Researchers have suggested that machine learning—using artificial intelligence to investigate a complex phenomenon—might be better at identifying which neurobiological measures are important and how to use them to predict psychiatric diagnoses. Unfortunately, so far, these attempts have landed with an accuracy little better than pure chance.
However, much previous research has used a single type of neurobiological measure (such as one type of brain scan) to try to predict psychiatric diagnoses.
In a new study, researchers tried something different. They created a machine learning algorithm to combine every conceivable neurobiological measure in order to predict depression.
But their results were just as underwhelming:
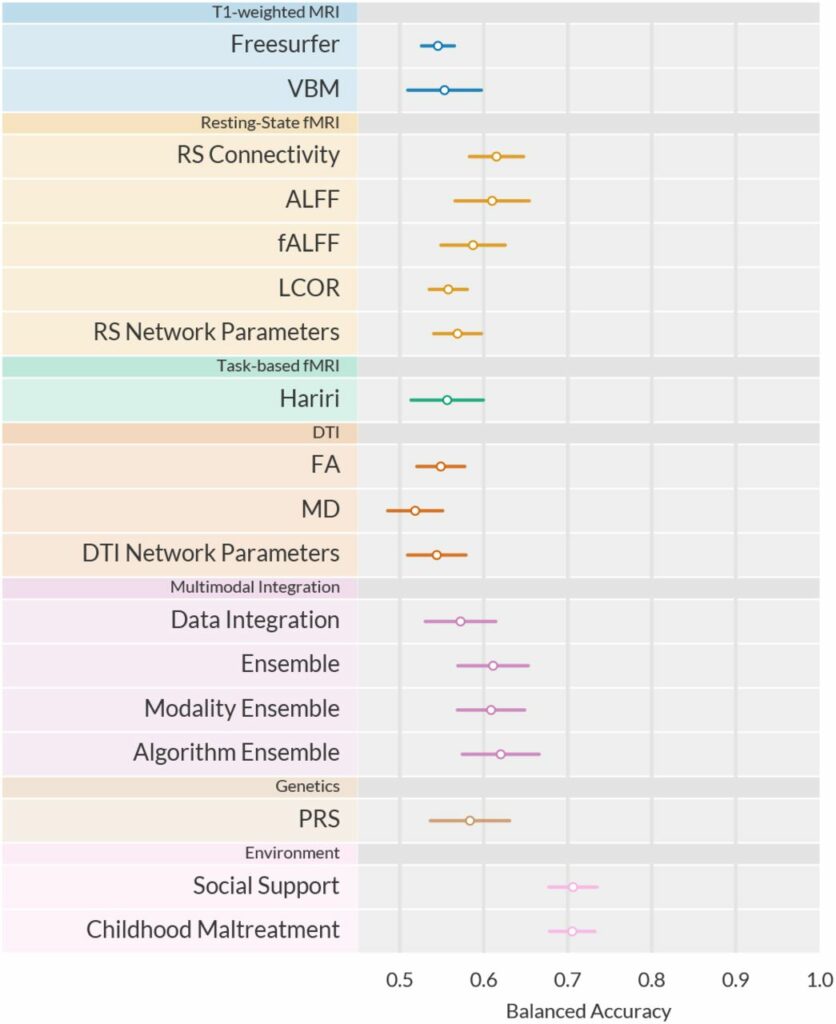
“Training and testing a total of 2.4 million ML models, we find accuracies for diagnostic classification between 48.1% and 62.0%,” they write.
For comparison, they note that the social/environmental variables of social support and childhood maltreatment each predict depression with greater than 70% accuracy. Combining social/environmental variables and including more than just those two might bring accuracy even higher.
In sum, they write, “Although multivariate neuroimaging markers increase predictive power compared to univariate analyses, single-subject classification—even under conditions of extensive, best-practice Machine Learning optimization in a large, harmonized sample of patients diagnosed using state-of-the-art clinical assessments—does not reach clinically relevant performance.”
The research was led by Nils R. Winter at the University of Münster, Germany. The article was uploaded before peer review to the preprint server medRxiv.org. On Twitter, Winter wrote about the study:
“The fact that we cannot find meaningful (univariate or multivariate) neurobiological differences on the level of the individual for one of the most prevalent mental disorders should give us pause.”
The previous study by this group resulted in a similar outcome. The researchers found that there were no individual-level differences in neurobiology between people with depression diagnoses and healthy controls.
In that study, the researchers wrote that “healthy and depressive participants are remarkably similar on the group level and virtually indistinguishable on the single-subject level across a comprehensive set of neuroimaging modalities.”
 A Deeper Look at the Current Study
A Deeper Look at the Current Study
The current study by Winter’s group included 1,801 people from three groups: those who currently met the criteria for the depression diagnosis, those who had a history of depression, and healthy controls. They were recruited through the Marburg-Münster Affective Disorders Cohort Study (MACS) in Germany.
Previous studies have raised concerns about the reliability of diagnosis since patients listed as “depressed” are often defined based on screening questionnaires or other less reliable measures. The current study used the clinical standard of a DSM-IV Structured Clinical Interview to diagnose depression, ensuring that the diagnosis was as reliable as possible.
