Editor’s Note: This article first appeared on our affiliate site, Mad in the UK.
In Part 1, I looked at the longer-term inefficacy of ‘maintenance treatment’ with antipsychotics, and also at some ‘disappointing’ outcomes for ‘early intervention in psychosis’ (EIP). Part 2 examined, what I take to be some ill-founded assumptions supporting their continuing employment.
If long-term reliance on treatment with neuroleptic drugs appears increasingly unjustifiable, what can be said about their use in the first instance?

After a look at that question here and keeping in mind some of the issues that evaluations of early intervention have raised, I’ll consider some alternative measures and adaptations services might incorporate into their approach; with the aim of avoiding both those ‘disappointing outcomes’ and the higher rates of morbidity associated with ‘maintenance treatment’.
The case for developing new approaches to research and treatment is compelling. Some parts of my discussion here are more exploratory in nature, while the evidence for other recommendations is already well established.
If I were to sum up briefly my view on EIP, I’d say it has aspects that are good, some that are bad, and others that are ugly:
- the good — psychosocial support can provide practical psychological resources
- the bad — high rates of ‘bycatch’ and misdiagnosis
- the ugly — potential pathway to dependence and chronicity
I’ve previously outlined one way some of the more damaging consequences of psychiatric treatment may come about. The experience for patients can be tortuous when adverse effects from psych drugs are misdiagnosed as symptoms of psychiatric illness. This can often result in their suffering increasing estrangement and loss of agency, as well as causing lasting morbidity through exposure to psychiatric poly-pharmacy.
Shorter-term efficacy of neuroleptics
But mainstream psychiatric practice insists that the use of dopamine receptor blockading neuroleptics for psychosis is indispensable. Let’s give this claim some scrutiny. Just how well founded is it?
Firstly, the drugs are typically judged to ameliorate only, if at all, what are called ‘positive symptoms’ of psychosis and not the ‘negative symptoms’ of affect, or any cognitive impairments. In fact, some leading ‘molecular psychiatrists’, like Oliver D Howes, recognise that the drugs may, in fact, worsen negative symptoms; impairments that may impoverish a person’s quality of life, occupational and social prospects.
Also now recognised by these ‘molecular psychiatrists’, is that some psychoses, such as that putatively associated with Parkinson’s, can improve with a drug that does not block dopamine receptors.* Hence, the causal origin of such cases cannot be said to lie in ‘excess dopamine synthesis’. It follows that many cases of ‘treatment resistant’ first episode psychosis (FEP) will likely also have some other origin.
Nevertheless, the drugs remain the mainstay of treatment. Their ongoing use typically justified by appeal to statistics. For instance, according to a meta-analysis of clinical trial results, twice as many patients improve with antipsychotic treatment as improve with placebo. A finding derived from double-blind randomized control trials (RCTs), the so called ‘gold standard’ for medical research.
However, it is documented that ‘unblinding’ in these trials is common.** And, as discussed in Part 1, many antipsychotic trials’ methodologies are based on keeping one group of patients on their pre-existing drug regime and switching the other group from that to placebo in a very short time-frame. A procedure likely to result in ‘rebound’ psychotic symptoms from abrupt drug withdrawal.
Placebo helps. Why?
But for the sake of argument, let’s take that statistic at face value: twice as many patients improve with antipsychotics compared to placebo. Conversely then, if my grasp of maths is up to anything, half as many improve with placebo as with the drug treatment.
The rate of ‘non-responders’ to the drugs is generally reported to be around 30–35%. This rate of ‘treatment resistance’ seemingly tends to increase over time. For antipsychotic naive FEP patients, perhaps only 20% fall into this bracket. However, 50% or more of those receiving ongoing attention from services for ‘chronic schizophrenia’ may be deemed ‘treatment resistant’. Increasingly poor drug response over time may largely be due to cumulative exposure resulting in dopaminergic supersensitivity; as the brain’s density of dopamine receptors increases — its natural adaptive response to their blockade.
But let’s say that roughly two thirds of those prescribed neuroleptics do ‘respond’. So, roughly half this number, a third of patients will show some improvement when treated with placebo; following the implicit conclusion of that meta-analysis. That is, they improve without taking antipsychotics. This is a significant phenomenon and one that merits serious attention.
Of course, no one suggests using placebo pills in routine clinical practice. Nevertheless, I think it is worthwhile thinking through what might be happening in these cases. My interpretation would be that this is due not to placebo effects as such, but reflects that participants in a research trial should be; receiving appropriate attention in the form of supportive care from professionals, and any support network they may have. Additionally, that they are allowed some period of time, with suitable rest and settings, in which any symptoms or disrupted functioning may, potentially, resolve of their own accord.
It seems likely to me that this one third of patients improve, in the main, due to the generalised benefits of receiving appropriate care, rather than any beliefs about dummy pills they’re taking.
Non-drug based support
Recently, there have been a few feasibility and pilot trials on non-pharmacological interventions, such as cognitive behavioural therapy (CBT), including the Orygen trial I mentioned in Part 1. They have demonstrated:
- Firstly, that deferring antipsychotic treatment can be done safely. Concerns that this would mean extending the ‘duration of untreated psychosis’ (DUP), potentially worsening longer-term outlook were shown to be unwarranted. A separate study in Finland found that immediate use of antipsychotics for FEP actually lead to worse outcomes five years on, than initially withholding their use.
- Secondly, the ‘non-inferiority’ – in terms of both symptom management and social functioning – of more intensive psychosocial interventions compared with neuroleptic based treatment. (More details on these trials in the footnotes below)***
It has to be acknowledged that these trials were very selective, in that their participants were limited to those willing to engage; ‘help seeking’ individuals not showing aggression, suicidality or other behaviours that would tend to exclude them from a trial. But such selectivity is common in antipsychotic trials, where more ‘challenging service users’ tend to be excluded.
These limited pilot and feasibility studies appear to replicate the results of an earlier more comprehensive research project carried out in California in the 1970s. Headed by Lauren Mosher (then lead psychiatrist for the NIMH), the Soteria Project was based on a model of intensive psychosocial support, called ‘being with’, provided in a home-like residential setting. Where patients could be supported to work through their ‘altered experiences’. Soteria demonstrated that recovery was more than possible without the use of neuroleptics, or with their use much reduced.
The approach “was as successful as anti-psychotic drug treatment in reducing psychotic symptoms in 6 weeks”. And resulted in “better 2-year outcomes for patients with newly diagnosed schizophrenia spectrum psychoses,” when compared with hospital based treatment. Patients were generally enthusiastic about its minimal medication approach.
Other projects would take up its model in the US and elsewhere. The professional insights and guidance gained from the experience of these long-running projects shouldn’t be lost.****
Among the advantages of more psychosocially based models, is that a majority of young people will likely prefer to engage with practical psychological input around social functioning, rather than with clinical management of symptoms. Approaches informed by lived experience such as ‘Hearing Voices’ can enable some to come to terms with their ‘symptoms’ and live well with them.
While a minority of patients may be unwilling to partake in ‘talking therapies’ – perhaps due to cultural factors or beliefs about drugs fixing ‘chemical imbalances’ – it is widely acknowledged that rates of ‘non-compliance’ with ongoing drug treatment are high; due to the drugs’ many adverse effects.
