After years of misdiagnosis and psychiatric trial-and-error, I discovered that the real problem wasn’t depression — it was a broken brain circuit. Here’s how I found the map psychiatry forgot.
I was born in an emergency C-section after a uterine rupture — deprived of oxygen, but quickly declared “fine.”
At age five, I was diagnosed with auditory processing disorder. No one explained why. It was the first red flag — a subtle sign that something in my brain’s relay system had misfired early on.
Still, I lived a normal life.
I smoked weed through adolescence and into adulthood — and honestly, it worked. I had friends, relationships, creative energy, traveled the world, graduated college, held jobs. I was fully functional.
Then one day, after more than a decade of daily use, I quit weed.
That decision flipped my entire world upside down three months later. Within weeks, I was experiencing symptoms that made no psychological sense:
-
- A neutral, frozen emotional state
- 24/7 ice pick migraines
- A feeling of unreality so pervasive I couldn’t recognize myself in the mirror
Weed wasn’t just a drug I used. Daily cannabis use may have been inadvertently stabilizing my fragile glutamate system, dampening excitotoxic activity. Especially with high-THC strains, cannabis can modulate NMDA receptor activity and reduce unstable glutamate firing. In my case, it seemed to act like a chemical crutch, dampening the overactive, unstable signaling between the thalamus and cortex. It didn’t fix the problem. But it kept the disconnection muted, so I could live a normal life — friends, school, travel, girlfriends.
Eventually, I quit — not realizing what I was holding together. And the fragile house of cards collapsed.
Enter Psychiatry
I figured maybe I was depressed. So I saw a psychiatrist. He labeled me with Major Depressive Disorder and began the ritual: pill after pill after pill. Nothing worked.
So I kept trying. I saw six more psychiatrists. I explained the same bizarre symptoms over and over, but they didn’t fit the manual — so I was stamped with “anxiety,” “atypical depression,” or just “treatment-resistant.”
Eventually, one psychiatrist, hearing that I’d failed every antidepressant, gave me something different: Lamotrigine (Lamictal)— an anticonvulsant.
Within weeks, the ice pick migraines stopped — completely.
It wasn’t just that my mood improved (it didn’t, at first). It was that something deep in my brain had finally calmed — like the misfiring had stopped, and the noise had gone quiet.
Psychiatry Had No Map — So I Found One Myself
Instantly, I was re-labeled: Bipolar II. Because in psychiatry, if an antidepressant fails but an anticonvulsant works, you must be bipolar. But I wasn’t. I wasn’t moody. I wasn’t manic. I was disconnected. And Lamotrigine wasn’t fixing my mood — it was repairing my circuits.
That’s when I stopped trusting psychiatry and started studying neuroscience.
When Lamotrigine stopped the migraines, I knew something was wrong — not with me, but with the model.
I wasn’t “less depressed.” I wasn’t “elevated” or “manic.” What happened was physiological: my brain calmed, my pain vanished, and for the first time in months, I could feel presence. But no psychiatrist could explain why. So I started looking deeper — not into psychology, but neuroanatomy.
The Brain Isn’t a Bag of Chemicals — It’s a Circuit Board
In psychiatry, everything is boiled down to serotonin, dopamine, and vague emotions. But the brain doesn’t operate on feelings alone — it runs on loops, rhythms, and relay systems.
That’s when I found something I had never once heard mentioned in a psychiatric office: the Brodmann system.
It’s a cortical map of the brain — 52 regions, each with a distinct function.
-
- BA7 helps you locate your body in space
- BA31 links self-awareness and time-memory integration
- BA24 (anterior cingulate) is your emotional compass and attention control
- The insula blends physical sensation with emotion
- The precuneus helps simulate yourself in social and spatial contexts
All of these regions are standard in neuroscience and neurology. Yet in psychiatry? Not even mentioned.
And at the center of all these cortical hubs sits the thalamus — the brain’s sensory relay. It doesn’t just route input , it binds consciousness itself. When the thalamus isn’t syncing with the cortex, the entire network goes dark. You don’t just feel sad — you feel like a ghost in your own body.