The neurobiological measures included various forms of structural, functional, and task-based MRI, as well as the polygenic risk score (a theoretical measure of complex genetic risk for depression).
The researchers note that there is no accepted theory linking depression to neurobiology:
“Since there is no established formal theory of the neurobiology of depression, it is uncertain which neuroimaging methods will be best suited to capture clinically relevant information.”
Their study confirmed this lack of connection between depression diagnosis and neurobiology since none of the neurobiological measures tested—even when combined—could reach a clinically relevant predictive value.
Thus, they write,
“How biological Precision Psychiatry can deliver more accurate individualized prediction to improve treatment and patient care remains a central open question at this point.”
Yet the social/environmental variables of social support and childhood maltreatment were each individually able to predict depression at greater than 70% accuracy.
The researchers write that the algorithms were slightly better at classifying people with severe, chronic depression who had been hospitalized and were on multiple medications. That is, the algorithms were not very good at identifying people that might be missed by a human clinician, but were slightly better at identifying the very group that is also easiest for humans to diagnose.
But what’s worse is that when the researchers restricted the analysis to just this group—supposedly the easiest for the algorithm to diagnose—it did not substantially increase accuracy:
“Our complementary subgroup analyses focusing on acutely and recurrently depressed patients, respectively, did not increase predictive performance,” they write.
One explanation they propose is that the diagnosis of “depression” is so wide that it doesn’t do a very good job of capturing individual experiences. Thus, they suggest that the depression diagnosis itself does not represent a single “mental illness” linked to neurobiology, but is rather a broad category holding a variety of experiences, mental states, and levels of functioning that vary widely between individuals.
They suggest that there might be a better way to categorize people based on their specific “symptoms” and levels of functioning. However, as they were unable to find such theoretical subcategories, this remains unproven.
Ultimately, they write,
“The complexity of the MDD phenotype might require a more comprehensive approach that incorporates interactions between neurobiology, the entire body, as well as the environment.”
****
Winter, N. R., Blanke, J., Leenings, R., Ernsting, J., Fisch, L., Sarink, K., . . . & Hahn, T. (2023). A Systematic Evaluation of Machine Learning-based Biomarkers for Major Depressive Disorder across Modalities. medRxiv.org. doi: https://doi.org/10.1101/2023.02.27.23286311 (Link)












When your science is so shit, it is an improvement to replace it by two questions.
Report comment
This is what psychiatry has to show after a half-century of intensive research on this topic done by untold thousands of scientists with untold billions of dollars. No biological theory of depression. No biological tests that are clinically useful let alone that demonstrate the long-assumed pathology of the presumed “illness.” Results from a test involving a sheet of paper with some questions and a pencil are more diagnostically accurate than the best neurogenetic variables modern psychiatry has to offer.
And the authors conclude their findings “should give us pause.”
Report comment
The researchers’ stupidity is rooted in assuming that “depression” is an illness in the physical sense.
It’s time these people put away their electronic toys and signed up for some courses in semantics and logic.
Report comment
Someone should ask these characters if they’d feel comfortable having a robot look after their kids.
Report comment
Because AI cannot lie for money.
————————————
James Hillman “Re-visioning psychology”
People made by enlightenment era into biological machines without rights to the psychological reality does not understand that depression and psychosis, and all of the psyche is not a branch of medicine (medical empiricism). And that this kind of simplify is illegal and completely antipsychological, because medical jargon reffers to nothing. Diagnosis reffers to nothing. The REALM of psychological experiences does not exists in nominal language of people beyond 17th century. Maybe AI knows better. People who asks medicine for their identity are not humans anymore. They are only biological machines and they love it. It is an extreme materialism and pro technocratic thinking based on labels, procedures, and it will be worse. Thinking based on procedures and labels is a programming of enligtenment era leading to technocracy. Because thinking of normal people reffers only to economy, and that economy is based on exploitation of the seemingly non existent reality of the psyche.
————————————————————————————————-
Normal people sacrified their psychological identity for the sake of the elites. And there is no sign of psychiatric victims in this corrupted evil society. And normal people are in “mental health” agenda. State based on psychiatry protect their materialism and super rich predators, not the psyche.
Report comment
James Hillman is brilliant:
“….medical jargon refers to nothing.”
“It is an extreme materialism and pro technocratic thinking based on labels, procedures and it will be worse.”
“Thinking based on procedures and labels is a programming of the enlightenment era leading to technocracy.”
“And there is no sign of psychiatric victims in this corrupted evil society.”
This is an evil society and things probably will get worse in some ways. But I hold out hope for radical change in how people see “mental illness”.
Report comment
I believe in two kinds societes, for abot 150 years, like in movie “Cloud Atlas”. People of the earth and high tech societes “in the sky”. I believe in the alliance of soul and high tech, after destroying technocracy in about 150 years. I believe in society without corrupt corporatism.
I am a great fan of “Sonmi-451”, bacause we share the same thoughts. “Our life does not belong to us.”
I also believe in st. Robert Frobisher.
“”Our lives are not our own. From womb to tomb, we are bound to others, past and present, and by each crime and every kindness, we birth our future.”
—Sonmi-451″
James Hillman, “Re-visioning psychology”
Report comment