Psychosocially focused interventions may foster better engagement. A more collaborative approach, with greater scope for the client’s self-determination about their care, is more likely to build trust than the coercive approach services often take.
Ensuring that the benefits of psychosocially based approaches can be provided to a less selective group of patients would be a practical challenge. But could revolve around an individual’s progress over time and potential adaptations to existing service models. There are plenty of possibilities already established as both safe and effective. Five decades on from the first Soteria project, I believe its model can be taken and improved upon.
Biomedical approaches: Being wary, but open minded
There are, apparently, new drug treatments in development and said to be promising. Revolutionary new approaches are occasionally touted in the media, but then nothing seems to come of them. I can’t rule out that newer drugs may be better — which is to say, less bad — than neuroleptics. But as I argued in Part 2, drug interventions targeting a single aspect of the brain’s function are likely addressing only one aspect of a multifaceted causality that plays out through functional level network effects, not identifiable with molecular processes.
Given the current level of neuroscientific understanding of causality in the brain and nervous system, it seems pretty much inevitable that exposure to pharmaceutical psychotropics will produce adverse consequences. Even if the harms are not properly recognized or understood till decades later.
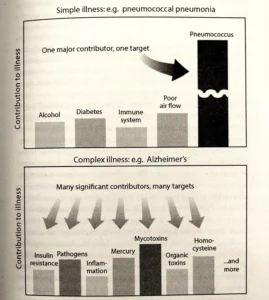
I concluded before that assumptions of ‘underlying illness’ are unwarranted, inasmuch as these assume a single disease process. We are probably talking about multiple aetiologies; arising from a patchwork of susceptibilities, both innate and acquired, and likely triggered by the presence of external stressors — where a person’s conscious interpretation and ‘window on the world’ also play determinative roles. These latter are clearly not reducible to biochemical processes.
Working with a framework like this can, I think, help remove some of the mystery around the typical course of ‘relapse and remission’ that a simple disease model of ‘schizophrenia’ does little to explain.
If the causality cannot be taken as simple, then it stands to reason that interventions also have to be multi-dimensional, rather than focused around a single variable only. Where no single factor stands out as a necessary or sufficient cause, a broader approach is called for.
The graphic below is discussing Alzheimer’s, but I include it here to illustrate the principle in general.
Adjunctive or supplementary interventions
Having some wariness of drug interventions needn’t entail that we dismiss out of hand any role for ‘therapeutic molecules’. Trials are looking at the role adjunctive treatments can play. Among them Cannabidiol, Omega-3 oils and N-acetyl-cysteine (NAC). The latter appears to be a safe intervention that can regulate glutamertergic signalling — which neuroscientists identify as one mechanism potentially leading to psychosis.
Although such ‘supplementary’ treatments are generally assumed to be of marginal benefit, their risk profile is accepted as low. And I think it is fair to surmise that the benefits of such interventions may be masked in trials where patients are maintained on higher doses of one or more psychiatric drug.
Combining such adjunctive treatments may add up, synergistically, to more significant benefits and for symptomology more broadly, including the ‘negative’ and cognitive symptoms that ‘antipsychotics’ don’t help.
Ameliorating factors like oxidative stress, neuro-inflammation and mitochondrial dysfunction with such interventions may have ‘neuroprotective’ effects, as well more general health benefits. This could contribute to better levels of ‘functioning’ and sense of well-being. Interventions like these can be made safely and at relatively low cost. So what is there to lose?
At the end of Part 1, I noted that neuroleptics cause cerebral atrophy. This is a rather grim fact. But the brain is a remarkable thing, and there is not a simple relation between the function of the mind and the matter of the brain. Neuroplasticity and neurogenesis are scientifically established phenomena.
Suitable exercise, mental stimulation and appropriate nutrition can be conducive factors allowing for recovery of healthy brain function. Awareness of this potential should, at least, have a role to play in guiding how services approach ‘sustaining remission’, and the advice they offer.
To take just one example that might warrant further research, there is some indication Lion’s Mane mushroom used as a supplement may aid recovery from nerve damage. “Pre-clinical testing found the lion’s mane mushroom had a significant impact on the growth of brain cells and improving memory”. Shouldn’t psychiatric researchers be interested in knowing more about the potential of such ‘nutraceuticals’?
Why is there such resistance to alternative approaches?
Research programmes tend to be based around identifying single causes and proposing mono-variable interventions. Consequently, approaches that don’t easily fit into this research model – focused around RCTs – will likely not be given fair consideration.
For instance, the Bredesen Protocol, thought to be a quite promising approach to Alzheimer’s disease, has been discounted because it isn’t “targeting a common underlying neuropathological process of Alzheimer’s disease”. But the point is, that the existence of such a ‘common underlying process’ cannot simply be taken for granted.
A focus on identifying single factors may well be reasonable scientific practice in many fields. But it may belie the nature of living, adapting, neuroplastic, incredibly complex and sensitive human brain and nervous system.
Moreover, the funding model for healthcare research, in general, seems geared towards developing patentable and marketable products. An imperative that prejudices those whom have the final say, about what proposed solutions should look like. This then blinkers society at large against potentially helpful interventions that don’t fit the established pattern and its assumptions.
In summary
Until such time as there is a comprehensive understanding of causality in the brain and nervous system, with low-risk drug treatments truly proven as safe and effective; mental health services should prioritise harm reduction. Here are some suggestions, perhaps readers can add to them:
- Allow time for ‘help seeking’ individuals to get support and respite in less jarring settings. Taking a ‘watch and wait’ approach before resorting to the use of neuroleptics.
- The provision of psychosocial support and resources to enable patients to come to terms with altered experiences, should be given equal weight with drug based management of symptoms.
- Any ‘critical period’ of neural plasticity in the typical age group for onset of FEP should caution against immediate intervention with psychotropic drugs — against the current presumption in favour of use at the earliest. Perhaps there may be some limited role for sedatives in the more acute stages of a crisis.
- The prescription of SSRIs (and also SNRIs) to those with milder mental health problems should be avoided. They’ve been shown to increase the likelihood of patients developing more intractable issues. Greater education on the drug interactions and risks of pharmaceutical psychotropics, for both prescribers and patients, is required.
- Reducing the toll of neuroleptics and other drugs on those who already have treatment histories should be a greater priority than present. Moncrieff et al have proposed that there is a need for specialist ‘deprescribing services’. So that the risks of clinically mismanaged drug discontinuation — currently commonplace through lack of awareness — can be properly addressed. Alternatively, ensuring there are staff members on teams that have this training and understanding — in order to support those stable in remission to reduce step-by-step according to hyperbolic tapers, and as their personal circumstances allow. Enabling ‘managed reduction’ should reduce the temptation for service users to discontinue covertly.
- An understanding of ‘dopaminergic supersensitivity’ and ‘rebound’ effects from drug withdrawal must also inform both the design and evaluation of trials of ‘antipsychotics’.
- Research should focus not only on mono-variable interventions, but allow for a broader range of complimentary measures. Accordingly, there may be a need for research to incorporate ‘observational’ and other methods of evaluation, rather than relying solely on RCTs.
- Services should encourage and support patients to take up regular exercise, and also to eat healthily; providing advice on suitable nutrition for maintaining recovery.