There’s a name for this condition, even if it’s not in the DSM yet: Thalamocortical disconnection.
My Symptoms Weren’t Psychological — They Were Topographic
For years, I kept trying to explain what I was feeling:
“The world looks foggy. Like it’s in 2D, not 3D.”
“I don’t feel like I’m in my body. I can’t feel time passing.”
“It’s not sadness. It’s like reality doesn’t land in my mind anymore.”
But each time, I was told it was anxiety. Or trauma. Or just more “treatment-resistant depression.” I was given more SSRIs. More SNRIs. None worked.
Eventually, I underwent a quantitative EEG (qEEG) — a scan that measures brain wave activity and shows which circuits are dysregulated.
What it showed floored me:
I had 14 dysregulated Brodmann areas. Every region matched my symptoms:
-
- BA41/42 — auditory processing (I was diagnosed with this at age five)
- BA31 — self-awareness and derealization
- BA7 — spatial disorientation
- BA24 — emotional blunting
- The insula — disconnection from bodily sensation
It was the first objective proof I’d ever seen — proof that my symptoms were coming from real, identifiable regions of the brain.
The Puzzle Snapped Into Place
Suddenly, everything I’d experienced made sense.
My problem wasn’t “depression.” It was signal failure — a literal disruption between the thalamus and cortex, especially in regions responsible for identity, emotion, and sensory integration. And Lamotrigine helped because it modulates voltage-gated sodium and calcium channels — calming hyperexcitable cortical neurons and restoring functional rhythm.
Later, I added Memantine, an NMDA antagonist that regulates glutamate, the neurotransmitter responsible for plasticity, learning, and attention. That’s when things really started to shift. I began experiencing “flickers” — brief flashes of clarity, memory, and realness.
This wasn’t mood regulation. This was circuit reintegration.
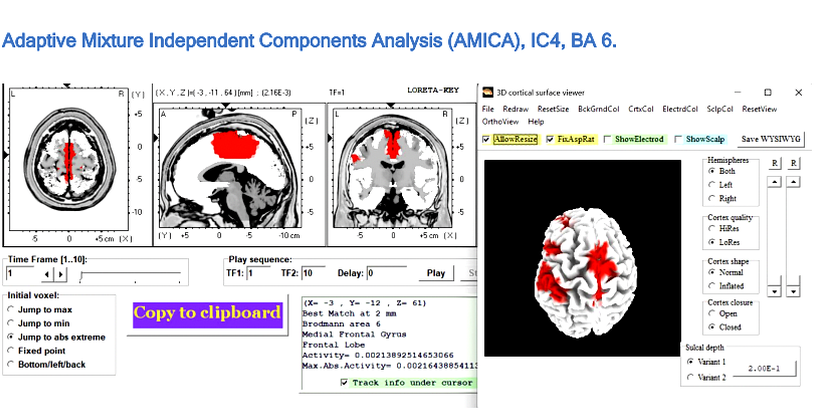
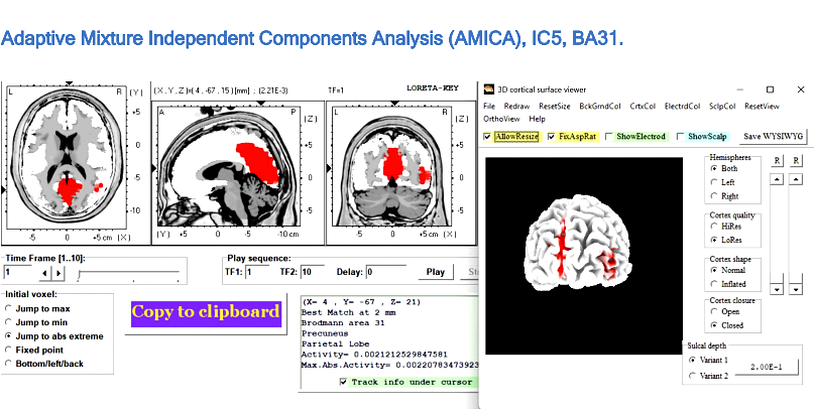
The first image shows BA6, a motor integration area. The second is BA31 — the heart of self-awareness and derealization.
