A recent article published in the journal Psychosis sought to understand how people’s sense of self is affected after the experience of first episode of psychosis. The qualitative study results shed light on the possibility for post-traumatic growth, highlight the limits of current explanatory frameworks for psychosis, and point to treatment approaches that support recovery.
“Psychosis can affect identity in fundamental ways,” Phoebe Friesen, the lead author of the study and a professor of Biomedical Ethics at McGill University, points out. “Increasingly, those experiencing psychosis for the first time are enrolled in early intervention services. We sought to explore how individuals enrolled in such services felt their identity was impacted by their experience of psychosis.”
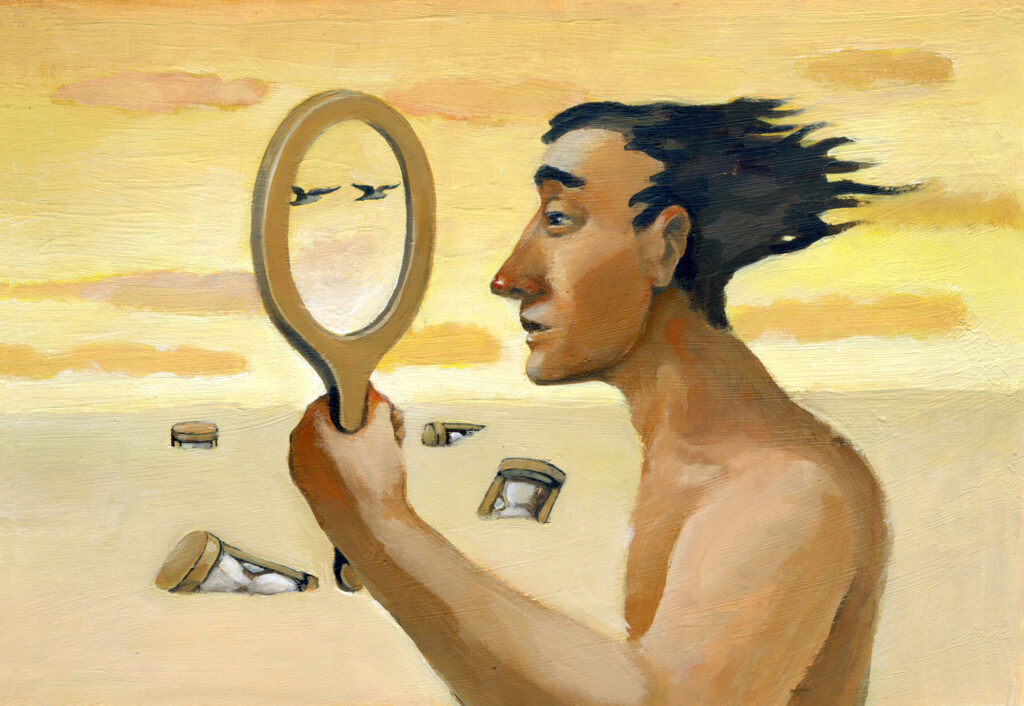 How does someone’s identity change during and after the experience of psychosis? Can you still be yourself after experiencing psychosis? The relationship between identity and the experience of psychosis raises philosophical questions with real-world implications for clinical practice and mental health treatment.
How does someone’s identity change during and after the experience of psychosis? Can you still be yourself after experiencing psychosis? The relationship between identity and the experience of psychosis raises philosophical questions with real-world implications for clinical practice and mental health treatment.
Early intervention services such as first-episode treatments for psychosis and approaches to people at clinical high-risk for psychosis offer specialty care for people experiencing psychosis and psychosis symptoms for the first time. These services are receiving more recognition and often focus on personal goals, recovery, and maintaining the roles people play either in their family, at school, or work. Although there are many different understandings of the cause of psychosis, exploring identity with people who experience psychosis is often essential for the treatment.
“The link between identity and psychosis may be particularly pronounced during experiences of first-episode of psychosis,” the authors note. “While most research examining the link between psychosis and identity has focused on individuals with a long-term diagnosis of schizophrenia, a few studies have investigated the experiences of those enrolled in an early intervention service.”
“As we shift away from a system of care in which diagnosis of schizophrenia is received as ‘a prognosis of doom’ and towards one in which those who have experienced psychosis are encouraged to continue setting goals and engaging in personally meaning activities, the identities of those enrolled in early intervention services are likely to be significantly impacted.”
As people’s sense of self is often affected by the experience of psychosis, how people’s identities change and how they make sense of these changes need to be studied. One way to understand the differences in identity following first-episode psychosis is through the concept of post-traumatic growth.
Post-traumatic growth is characterized by persons making positive changes following an experience of trauma or significant tragedy. Through post-traumatic growth, people may gain new insights about themselves, view their lives differently, develop new values, and adapt new coping strategies for better living.
The authors highlight two common responses to the changes people experience after an episode of psychosis: integrating and sealing over. People who adopt an integration approach tend to believe their psychotic experiences are meaningful and try to understand how their experiences fit into their lives. Conversely, people who adopt the seal-over style tend to put their psychotic experiences behind them so they can return to their previous life.
Although some studies suggested that the integration style of recovery has more positive outcomes in terms of their symptoms and quality of life than the seal-over style, more studies are needed.