Pragmatically, we should be exploring a raft of safe interventions, understanding that any susceptibility to psychosis isn’t separable from a person’s general health and well-being. By covering more bases (at least the easier ones to cover), finding and sustaining incremental gains, we may enable ‘recovery’ in a fuller sense of the word.
Footnotes:
* Pimaversin’s mechanism of action is said to be unestablished, but thought to be due to antagonist effects on serotonin receptors. If a drug that dampens serotonin receptors is considered to have an antipsychotic effect, this would underscore the risk of SSRIs triggering psychosis and mania. SSRIs heighten serotonergic signalling.
** Due to the heavy side effect profile of ‘antipsychotics’, it is very likely that trial participants taking them will realise they are not in the placebo group. This is likely to produce an expectations effect that would reinforce any subjective perceptions of improvement.If you had rapidly gained weight after starting the pills, it would be natural to want to believe they were of some benefit to your mental health symptoms, wouldn’t it?Such effects will likely boost the apparent efficacy of the drugs in research trials. In fact, low levels of weight gain amongst trial cohorts can be taken by researchers as indicating poor adherence to a trial’s antipsychotic drug regime.
*** Pilot and feasibility trials assessing the efficacy of psychosocial intervention compared to antipsychotics:
- Orygen, Melbourne, Australia: Psychosocial intervention with or without Antipsychotic medication for first episode psychosis
- UK NIHR 2020 feasibility trial: antipsychotic medication versus psychological intervention…adolescents with first episode psychosis
- Manchester 2018: Antipsychotic drugs versus cognitive behavioural therapy versus a combination of both in people with psychosis: a randomised controlled pilot and feasibility study
Although the papers indicate that there may have been some use of medication in the placebo/psychosocial treatment arms, the trials at the very least, show that dosing much lower than standard does not simply translate into a loss of therapeutic effect. Which is, in itself, an important finding encouraging of greater openness towards deprescribing. Especially, when combined with an understanding of the ‘hyperbolic’ relation between dose and D2 receptor occupancy. Mark Horowitz’s work shows that very low doses can be efficacious.















More than 10,000 research papers were retracted in 2023 – a new record
From the NIH…
be careful not to site bogus studies…to many to count
Report comment
My Partner, who is 66 years old, was diagnosed with Parkinson’s disease last year. We noticed that he was experiencing hallucinations, slow movement, disturbed sleep, and twitchy hands and legs when at rest. He had to stop taking pramipexole (Sifrol), carbidopa/levodopa, and 2 mg of biperiden because of side effects. Our family doctor recommended a PD-5 treatment from natural herbs centre , which my husband has been undergoing for several months now. Exercise has been very beneficial. He has shown great improvement with the treatment thus far. He is more active now, does more, and feels less apathetic. He has more energy and can do more activities in a day than he did before. As far as tremors I observe a progress, he improved drastically. I thought I would share my husband’s story in case it could be helpful, but ultimately you have to figure out what works best for you. Salutations and well wishes
Report comment
I think money is the best treatment for all mental health problems. At least enough money to escape poverty have decent housing and health care and also to provide for transportation and leisure activities.
Report comment
I can’t argue with that one.
Report comment
Conventional psychiatric treatment is so bad that I think it should be considered the “alternative” treatment. I started looking for the causes and cures for mental disorders 28 years ago and the first approach I found that actually restores one’s mental health is “orthomolecular” medicine. It’s wonderful, has nothing patented about it, no side effects. The Am Psych Ass’n has been fighting against it since about the 1950s. Here in the US, there is no law that says psychiatrists must even try to cure patients—so they don’t. The APA could treat all their patients with voodoo and they wouldn’t even be breaking the law because there is no law to break. They have 100% freedom to choose any approach they like, and what they like are the profits from patented “medicines” and talk therapy. If you’d like to know more about the orthomolecular approach, I have 3 videos about it on YT at “Linda Van Zandt’s Mental Health Recovery Channel.” I’ve since learned a second approach, too, so my “incurable” “bipolar with psychosis” relative is mentally well and free of psychiatrists and their harmful drugs. Mental illnesses are curable but only if we correct their physical causes. Psychiatrists have no clue how to cure anyone because they’re taught to only match up symptoms to a patented, synthetic chemical and turn all patients into lifelong customers.
Report comment
Linda – I wonder if you would consider writing a post on this site explaining the basics of what you have learned about orthomolecular medicine. I prescribe a lot of folic acid, fish oil, and b vitamins. I am curious to know if that is along a similar line and how I can learn more about what sounds like a lost art
Report comment
Karl, I’m so happy you asked about the orthomolecular approach. Yes, it sounds just like what you’re already prescribing. I have 3 videos about orthomolecular treatment on Youtube at “Linda Van Zandt’s Mental Health Recovery Channel,” and have written a book which is mainly about my family’s experiences in getting conventional psychiatry out of our lives. It’s also a beginner’s guide to orthomolecular medicine. The title is “The Secrets to Real Mental Health” by Linda Van Zandt. (I used a pen name to protect my loved ones’ privacy back then because it’s such a personal story.) I’ve since learned to use homeopathy so now I’ve written another book about our experiences as well as the beginner’s guide to using homeopathy. It’s “Goodbye, Quacks – Hello, Homeopathy!” by Linda Santini. I don’t have any videos on it, I’m afraid. It’s available from Amazon but beware that if you buy the e-version, it still needs a bit of editing. The paperback is fine. Months ago MIA was interested in my story and these natural treatments so I did submit an article to them but they didn’t print it and seem to have lost interest. I’m happy to answer any questions you might have. Both treatments have worked wonders for my family.
Report comment
What Are We Overlooking?
We are overlooking all the “non-academic” work done for approximately the last century, as well as some work that has been done by “real” academics regarding the human mind.
What we need, to get to “square one,” is a more workable and comprehensive model or theory of the mind and of the human and its behavior. The “biomedical” model – based mostly on neuroscience – has long since proven totally inadequate. Even the small amount of work done by academic researchers (like Ian Stevenson) support this assertion. How does that model explain observations of verifiable past life memories? I don’t think it can. Obviously there is more going on here than a brain acting in a body in its sea of chemical compounds and electrical signals.
Outside of academia there is voluminous data available, based on research, that confirms the reality of reincarnation and related phenomena that can best be interpreted as “spiritual.” The longer the healing professions resist this information, the closer they will come to destroying what thin reputations and power they currently maintain.
Of all the named and formal human studies, only psychiatry and psychology are pledged by their very names to study the human psyche – the soul or spirit. The sooner they decide to actually start doing this, the more lives will be saved instead of wasted.
Report comment
“Of all the named and formal human studies, only psychiatry and psychology are pledged by their very names to study the human psyche – the soul or spirit. The sooner they decide to actually do this, the more lives will be saved instead of wasted.”
I’m not so sure about that. To me most of them seem too split off from their own souls.
IMHO.
Report comment
…. and what is most wrong with psychology and psychiatry?
Both lack reverence for human life.
IMHO.
Report comment
First, Larry, I’m personally thrilled to hear that studies prove reincarnation. I’m hoping my next life will be a whole lot better than this one has been. So thank you for mentioning this.