Both circuits were severely dysregulated.
It was a functional disconnect — and psychiatry had no map for it.
Recovery Was Reconnection
When I first took Lamotrigine, the world didn’t instantly return. But something shifted. The ice pick migraines I had 24/7? Gone. The fog of unreality? Slightly thinner.
Lamotrigine was stabilizing my thalamocortical oscillations—allowing parts of my brain to communicate again. Areas like BA31 (posterior cingulate) and BA24 (anterior cingulate)—once dimmed—began to flicker back to life.
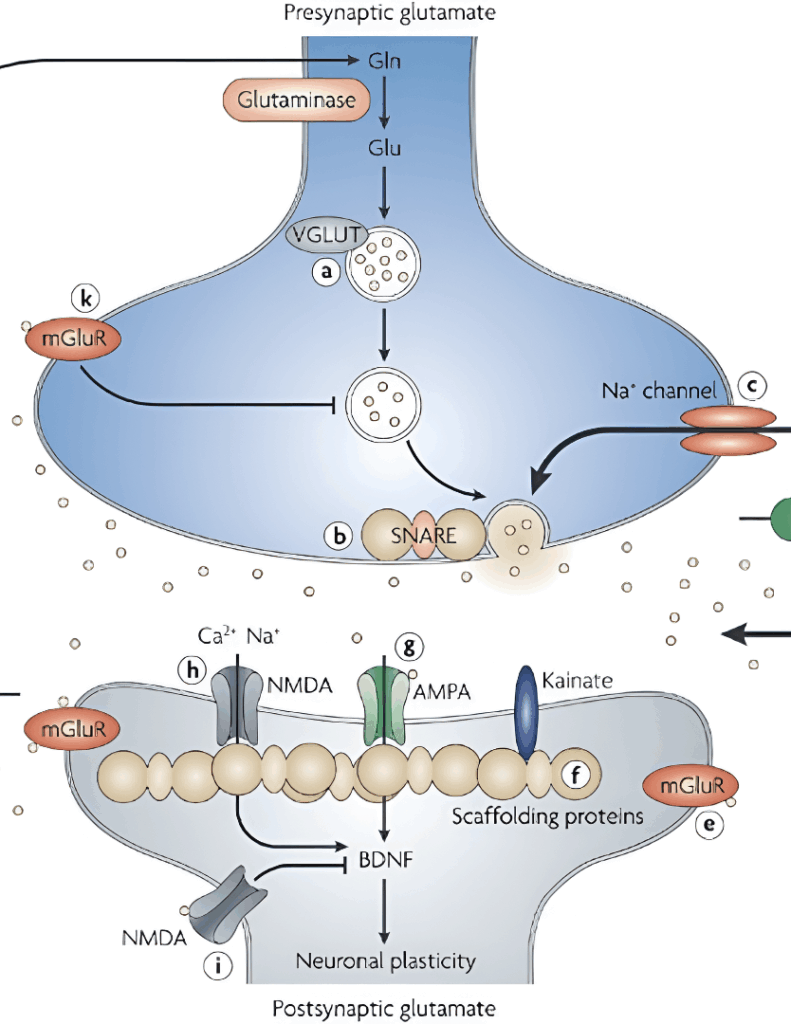
But Lamotrigine alone wasn’t enough. My breakthrough came when I added Memantine—an NMDA receptor antagonist typically used in Alzheimer’s disease. In my case, it wasn’t off-label—it was precise. Memantine didn’t just suppress symptoms. It completed the system.
Where Lamotrigine modulated presynaptic glutamate release, Memantine regulated postsynaptic NMDA receptor activity, creating the quiet, low-noise environment necessary for functional restoration.
The Glutamate Clues Psychiatry Missed
My turning point came when I saw that no single study held the full answer—but several, when integrated, did.
Rodolfo Llinás (neuroscientist) showed that NMDA receptor dysfunction can destabilize the thalamocortical rhythm, producing the exact “disconnection” signature seen in my qEEG.
