensive and honest while not throwing the baby out with the bathwater. I maintain there is a place for all b vitamins—all nutrients—including methylfolate. Some rare individuals with a genetic disorder or sensitivities can’t take vitamin c even though it’s generally one of the safest substance known. And, yes, I’m keeping the diarrhea in mind.
Report comment
Just relaying my experience from being on BenzoBuddies/Surviving Antidepressants lo all these years.
From what I read in the threads, almost universally, B vitamins cause overstimulation problems. I could not sleep for years and believe me that was my first priority.
and yes, I do still get jacked with the Methlfolate. I only take it if I’m experiencing a run of ‘window-ish’ relief. Which hasn’t been lately.
Yes, everyone is different. But there’s huge commonalities, too.
Report comment
One last comment for me:
I do agree that b vitamins can give energy and sometimes too much or in a jittery way. B-complex is often given to boost energy and mood…sometimes uncomfortably so. It is important to recognize the differences between what are at least 8 different B vitamins. B6, B12, & B3 are known for boosting energy in one way or another. But B3 also has anti anxiety effects, and I know a person who took 500mg niacin(B3) before bed that helped her sleep. B6 for autism is often prescribed with magnesium to help counter its activating effects. B1, B3, B6, B9, & B12 all have antidepressant potentials. I think B3 can give ‘energy’ but also calming effects. I believe it activates receptors in a similar way to benzos, but it’s been awhile since I’ve looked into it.
Report comment
Thanks James for this compelling interview with Dr. Jim Wright in follow up to the World Benzodiazepine Awareness Day 2020 (W-BAD) and the informative, revealing Medicating Normal film. It is very heartening to see so many good people working to expose the harm and suffering caused by benzodiazepines and other damaging psych drugs. Thank you Angela Peacock, Nicole Lamberson and everyone involved in producing the film.
Thanks to Dr. Jim Wright for his knowledge and expertise in speaking out on the harms and potential harms of drugs that somehow have managed to be ignored for so long while being so loosely prescribed to so many unsuspecting people.
Thanks to Baylissa Frederick for bringing her knowledge, compassion and humanity in helping those who are dealing with the impact and horrible withdrawal of these drugs. My younger brother was one of the unfortunate ones who succumbed to a combination of benzos and SSRI’s and I hope the day comes when this never happens to another person.
Also must thank Robert Whitaker for all his amazing work as well.
Report comment
My comments address both interviewees: I actually believe people are designed for drugs, namely chemicals or biochemicals. The usual suspects are of course micro and macro nutrients, which are typically viewed as obtained through food and beverage, particularly a ‘balanced diet’. I would broaden the chemical need/want to other non-nutritional substances. However, I find it interesting that Baylissa mentions she’s had a number of clients come in for magnesium withdrawal. This is interesting, and I won’t say much, but what I will say is this: Does she believe that the RDA (recommended daily allowance) for nutrients is a reliable guidepost for society? If so, does she believe people eat and, even with a so-called balanced diet, obtain the RDA for magnesium? Do people Really eat enough leafy greens to get 350-450mg of magnesium per day? The same applies to most nutrients, but especially vitamin e, iodine, and omega 3’s. Are people Really eating enough fish 2-3x a week, iodized salt and seaweed, olive oil and avocados, or leafy greens? If so, I solute them. But let’s be real. Therefore, if someone chooses to take a supplement, they are not stretching the envelope based on this consideration. And this is for the RDA, let alone optimal amounts for preventing/treating illness and increasing well being. Jim says there’s no supplements that can help withdrawal. I completely disagree, but I won’t elaborate, other than to agree with bcharris’, another commentator’s view on vitamin b3, in this case niacinimide. Taking higher doses of supplemental nutrients, and suddenly stopping, Can create rebound/withdrawal effects, for example high dose vitamin c when taken in large daily doses should not be suddenly stopped in the hospital, for example. But I guarantee you the hospital staff will not offer, let alone taper, vitamin c through controlled supplementation. Also, nutritional withdrawal is usually relatively mild—and also begs the question of removing effects that really can be useful. I didn’t hear her describe the undesirable effects of magnesium, just its removal, although of course nutrients can have undesirable, even harmful, ‘side effects’ too. Anyways, other than these remarks, I rather appreciate the interviewees’ work. It’s a complicated issue, and conventional medicine hardly bothers, so they are compensating a neglected area. For this, I also solute them.
Report comment
The belief that counseling cures benzo-dependence remains baffling.
Ashton claimed that when a “cut” was too ambitious , just place more time between cuts. Well if the cut is a problem today, will it be just fine later? Oh and the cut and hold method is not intended to reverse benzo-dependence, and “healing begins after the taper is competed”? What is the function of the taper then? Some of these beliefs live on with no validation and no questioning.
Oh just jump? Look at the people who did. If you are tapering with a number and are doing well, why would you suddenly make one big cut to end it? Yet people did just that.
Mostly the BenzoMicroTaper has been so corrupted through the years that the current versions ignore basic chemistry. The current and mangled versions place any benzo in water! Clonazepam and Diazepam and more are poorly soluble to insoluble in water. That means that the benzo is in suspension at best and not in solution. You never know how much you are cutting. It’s a return to the invalid water titration thing. These benzos do not mix well with water. The taper becomes a crap-shoot.
Why don’t people look up these things? Solution. suspension are not identical. Suspensions precipitate! even with suspension agents they precipitate.
Does it make sense to determine any cut by deciding how many days you will be tapering and then divide your benzo dose by that number of days? Really? Is that not backwards?
I was one of the first people to recover using the authentic BenzoMicroTaper of 2005. The corrupted versions of today are missing the two essential elements that changed the benzo world. Why does it not “work for everyone?”. Not “everyone” is really using it.
Now for the 10% commandment, there is no evidence that the correct or acceptable cut will be identified by a percentage of anything. The 10% was suggested only as a ball park limit for any psychoactive medication discontinuation step. It was not a suggested cut limit.
People, especially heavily damaged people, are harmed by not reading carefully and by accepting hearsay.
The level of verified benzo information has fallen dramatically in the last few years. It may not be intentional; it may be carelessness; it may stem from limited education.
The ad hominem argument has replaced the ad hoc, and the result is bad science and more suffering.
Report comment