Second, I don’t understand why scientists/psychiatrists/psychologists call their chemical approach “biomedical.” There’s nothing “bio” about it. “Bio,” to me, means natural, related to nature. Psychiatrists’ psych chemicals are just man-made junk devised in test tubes, created for the purpose of making money, not curing anyone. How could they possibly cure someone when
A) that’s not what they’re designed to do. That would be like expecting cough syrup to cure pneumonia, which ain’t gonna happen, and
B) humans are not “chemical” but “biochemical” beings.
I used real biochemical medicine, aka “orthomolecular” treatment, to treat 2 of my family members. One was psychotic because his histamine level was too high. I could have left him on for-profit psych drugs for life because they artificially manipulate one’s histamine level but I wanted his mental health restored. So I did my own research. I learned from Carl Pfeiffer, MD how to naturally lower one’s histamine level. That enabled me to taper him off the 3 different, daily antipsychotics (in 4 months) and at that point he was mentally well.
“Orthomolecular” is real biochemical repair while psych meds are just chemical straight jackets, designed to cure no one. The APA has been fighting the orthomolecular approach since about the 1950s.
Sadly, the US has no law saying the APA must even try to cure patients, so they don’t.
Report comment
“Obviously there is more going on here than a brain acting in a body in its sea of chemical compounds and electrical signals.”
Larry, your thoughts on past lives are not only intriguing, but well worth considering, imo.
Report comment
But the Open Dialogue approach pioneered and rolled out in Finland has world beating results – 80% permanent remission from first episode psychosis compared to our 70% permanent disability in the West. Surely you have come across these results: it has made waves across the world. Their approach is to restrict the use of antipsychotics wherever possible to short term stablization if necessary, and then to conduct therapeutic sessions not just with the sufferer, but with the social networks, and we needn’t go into the reasons why this approach is so successful: but it does facilitate not just the direct confrontation with, observation of and understanding of ones own psychological difficulties, but it also promotes understanding among the mental health workers and those family and friends who attend the sessions, therefore allowing their family and friends to lose their fear and become more genuinely supportive. And because this support is based on listening to and understanding the person going through the difficulties, their support will be more intelligent and responsive to the persons real needs.
So what value has this whole article you have written if it omits to recognize the supremacy of this new treatment modality which has shaken the field of psychiatry? I’m afraid that even though Mad in America contains among the most critical intellectual perspectives on the field of psychiatry and psychiatric medicine, it has not swallowed, let alone digested, the important facts which all point to a picture of a totally fraudulent and harmful psychiatry, and a totally misguided, confused and impotent set of professions including all mental health worker and even critical psychiatrists and psychologists. Because the true critical perspective is uninfluenced observation and understanding of what is, as it is. That is clarity, and clarity condemns almost everything said or thought about mental health and our proper response to it. You might think this sounds intellectually arrogant, but it is not a set of intellectual conclusions at all. It is a patient observation and investigation of the facts of my own mind, people in my life, the field of psychiatry, and the world as a whole. That is not theoretical investigation but uncovering and discovering the facts. So I’ll risk sounding arrogant because we need to start talking about this in painfully honest terms, otherwise all our efforts in this field remain absolutely worthless, which sorry to say remains the case with articles like this. The most powerful work would be an exposition of the facts devoid of all opinion. Opinions are totally worthless because they are non-facts. The facts give a luminous and total picture if your perception of them isn’t distorted and destroyed by opinions and conclusions. That is the actual truth people.
Report comment
You are absolutely correct. Thank you. There are no redeeming factors, none.
Report comment
Thank you sir! I’m glad you agree. I hope you will make a noise too!
Report comment
“I’m afraid that even though Mad in America contains among the most critical intellectual perspectives on the field of psychiatry and psychiatric medicine, it has not swallowed, let alone digested, the important facts which all point to a picture of a totally fraudulent and harmful psychiatry, and a totally misguided, confused and impotent set of professions including all mental health worker and even critical psychiatrists and psychologists. Because the true critical perspective is uninfluenced observation and understanding of what is, as it is.”
Beautifully stated.
My observation tells me that there seems to be lots of people who never stop playing ‘Follow-the-leader”.
Report comment
“My observation tells me that there seems to be lots of people who never stop playing ‘Follow-the-leader”” – amen to that! I think we both agree often because people who are able to see what is as it is tend to agree. Unfortunately, you have to be on the wrong side of psychiatry to see psychiatry for what it is, but then when you see it for what it is you’re on th right side – i.e. our side, not these dumb psychiatrists and nice but impotent technocrats writing for Mad in America. Rather be a psychotic then a technocrat personally! 😀
Report comment
Me to! 🙂
I think you are absolutely right – you have to be on the wrong side of psychiatry to see it for what it is: on shaky ground!
Report comment
Please be also aware of many success stories and now real clinical trials using the medical ketogenic diet (developed 100 years ago for epilepsy) for those with serious mental illness. Info can be found on metabolicmind.org, https://www.chrispalmermd.com/
&
https://www.diagnosisdiet.com/
This is amazing news – we are trying it with our psychotic son.
Report comment
For anyone with psychosis, I would also look into orthomolecular treatment. It’s easy to learn, inexpensive, effective and proven over the last 80 years to restore one’s mental health. Please see my 3 videos on on YT about it at “Linda Van Zandt’s Mental Health Recovery Channel” for more info.
My loved one’s “incurable” “bipolar with psychosis” disappeared by using food supplements from our local health food store to lower his histamine level. Most psychotic patients need to raise their level but my relative was among the 20% whose level is too high. Many anti-psychotic drugs work by artificially lowering one’s level. I still wondered though what was causing his histamine level to go high in the first place and then someone introduced me to homeopathy. Homeopath, Elaine Lewis, who cured my son, has lots of articles on homeopathy at hpathy.com. I wrote “Goodbye, Quacks – Hello, Homeopathy!” about homeopathy and my family’s experiences with curing mental illness. BTW, the WHO says homeopathy is the second most widely practiced system of medicine in the world.
Report comment
Our psychotic son has been on the Wm Walsch orthomolecular protocol/ supplements for 9 months. High histamine, pyroles & high serum free copper with little but some symptom relief – still very psychotic. We are finally having some success getting him into ketosis – 3 days is longest stretch so far. Gives us hope as when he is in ketosis we see an immediate change – we have seen no improvement in psychosis 24/7 from any psycmed or supplement like we see with ketosis. We just need to learn better how to keep him from sabotaging the food parameter. We received advice from a psychiatrist currently doing a clinical trial in SF KETO for psychosis. Use the keyo-mojo to measure blood ketones & an experienced psychologist/keto coach. It’s not a “diet” it’s a metabolic medical intervention.
Report comment
Terri, is it possible your son’s histamine level is back down to normal now and that he no longer needs the supplements to lower it? One orthomolecular expert told me that once a person’s histamines are back down in the normal range, they need Dr. Hoffer’s treatment: mainly niacinamide, usually 1 gram three times a day with meals, plus one daily capsule of B Complex.
Also, is it possible your son might have contracted Toxoplasmosis? Most people catch it from a cat that has been sickened by a sick rat or some other critter outside.
The NIH says that 21% (1 out of 5 cases) of schizophrenia are actually misdiagnosed cases of Toxoplasmosis. It’s caused by protozoa that create cysts and when they grow in the brain they, of course, cause it to malfunction.
The NIH also says the plant extract, artemisinin, kills this protozoa.