Gary Parsons (neuropharmacologist) demonstrated that low-dose Memantine can stabilize NMDA receptor activity.
Stuart G. Cull-Candy (synaptic physiologist) revealed that, during recovery, NMDA receptors shift from their immature NR2B form to the mature NR2A configuration, improving signal precision.
In parallel, Chun-Yao Lee (pharmacologist) and colleagues showed that Lamotrigine inhibits postsynaptic AMPA receptors and reduces glutamate release in the dentate gyrus—quieting excess excitatory activity without impairing normal signaling.
Clinicians like Dirk De Ridder (neurosurgeon) and Sven Vanneste (neuroscientist) have already shown through qEEG research that thalamocortical disconnection has a measurable electrical signature—one that aligns precisely with what my own scan revealed.
Combining these insights produced a coherent protocol: Lamotrigine to suppress AMPA/kainate overdrive, Memantine to stabilize NMDA receptors, and time for natural receptor maturation.
Addressing all three major glutamate receptor subtypes—NMDA, AMPA, and kainate—restored balanced excitatory signaling, essential for re-establishing thalamocortical coherence.
This was a patient-led synthesis of four independent neuroscience frameworks into one functional treatment—and it worked.
The Brodmann Circuits Reawakening
Once this cord was restored, the thalamus could finally re-engage to the cerebral cortex. It began to power on the Brodmann circuits — BA31, BA24, BA7, BA41/42, and more — allowing sensory information, self-awareness, emotional tone, and spatial mapping to flow again. And from there, my brain began its return to homeostasis.
The Brodmann circuits that came back online:
BA31: Sense of self, time, derealization (posterior cingulate)
BA24: Emotional regulation and attention (anterior cingulate)
BA7: Spatial awareness, proprioception
BA41/42: Auditory processing, language integration
BA6: Premotor planning and action initiation
BA10: Executive function, future planning, multitasking
BA13: Insular cortex — interoception, emotional salience
BA9: Working memory, social reasoning (dorsolateral prefrontal cortex)
BA8: Eye movement planning, decision making
BA39: Language comprehension (angular gyrus)
BA40: Multisensory integration, speech production
BA46: High-order executive attention
BA11: Social emotion processing (orbitofrontal cortex)
BA20: Visual memory, object recognition
The DSM Failed Me — But My Brain Didn’t Lie
The field of psychiatry is still dominated by the chemical imbalance theory, even though modern neuroscience has long since moved on. They throw SSRIs at anything that looks like sadness. They throw antipsychotics at anything confusing. They throw diagnoses like darts — hoping one will stick.
But what if the issue isn’t serotonin? What if it’s glutamate and electrical synchrony? What if the problem isn’t “mood” at all — but a misfiring thalamocortical system, disrupting circuits like BA31 (self), BA24 (emotion), BA41/42 (sound), and BA7 (space)?
That was my case. And I have qEEG data to prove it.
My circuits weren’t emotionally blocked. They were electrically disconnected.
We Need a New Diagnostic System — One Based on Brain Maps, Not Labels
It’s time to retire the DSM as the gold standard.
It’s time to stop calling things “treatment-resistant” when we haven’t even mapped the brain.
The future of psychiatry isn’t in more labels. It’s in qEEG, neuroimaging, and AI-guided pattern recognition. It’s in matching symptoms to circuits — and using that map to reverse engineer recovery.
I’m not a doctor. I’m a patient. But I solved what six psychiatrists could not. Because I used neuroscience, not trial and error. Because I listened to my brain — not their model.
I am living proof that psychiatric misdiagnosis can steal years from a person’s life. I am also proof that a brain — even a broken one — can be rebuilt.















