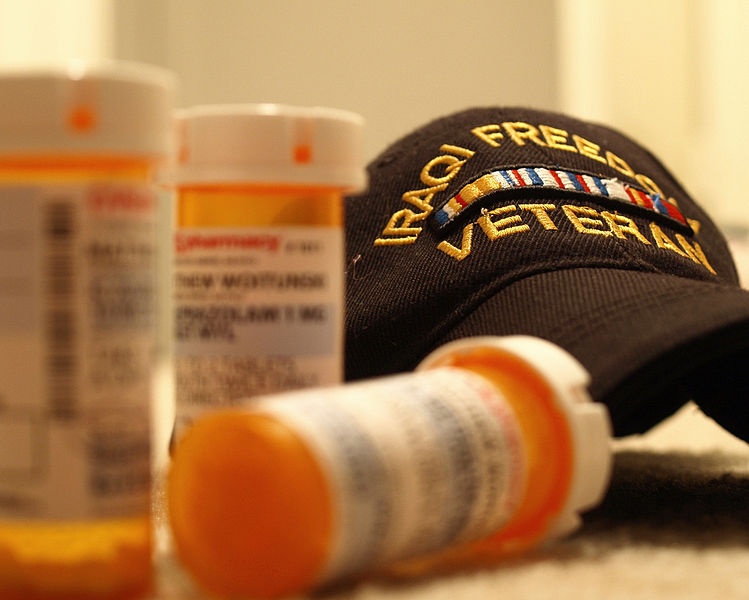
A new study, published in Psychiatric Services, investigates the quality of inpatient psychiatric care. The results of the cross-sectional study show that U.S. Department of Veterans Affairs (VA) owned hospitals perform worst on most measures.
“The apparent failure of the VA hospitals to screen for trauma—as well as substance use, violence risk, and patients’ strengths—warrants deeper investigation and potentially regulatory attention,” write the authors. The research was conducted by Morgan Shields, a doctoral student at Brandeis University, and her former professor at the Harvard T.H. Chan School of Public Health, Dr. Meredith Rosenthal.
Although there is a push for more access to mental health care services, there is little research evaluating the quality of psychiatric inpatient units and significant concerns have been raised about current standards of care. In 2008, the Hospital-Based Inpatient Psychiatric Services (HBIPS) measure set was developed to assess psychiatric inpatient care in seven domains. These domains include screening upon admission, use of physical restraint or seclusion, prevalence of and justification for discharging patients on multiple antipsychotics, and creating and communicating continuing care plans at discharge.
In the first study to evaluate HBIPS measures, the researchers analyzed data from 665 psychiatric inpatient facilities in order to better understand psychiatric facility performance. They also examined differences in performance quality based on hospital ownership (e.g., for profit v. non-profit, VA v. other government).
For-profit and non-profit hospitals performed best in admission screening and rates of restraint and seclusion. For-profit hospitals also performed best in creating a continuing care plan upon discharge and communicating the plan to future care providers. VA hospitals performed worst on all measures except for rates of restraint and discharging with prescriptions for multiple antipsychotics, which were worst at non-VA government hospitals.
“Overall, facilities performed the best on admission screening and the worst on appropriately justifying the practice of discharging patients on multiple antipsychotics,” write the authors. The researchers also highlight that, although for-profit hospitals had the highest performance on most of the measures, all hospitals had areas that need to be improved.
The researchers also found weak relationships between HBIPS measures. They conclude that either inpatient psychiatric care quality is multidimensional, or the HBIPS measures are not reliable. The authors argue, “Despite the variability both within and between measures, it is clear that hospital ownership matters when it comes to quality of performance on all of the measures. In particular, the data provide reason for concern about the performance of VA hospitals as well as other government hospitals.”
Methods for measuring and reporting inpatient psychiatric care quality are in the early stages, and a lot of work still needs to be done to validate current measures. The authors also note that the lack of “gold standards” for the measures, such as how to conduct admission screening and criteria for when restraint or seclusion are utilized, makes it difficult to implement quality improvement on a large scale.
The researchers explain that variation in hospital performance may be a consequence of different resources, and note that VAs may suffer from lack of funding. As the number of HBIPS measures is expected to reach 16 by 2017, the researchers call for new measures that capture patients’ experiences. The authors close by stating, “These data are critically important not only to foster accountability but also to improve our understanding of the mechanisms that support high-quality inpatient care and optimal outcomes for an especially vulnerable patient population.”
****
Shields, M. C., & Rosenthal, M. B. (2016). Quality of inpatient psychiatric care at VA, other government, nonprofit, and for-profit hospitals: A comparison. Psychiatric Services. Advance online publication. doi: 10.1176/appi.ps.201600074 (Abstract)















Thank you
Shannon for finding this so relevant and highly on target research information
So lucky you never had to experience this yourself!
Report comment
That the VA hospitals perform the worst does not surprise me.
But I also find it outrageous that people come back from wars and are told that they need psychiatry or psychotherapy, and that these could be the solutions to their problems.
These people have served in areas where things happen which are not talked about here at home, like friendly fire casualties and fragging, and like atrocities committed against combatants and civilians. Those who go off to war often have been fed a very distorted version of reality, and often a lack of other economic opportunities plays into it.
So then to return, living in the gap between reality and the lies and illusions our society lives on, to be told that they need psychiatry or psychotherapy is just another abuse.
Thou Shalt Not Kill
https://www.youtube.com/watch?v=aBADjCeFnuU
Nomadic
Move From Talk to Action, Please Join:
http://freedomtoexpress.freeforums.org/fighting-to-eradicate-the-mental-health-system-and-incarcerate-the-practitioners-f2.html
Report comment