My son was diagnosed with “bipolar with psychosis” which turned out to be Toxoplasmosis. (We had a sick cat at the time. The cat and I both developed heart disease.)
I hired a professional homeopath, Elaine Lewis, to help us. She figured out the right remedy (homeopathic medicine) and completely cured my son. That was 9 years ago. (I happened to take the right remedy to cure something else and it cured my heart.) Elaine is at hpathy.com. Hiring her was the best money I ever spent. She uses a questionnaire of about 70+ questions to figure out what remedy the person matches up with, all done through emails.
I know that what you’re going through is so difficult and I wish you all the best.
Report comment
Thank you, he does not have Toxoplasmosis and that explains how orthomolecular helped your son. My son is on the wm walsh protocol via mensah medical After 9 months histamine is still high. Their protocol stems from pfeiffer/hoffer – that was a LONG time ago. Research is now showing much mental illness is metabolic and can be helped , even sometimes put into remission by metabolic therapies. His illness is beyond the scope of orthomolecular but it has helped with some symptoms.
Report comment
Terri, Yes, orthomolecular medicine restored my son’s mental health but homeopathy is what finally cured him. I wonder, too, if he could have any elevated levels of toxic metals, e.g. copper, aluminum, mercury, cadmium, lead, etc.
Report comment
those safe and effective “vaccines” have aluminum in them…..considered a heavy metal and toxic when injected…
Report comment
We are overlooking the elephant in the room.
We don’t know the definition of psychosis; there is no real scientific definition of it. It is very difficult to treat something if you don’t even have the definition right. Most people who experience psychosis are dismissed, even when they are not psychotic. Only those people can tell you what psychosis is and what may heal or help them, if you respect them. We don’t respect them, so we will never know what psychosis actually is until we respect people when they are not in a psychotic state and actually include them in the solution.
That’s the elephant in the room.
This idea is not different from the architecture for disability. If you are designing a chair for a disabled person, you actually want to have the person you are designing for test the chair and part of the process. If you create a chair without the input of the person you are designing for, guess what? It’s not going to fit that person. Most disabled people overcompensate for the lack of and the oversight of those designing products for them without their input.
In short, without respectfully collaborating with those who have experienced psychosis in a meaningful way—not in hierarchical and power-structured ways—this type of talk is just “regurgitation”.
Report comment
Injecting someone with anti-psychotics sounds to me much like embalming a live human being.
Report comment
That would be correct but would dramatically reduce the rate of recidivism. No profit there. won’t happen, ain’t going to happen. Keep em alive, that is where the $$$$$ is.
Report comment
Yup. Kinda like “Night of the Living Dead”.
Report comment
This article, as the last of a three part series, was intended as more exploratory and suggestive, rather than critical. With the modest aim to stimulate further debate on how harm might be reduced, rather than to provide an exhaustive review.
Thanks to those sharing what they have found works for them.
I am aware of the Open Dialogue approach, even if I have not yet read much of the literature pertaining to it. It is though, clearly, an approach congruent with the type of psychosocial based treatment (minimal medication) models and trials I discuss. And Open Dialogue has historical roots in common with Loren Mosher’s Soteria.
Without attempting to theorize (and express opinions) a little we are unlikely to uncover any new ‘facts’.
Of course, whether, what are loosely called ‘psychotic states’, should always be considered as harmful or unwelcome is open to debate. But I didn’t choose to examine that wider question here.
Report comment
What are they overlooking? In my opinion, the two most important things: the person in front of them and the trauma that most likely brought on their psychosis, an important conversation that usually never happens.
Report comment
What is being overlooked? That when doctors prescribe antipsychotics, they are actually “treating” themselves.
Report comment
That does not seem to be working for them either.
Report comment
Humility is the only cure for what ails them.
Report comment
My Partner, who is 66 years old, was diagnosed with Parkinson’s disease last year. We noticed that he was experiencing hallucinations, slow movement, disturbed sleep, and twitchy hands and legs when at rest. He had to stop taking pramipexole (Sifrol), carbidopa/levodopa, and 2 mg of biperiden because of side effects. Our family doctor recommended a PD-5 treatment from natural herbs centre. com, which my husband has been undergoing for several months now. Exercise has been very beneficial. He has shown great improvement with the treatment thus far. He is more active now, does more, and feels less apathetic. He has more energy and can do more activities in a day than he did before. As far as tremors I observe a progress, he improved drastically. I thought I would share my husband’s story in case it could be helpful, but ultimately you have to figure out what works best for you. Salutations and well wishes
Report comment
Homeopathy has medicines for Parkinson’s. Western doctors claim it’s “incurable” but they said that about my psychotic loved one, too. He’s fine now because homeopathy cured him. Elaine Lewis has lots of good info over on hpathy.com. She’s the professional homeopath I hired who cured my loved one.
Report comment
What is being overlooked in matters of psychosis?
Fostering a meaningful connection with the person experiencing it.
Report comment
…. WITHOUT the following agenda: diagnoses, “therapy” or “medication” —
Report comment
We’re overlooking the fact that psychiatrists aren’t taught to even look for, let alone cure, the proven physical causes of psychosis. They have no clue how to do so. Try asking a psychiatrist about a cure—you’ll be laughed at. Why? Because they don’t know and they don’t want you asking about it. End of discussion.
There are many proven causes and cures for psychosis and other mental illnesses:
People following a vegan diet can become psychotic from a lack of B-12 because only animal foods contain this vitamin and it is critical for proper brain function.
The NIH says 21%, or 1 in 5 cases, of schizophrenia are misdiagnosed infections of Toxoplasmosis.
Decades ago, orthomolecular scientists identified the three extremely important, widespread, biochemical causes of about 95% of all cases of psychosis and also figured out which biochemicals restore these imbalances. (Please note: humans don’t have a “chemistry.” We can only have a “biochemistry” because we are living, biochemical beings.)
Nineteen years ago my “incurable” “bipolar with psychosis” loved one had a histamine level that was too high. Orthomolecular treatment lowered it back down to the normal range. Over a period of 4 mo’s I was able to taper him off 3 different, daily antipsychotic drugs while I also gave him the “nutraceuticals” that lower histamines. (I tried one myself and it made me irritable, most likely because I tend to already be a low-histamine person.)
I also know that homeopathic medicine cured my loved one 9 years ago and I use the word “cure” intentionally. Homeopathy cures. It cures gently, deeply and permanently. Homeopathy doesn’t go by the name of an illness. Homeopaths are taught to pay close attention to what their client’s unique symptoms are communicating. Homeopathy has hundreds, maybe thousands, of medicines to cure various causes of psychosis. The right homeopathic medicine made my relative’s psychosis disappear in about 10 minutes, although it came back a few times and he needed a few more doses.
The Am Psych Ass’n has been very effectively fighting the orthomolecular approach since about the 1950s and fighting against homeopathy since the 1800s. The APA is making so much money by claiming they are the experts on mental illness that they’re never going to admit their cover-up. What do they care that they cure no one or how many millions of lives are being destroyed daily by their sleazy, for-profit care? They’re not in business to make friends. They’re a corporation in business to make money. Psychiatrists are their pawns for bringing in the dough.