To contribute to this growing body of literature, the researchers conducted in-depth interviews with several individuals enrolled at the early intervention services in New York City “to better understand how their identities were affected by their experiences of psychosis.”
The researchers conducted semi-structured interviews with ten racially diverse people enrolled in early intervention services for at least six months. They were asked about their experience of psychosis, identity, and wellbeing.
There were four themes identified from the analysis: (1) identity during and after psychosis, (2) psychosis and meaning, (3) reconciling experiences with explanations, and (4) positive changes to identity following psychosis. Each theme also included four sub-themes (underlined below).
Based on these themes, the study further discussed people’s recovery styles, explanatory frameworks, and post-traumatic growth.
For the theme “identity during and after psychosis,” many participants reported having a different identity during psychosis but some reported continuity of identity during psychosis. One participant felt they had to hide who they were while experiencing psychosis. In addition, many participants mentioned that part of themselves was missing following psychosis.
For the theme “psychosis and meaning,” as expected, participants responded either by characterizing their psychosis as meaningful or their psychosis as meaningless. Many believed that they had gained further self-understanding, while some were still struggling to understand experiences of psychosis. The authors explain:
“Some participants described psychosis as ‘crucial’ to their self-understanding or as helping them recognize a trauma they’d been carrying with them for a long time. Others described psychosis as a time in which ‘I left myself, and then I came back’ or as something that ‘postponed’ their identity, but that hadn’t changed them. These differences are similar to the distinction between integrating and sealing over.”
However, as that the experiences of psychosis are often complex, the authors suggested a mixed-recovery style, combining both integrating and sealing over styles. In addition, the principal author proposed the use of personal narratives and the development of a personally meaningful explanation for one’s experience for the recovery from the first episode of psychosis.
For the theme “reconciling experiences with explanation,” participants had a variety of responses. For example, some participants questioned whether they had experienced psychosis, some appreciated the medical explanation of psychosis, and some negotiated their own understanding of psychosis between their experiences and the explanations offered to them. Moreover, some participants emphasized that the diagnosis of psychosis did not define them.
“Many used multiple explanatory frameworks to understand their experiences, describing psychosis as ‘a chemical reaction in my brain’ but also ‘crucial’ to their self-understanding,” the authors write. “Participants also engaged in bricolage, utilizing a variety of explanatory frameworks, such as biomedical, spiritual, and psychosocial frameworks, to describe and understand their experiences of psychosis.”
For the theme “positive changes to identity after psychosis,” many participants endorsed positive changes to their identity, such as greater maturity, more empathy and compassion, and a greater sense of appreciation. In addition, some reported new goals and priorities in life.
“One particularly pronounced finding was the frequency with which participants reported positive changes to their identity following psychosis. This aligns with a growing body of literature documenting how people who have experienced psychosis see it as an opportunity to change and improve their lives as well as the experience of post-traumatic growth in the context of recovery from first-episode of psychosis.”
The authors conclude:
“Interviews with individuals enrolled in an early intervention service revealed that participants’ identities were impacted by their experiences of psychosis in a variety of ways… Some participants appeared to take on recovery styles of both integrating and sealing-over in response to their experience of psychosis, while most participants’ reports were suggestive of post-traumatic growth.”
****
Friesen, P., Goldstein, J., & Dixon, L. (2021). A “blip in the road”: experiences of identity after a first episode of psychosis. Psychosis, 1-11. (Link)















I agree, “Navigating the Meaning of Psychosis [is] Important for Recovery.”
My psychiatrist, who’d created “psychosis,” via anticholinergic toxidrome, insisted me and my psychosis were “w/o work, content, and talent” and “irrelevant to reality,” in his medical records.
But since my anticholinergic toxidrome induced “psychosis” was an insane story about a couple who’d raped my three year old child, and their pastor, claiming they were “God, the Holy Spirit, and Jesus.” It wasn’t difficult for me to agree with my psychiatrist, that I should dismiss the stupidity of his anticholinergic toxidrome induced “psychosis.”
But once the medical evidence of the rape of my very young child was handed over. Well, that made it very easy for me to leave my satanic, child abuse covering up psychiatrist. And become a psychopharmacological researcher, so I could find the etiology of how my psychiatrist had made me “psychotic.”
I generally agree,”Navigating the Meaning of Psychosis [is] Important for Recovery.” But, in general, especially when the etiology of a person’s “psychosis” is dismissed, denied, and ignored. I do think finding the etiology of a person’s “psychosis,” is more important for recovery. And, finding the meaning of one’s psychosis is not that difficult, once one is handed over, and picks up their medical records, and does their medical research.
But maybe the head of family medicine – at one of the most well respected hospitals in the country – was correct? When he stated that my research into the psychiatric crimes against me, and humanity – of systemically creating “psychosis” via anticholinergic toxidrome – was the research finding of a “one in a million” medical researcher.
Irregardless, let’s hope and pray the “mental health” industries get out of the business of systemically anticholinergic toxidrome poisoning people, to make them psychotic, with the antidepressants and antipsychotics.
https://en.wikipedia.org/wiki/Toxidrome
Report comment