According to my congressman’s aide in Wash, DC and the Congressional Research Service, there’s no law saying the APA must even try to cure patients. The APA truly has 100% freedom to choose any approach they like. Is it any wonder they’ve chosen the one that brings them and their business buddies, the drug companies, the most profit? They then stick DSHS with the bill for these individuals’ lifetime needs for food, rent, utilities, medical care, psychiatric care and all the rest. And when I say “DSHS,” I mean your tax dollars and mine.
I began looking for the causes and cures for a loved one’s mental problems back in 1996 so I’ve learned a lot over these 28 years.
For more info on the ortho-m approach please see my 3 videos on YT at “Linda Van Zandt’s Mental Health Recovery Channel” and/or read “The Secrets to Real Mental Health” by Linda Van Zandt (my pen name). I’ve recently written “Goodbye, Quacks – Hello, Homeopathy!”, which, like my first book, is about what my family went through. It’s also a beginner’s guide to using homeopathy to cure mental (and physical) illnesses.
Lastly, FYI, I’m not trying to pass myself off as a “writer.” I’m not a writer—I taught high school. I consider both books to be more like (really long) letters to help others pull themselves out of the trap of conventional mental health “care.”
Report comment
Maybe the reason people doped up on antipsychotics often fare worse than those who aren’t is because taking antipsychotics makes feeling one’s feelings impossible.
Report comment
My Partner, who is 66 years old, was diagnosed with Parkinson’s disease last year. We noticed that he was experiencing hallucinations, slow movement, disturbed sleep, and twitchy hands and legs when at rest. He had to stop taking pramipexole (Sifrol), carbidopa/levodopa, and 2 mg of biperiden because of side effects. Our family doctor recommended a PD-5 treatment from natural herbs centre , which my husband has been undergoing for several months now. Exercise has been very beneficial. He has shown great improvement with the treatment thus far. He is more active now, does more, and feels less apathetic. He has more energy and can do more activities in a day than he did before. As far as tremors I observe a progress, he improved drastically. I thought I would share my husband’s story in case it could be helpful, but ultimately you have to figure out what works best for you. Salutations and well wishes
Report comment
What are we overlooking? That people need inspiration, not “medication”.
Report comment
What we’re overlooking is that mental illnesses are curable, just not with man-made chemicals. To cure an illness we have to know what’s causing it. An elevated level of copper may be to blame, or Toxoplasmosis, or a histamine level that is too high or too low. It could be something that matches up with a homeopathic medicine. It could be due to a severe trauma or head injury (which homeopathy also has medicines to cure).
No matter what the physical cause, the APA has carte blanche to ignore it and only prescribe whatever patented chemicals bring them the most profit. The APA is 100% free to cover up the research which has proven the physical causes of schizophrenia, psychosis, anxiety disorder, depression and all the rest. Sadly, the US government backs them all the way by not having a law saying psychiatrists must even TRY to cure anyone. All we have is a giant, gaping loophole where a law should be. And this is exactly how the APA wants the American mental health care system to remain. It’s sad how many millions of Americans (myself included in the distant past) have fallen for their scam.
Report comment
In my experience, histamine is activated by the nervous system alone. It took me a long time to understand that even calm states – reading a book – can activate histamine. So it’s not just the highly active nervous system, e.g. by re-experiencing trauma, but also the very calm ones. I call them hypnagogic states. I could imagine that it is precisely these states of consciousness that lead to “psychotic states”. It’s all a question of the nervous system and, above all, the state of consciousness.
So I have learned to minimize calm states and integrate them very consciously into my life. Sometimes I set myself an alarm clock to remind myself that I need to get moving again. I have learned that a change of state of consciousness is always necessary.
Wilhelm Reich observed that his predominantly female patients developed urticaria while lying on the couch in psychoanalysis. These women were also in trance states in which they reacted extremely strongly.
Today, doctors claim that certain foods increase histamine levels. No, the nervous system does it. However, it can be reduced by a diet, especially without eating sugar.
Antihistamines are old drugs. Psychotropic drugs were developed from them. So the mechanism of effect is the same, or similar.
Thank you for the reference to orthomolecular medicine. I will deal with Dr. Carl Pfeiffer and go deeper into this subject.
Report comment
Histamine is activated by many things…stress, spikes in blood sugar, inflammation (because inflammatory mast cells release histamine), and it’s higher at night
“hypnagogic states”…as in sleep paralysis…interesting.
I think that histamine is going to end up being a critical player in the pathology of depression.
“spikes in brain histamine following stress likely drive neurochemical changes in monoaminergic systems. Indeed, elevated histamine can result in increased activation of H3 heteroreceptors on 5HT terminals in the hippocampus, resulting in blunting of neuronal serotonin release and producing a reduction in extracellular serotonin.”
Report comment
Thank you, Silvia Price, your answer has given me once again new insights.
Biochemically I am not so fit. So far I have distinguished between mastocytosis and MCAD. As far as I know, in mastocytosis the mast cells are multiplied, and in MCAD they release more messenger substances, which then trigger the inflammation. In my case a DNA test at a university medical centre ruled out mastocytosis. I was not told that the mast cells themselves are inflamed in both cases. Unfortunately doctors, even in the research field, know very little about histamine. They only test Tryptase and treat the symptoms with antihistamines.
Very interesting what you write about the “hypnagogic state” I mentioned. Until now I didn’t know that histamine is elevated at night. I didn’t read and wasn’t told about this fact but it explains a lot to me. I have been suffering from “sleep paralysis” for years; very rarely, but it started years ago in a stress situation. Years later the histamine problem startet. This is a very important information for me. Now I also understand why I wake up at 4 a.m. and could stand up and dance without any cardial problems.
When I fall asleep again – often I don’t sleep anymore – the “hypnagogic state” goes on. Sometimes I dream very intensely, very realistically, as if I was watching a movie, and sometimes the pictures are quite frighteningly, and I remember these dreams very well.
So I have the idea, when this state takes more and more place in the waking consciousness, or breaks through at any time – two states of consciousness at the same time – they call it „psychosis“. From spiritual people I know, they are in more than two states at the same time. Perhaps the question ist what triggers the states? In one case it may be training, in the other wrong running neurotransmitters???
Yesterday there was the film „Everything Everywhere All at Once“ from 2023 on TV. In 2023 this film won a lot of Oscars and the title says all about our consciousness.
Now I will go on researching.
Report comment
Liberationfrom drugs: you seem to have lots of experience with histamines. My family does, too, because at least 2 of us (the 2 tallest ones) have an elevated level and both tend to suffer from depression.
The NIH estimates that something like up to 50% of the population is infected with Toxoplasmosis gondii, and may, or may not, show symptoms. It is an infection of protozoa, “cousins” to the protozoa that cause malaria.
The NIH specifically says 21% of all cases of schizophrenia are misdiagnosed cases of T. gondii. Coincidently, Dr. Pfeiffer found decades ago that approx 20% of all cases of schizophrenia are due to an elevated level of histamine. So I’ve been wondering if these statistics match up. That is, I wonder if T. gondii might be the underlying cause of Dr. Pfeiffer’s 20%. Just wondering, of course. I’m not a scientist and maybe I’m making a connection where there is none.
The NIH further states that the plant extract, artemisinin, kills these protozoa. I bought some and took a capsule (500 mg). It caused such insomnia that lasted for two nights. I continued experimenting and took a third of a capsule next. It did nothing. I’ll probably take half a capsule one of these days to see what it does.
I think it’s criminal that psychiatrists don’t do a trial of artemisinin on all their psychotic patients in order to find the 21% who can be cured. Instead, patients are kept as lifelong customers of psychiatric goods (drugs) and services (talk therapy) until they die.
Report comment
Conditions like schizophrenia have high rates of MTHFR C677T homozygous mutations, which cause low Folic Acid and malaria and T.Gondii harvest Folic Acid from serum and neural cells. So infection is higher in people who have sufficient Folic Acid.
“I think it’s criminal that psychiatrists don’t do a trial of artemisinin on all their psychotic patients in order to find the 21% who can be cured”
According to the literature about 12% of Caucasians, 22% Hispanics have MTHFR C677T homozygous mutations and it may be higher in schizophrenia. Since they cause low Folate, using anti folate meds like the ones used for malaria would not be recommended.
High histamine/histamine intolerance and depression can also be caused by the same mutations.
Report comment
“If long-term reliance on treatment with neuroleptic drugs appears increasingly unjustifiable, what can be said about their use in the first instance?”
That it’s stupid to use them in people who have MTHFR homozygous mutations since they lower Folate, Vitamin D and Vit B12 and increase homocysteine and histamine…..all the things they already have.
Report comment
Oh yes the NIH. I think I am correct in saying that they received over 400 million dollars in patent rewards in a two year period beginning with the shots… the ones they say protect us for an invisible, deadly end to our lives…trust them for sure.
Report comment
liberationfromdrugs,
Re: sleep paralysis…I think it’s disordered sleep. For me it happens when I’m sleep deprived and fall asleep quickly (same thing happens in narcolepsy). So I try not to fall asleep too quickly.
The female patients who developed urticaria while lying on the couch in psychoanalysis is a good example of histamine intolerance. Once you get to a certain level without being able to get rid of it, increasing it causes symptoms, rash, hives, etc (For hives outbreaks I use Luteolin from Algonot)
According to Dr Walsh (who used to work with Dr Pfeiffer) hypomethylators have high histamine and overmethylators have low histamine. New research has shown methylation abnormalities in the different psych conditions (including schizophrenia, depression, autism, ADHD, PTSD, Bipolar disorder and Alzheimers) and it’s linked to MTHFR C677T homozygous mutations.
“Accumulating evidence suggests altered 1-carbon metabolism in the pathophysiology of these psychiatric disorders, since folate and vitamin B12—which are essential cofactors of enzymes involved in Homocysteine methylation to methionine—are found to be deficient in these patients.”
https://journals.sagepub.com/doi/pdf/10.1177/2326409817701471
A new study found that in 186 psych patients, 77 had normal MTHFR enzyme function, 85 had moderate deficiency and 24 had severe deficiency. The ones with severe deficiency were more resistant to treatment.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC11088868/?fbclid=IwZXh0bgNhZW0CMTEAAR1kZ6YZ5njlMvarOZKUhQ_kLPe6ami_eO1jUYpUPQ1nmx0yD8bFNLaefoE_aem_pNO8tWnPVhsJHlp_wZrhbg
In people positive for MTHFR C677T homozygous mutations, studies have shown the insomnia is caused by high homocysteine.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8974368/?fbclid=IwZXh0bgNhZW0CMTEAAR2DGy7of_rlgwpeZEEE6sdYxtfHCkl5JoQ__ew-Ju8EOOKIV86xIaaRUDA_aem_gg7HjqHUfMagCD8oca7oVQ#:~:text=Biochemical%20functionality%20of%20MTHFR.,human%20diseases%20such%20as%20insomnia
Report comment
Abram Hoffer, MD and Carl Pfeiffer, MD are considered the two founders of “orthomolecular medicine” which had its beginning in about the 1940s. Dr. Hoffer treated thousands of his patients with vitamin B-3 while Dr. Pfeiffer treated thousands by measuring their histamine level.
Both used a urine test for “pryoluria,” too, a common cause of mental illness, although eventually they didn’t even need to test. They had other markers to determine if a patient had pyroluria.
Hoffer’s B-3 worked wonders for one of my children. When my other child became psychotic and was put on 3 daily, antipsychotic drugs, I took him to see Dr. Hoffer in person. Unfortunately, his B-3 treatment did nothing for him.
I read Dr. Pfeiffer’s books and had my son’s histamine level tested. It was much too high so l lowered it and was able to slowly taper him completely off all 3 antipsychotic drugs that were destroying his quality of life. I wrote “The Secrets to Real Mental Health” about using orthomolecular medicine so others could avoid what we went through. I also have 3 YouTube videos, a beginner’s guide to orthomolecular treatment at “Linda Van Zandt’s Mental Health Recovery Channel.”
Still, I wondered what was causing my children’s need for either B-3 or histamine-lowering in the first place. I learned from reading the work of (the late) researcher, Lida Mattman, PhD that it isn’t really our genes, it’s the mutations to our genes. So what causes the mutations?
Dr. Mattman discovered that when someone is treated with (high-dose, short-term) antibiotics for diseases such as syphilis, Lyme Disease, etc, not all the bacteria are killed. The surviving bugs know how to hide. They wait until it’s safe to come out again but now they have “pleomorphed” (changed) into the incredibly tiny form of bacteria, Cell-Wall-Deficient bacteria. Mattman proved that’s what causes “Post Lyme Disease Treatment Syndrome.” Being as small as, or even smaller than, the cells of a virus, CWD bacteria infect wherever they choose. Then conventional doctors label the resulting symptoms as “autoimmune.”
In reality, our immune system isn’t stupid. It isn’t attacking its own body—it’s attacking the CWD bacteria hidden in those tissues.
Without the aid of modern science, Dr. Hahnemann, discoverer of homeopathy 200 years ago, figured this out himself. He learned that when diseases are treated with chemicals, they turn into a “miasm” or a “dyscrasia” that is typically passed from mother to baby, generation after generation.
Being a layperson, not a scientist, I can’t tell the difference between Dr. Hahnemann’s miasms and Dr. Mattman’s CWD bacteria. Either way, the only treatment I’ve found to cure these inherited diseases is homeopathy.
We have numerous miasms (or CWD bacteria) in my family but we’re curing them with homeopathy.
For a beginner’s guide to homeopathy with a focus on curing mental illnesses, please read my book, “Goodbye, Quacks – Hello, Homeopathy!” I gave it that name because, in my view, conventional psychiatry is nothing but quackery. That’s why it cures no one.
Report comment
I watched your videos. Let’s see if I can help you understand a few things.
What causes the mutations?
The MTHFR gene helps metabolize Folic Acid. Mutations are small variations. You inherit one copy of the gene from your mother and one from your father. If you inherit one mutation from your mother but your father doesn’t have any then you will end up with one mutation. That’s no big deal because that lowers MTHFR enzyme efficacy just a little. But if you inherit one mutation from your mother and one from your father and both are type C677T that lowers MTHFR enzyme efficacy to 25%. So you won’t be able to metabolize Folic Acid correctly (it also causes low Vit B12 and VitD).
That’s important because you need Folic Acid and Vitamin B12 to be able to recycle homocysteine to methionine and be able to make SAMe. SAMe is super important because it donates methyl groups to aid important processes like the manufacture of neurotransmitters and histamine metabolism (you need SAMe to methylate histamine). Plus, you need Vit B to make DAO, the enzyme that breaks down histamine.
Obviously, hypo and hypermethylators are treated differently. Watch some of Dr Walsh’s videos to see how he treats them as well as pyrrole .
Re bacterial and viral infections
TLRs (Toll-Like Receptors) are transmembrane proteins expressed by cells of the innate immune system. They recognize common structures on pathogens, known as pathogen associated molecular patterns (PAMPs), and activate signaling pathways that launch immune and inflammatory responses to destroy the invaders.
“Cell-Wall-Deficient bacteria”
Bacterial products, otherwise called Lipopolysaccharide, are large molecules consisting of a lipid and a polysaccharide found on the outer membrane of gram negative bacteria. When they reach the liver, they act as endotoxin and elicit a strong reaction from our immune system.
There is a fine line between “protection from TLRs” and “damage from TLRs”. TLR signaling induces the production of inflammatory mediators and anti-microbial peptides to eradicate invading microorganisms from the host as well as to bridge the acquired immunity to amplify immune responses. However, abnormal activation of innate immune signaling may also cause chronic inflammation, tissue and organ injuries, fibrosis, carcinogenesis and autoimmune diseases….but I certainly wouldn’t call them symptoms.
I checked out hpathy.com. Here’s what it says about one of the treatments they use….
“breath, saliva, urine, stool, etc is often heated with water for detoxification in the autopathic bottle, then diluted and applied on the skin at the forehead between the eyes”
In other words, they’re applying “Cell-Wall-Deficient bacteria” to their faces. So quacks are everywhere and so are people who believe them.
Report comment
We’re here to try to find answers to the puzzle of mental illness for the purpose of helping people. We’re not here to try to shoot down other people’s perspectives or call people names so be an adult: take from this forum what works for you and leave the rest.
For 200 years, those who don’t want homeopathy to work, denigrate it and try to make it seem “unscientific.” To repeat, the WHO has found homeopathy to be the second most widely used system of medicine in the world—because it works, whether most people understand how it works or not. I don’t know where the previous poster found her info on homeopathy but be aware, it’s nothing like any homeopathy I’ve ever heard of or used. Maybe someone has found some weird way of using this wonderful medicine, I don’t know. All I can tell you about it is that whatever she’s citing is bizarre and far from mainstream homeopathy.
I personally know of three people cured of ADHD, “bipolar with psychosis,” and schizophrenia all cured by homeopathy. At least two had Toxoplasmosis, a very common infection that psychiatrists have no clue how to cure even though the NIH says artemisinin kills the microorganisms that cause this dreadful disease. So if you’re looking for real answers to your or your loved one’s mental illness, don’t be afraid to consider homeopathy (or Ayurveda, or TCM, or acupuncture, etc).
In contrast to homeopathy which has been curing people for 200 years, any medicine, specifically man-made drugs designed to cure no one, is quackery.
Report comment
Linda,
The quote on my previous post came from hpathy.com the site you recommended, from an interview with homeopath Ellen V. Kire July 2024. Here’s the link….
https://hpathy.com/homeopathy-interviews/homeopath-ellen-v-kire-is-interviewed-by-alan-v-schmukler/
Report comment
It wasn’t meant to be an insult. More like a warning to be careful. An independent researcher attempted improving methylation in Chronic Fatigue Syndrome patients with a protocol that included Vitamin B and Folic Acid + Methyl Folate and some of the patients ended up with serious autoimmune conditions.
I’m glad you were able to save your son. I couldn’t save mine. I knew a lot but not enough. I knew about MTHFR mutations but I didn’t know I had them.
Report comment
Great article, thank you for bringing attention to this extremely important matter.
Several things came to mind while reading this article.
First, I think we need to ponder what “psychosis” actually is, albeit with the understanding that it will continue to be a work in progress for many years to come.
But I bring this up because too often treatments are based on the standard definitions of psychosis; definitions that (essentially speaking) have been contrived by the very entities that we are trying to combat (ie: Big Pharma).
Calling symptoms “psychosis” brings an entire schematic along with it that might be leading far more people astray, rather than helping them focus on the matter at hand.
(I will be illustrating some examples of this in the numbered items that follow.)
Let’s say someone is presenting with symptoms that current therapeutic and psychiatric frameworks would identify as “psychosis”.
1. A comprehensive food allergy panel (lab work) can be ordered that looks for biomarkers (such as food specific antibodies). In my experience, an astounding amount of people (and this can probably be inductively extrapolated to just about everyone) are eating foods that their immune systems are producing abnormal amounts of antibodies against.
Food allergies tend to be assessed in an all-or-nothing format, where either the patient is presenting with a very noticeable reaction that is temporally associated with a food they ate, or if nothing strikingly noticeable can be temporally associated with foods they eat, food allergies don’t enter into the conversation.
To clarify, I speaking about situations beyond the typical eating healthier foods can alleviate symptoms. While they certainly can, what I’m highlighting is that we can go far beyond that with assessing just how one’s diet is effecting their health, including psychological health.
Quick example: I am highly sensitive to soy, but had no clue about it until I myself had a comprehensive food allergy workup done. Afterwards, I eliminated soy from my diet and the results (decreased anxiety) were very noticeable.
The only catch is that this bloodwork isn’t covered by most insurances and is quite expensive. But if this could be progressively implemented in standards of care, I believe this could be a paradigm shift in the way psychological issues are screened, and treated. The ultimate implication being that perhaps emotional difficulties are far more physical-based (I’m not referring to neurochemical “imbalance” though) than currently thought.
2. Eliminating microplastics as much as possible, and switching to filtered tap water (preferably reverse osmosis filtration). The water purity guidelines haven’t been updated in almost 20 years, and current research (as noted by EWG) shows that even municipalities that meet EPA standards contain dangerously high amounts of toxic and carcinogenic compounds.
3. For people who suffer from varying degrees of delusional thinking, disorganized, or paranoid thoughts, I believe that a percentage of them can be helped by being taught basic formal logic.
I’ve seen too many patients told that what they are thinking/saying is “wrong”, “doesn’t make sense”, or they’re just told that what they said is a symptom of illness. But perhaps if they (of course this doesn’t apply to all patients) were taught how basic formal logic works then they can begin to work through on their own as to why what they are saying is illogical. I think it’s condescending, and often simply inaccurate, when practitioners work with irrational/illogical thoughts as if they are “matching game”. Meaning that patients are often essentially told that the best they can do is remember that certain things they think about are symptoms of an illness, and that they shouldn’t say those things because people around them will interpret them as bizarre, making it hard for the patient to integrate into society. … I think most patients are far more capable of learning sound reasoning/logic than they’re afforded the opportunity to.
4. As mentioned in this article, I think supplements are seriously underutilized, and have a far greater safety and efficacy profile than their pharmaceutical counterparts.
Lion’s Mane, Bacopa, Chaga, Cordyceps, Agarikon, Reishi, Lemon Balm, Stinging Nettle, Coffee Fruit Extract, Ginko Biloba, NAC, high-dose vitamin C, glutathione, vitamin D, vitamin B complex, CoQ10, MCT, Omega 3, Alpha Lipoic Acid, probiotics (especially bifidum strains), magnesium, and many others.
I also highly recommend that patients be guided towards liposomal delivery forms of all supplements when the option is available.
Report comment