Oh wow, what an interesting mind this one has. Only mad people like me and him can sound as delightfully mad and sane as this. Probably you might be right with all your theories my friend and if I was a psychiatrist, I wouldn’t be betting against your suggestions. But honestly, it doesn’t seem all that important to me what the brain is doing. Whether an explanation would involve serotonin receptors or neural circuits doesn’t alter a thing about the actual problem which takes place within consciousness, and can be understood only there. If your theories are correct, they are based on your own conscious observation, so the truth is clearly, manifestly, undeniably that the only cure for all human ills including so called ‘mental illness’ is in consciousness, not in the immeasurably complex and perplexing functions of the galaxy of neurons we call the brain. But perhaps that fantastically complex brain produced all your theories from inspiration. I can’t judge, especially not a brain that is as quirky and creative as yours.
Report comment
Sure glad the blood Brain barrier always prevents oral glutamate from crssing into the CNS otherwise I would be sure worried about all that MSG being shoveled down everyones throats these days
Report comment
Michael did what psychiatry only pays lip service to: look for physical causes for psychic unease. But switching from brain chemicals to brain circuitry just switches one narrow-minded approach for another. Not a good idea.
Report comment
I didn’t replace one narrow chemical theory with another. What I documented was objective qEEG evidence: cortical undercoupling, theta dominance, and PAC deficits… the same abnormalities described by Llinás, Vanneste, and De Ridder in thalamocortical dysrhythmia. That’s not speculation, it’s measurable physiology. Psychiatry has been content with vague metaphors like ‘serotonin imbalance,’ while ignoring circuit-level dysfunctions that can actually be recorded. To call that narrow-minded misses the point: evidence expands the frame, it doesn’t shrink it. If we want psychiatry to move forward, we have to acknowledge the brain’s rhythms as real contributors to lived experience.. not dismiss them because they’re harder to confront. Dismissing evidence because it complicates the story isn’t wisdom…it’s avoidance.
Report comment
Like anything else, the qEEG studies show correlations, not causation, and they associate very poorly with the DSM categories on a disorder-by-disorder basis. Maybe (MAYBE) thalamocortical dysrhythmia is an actual “disorder,” caused by something that somehow causes abnormal qEEG scores, but it still tells us nothing about what is really causing the problem, nor what anyone could possibly do to alter their qEEG wave patterns.
Report comment
I’m not replacing the DSM.. I’m saying circuit-level dysfunction creates the very profiles psychiatry later labels as disorders.
Excessive glutamate excitotoxicity is already documented as the mechanism driving thalamocortical dysrhythmia (TCD).
My qEEG showed that exact pattern.
This isn’t just correlation — Llinás, Jeanmonod, and De Ridder demonstrated that NMDA/AMPA imbalance destabilizes thalamocortical rhythms, and that interventions like Lamotrigine + Memantine restore them.
Saying nothing can alter qEEG wave patterns’ ignores decades of published data and clinical practice.
That claim isn’t just wrong… it dismisses proven neurophysiology.
Report comment
Sorry, not convinced. There is no reason to expect that any “circuit level dysfunction” consistently and predictably creates DSM “disorders,” because the “disorders” themselves have been shown to be invalid, as they subjectively grouped together heterogeneous groupings based solely on external observations.
When you have to talk about “Excessive glutamate excitotoxicity,” you’re clearly not talking about a measurable cause, but only a correlative observation. Why does someone have “EGE?” How does it happen? What’s the mechanism? Do ALL people with a particular “diagnosis” have EGE? Do ALL people with EGE get a particular diagnosis? Again, the diagnoses are so totally subjective that such predictiveness is absolutely not conceivable. If we START with the EEGs and then find a consistent CAUSE of the EEG “abnormalities”, then we might have a new “diagnosis” like TCD. But to expect that to directly correlate with these subjective DSM categories is kind of laughable. I mean, I’m open to listening to your proof, but I am absolutely certain you don’t have it, even if you can name a bunch of researchers who agree with you.
Report comment
You are like Joel Stern who is also meticulous with the facts and excellent in all refutations. You and Joel should be running the show here and writing articles. Kick those loopy conceptual cretins out the way and replace them with yourselves. I reckon Joel is a young man probably but he’s one of the few young men that kick butt with facts rather then theories, just like yourself. And no I’m not pitching to write for MIA because I never ever in a million years would do anything like that because it’s way to square. Unless I could put a little advert at the bottom of my articles advertising my penis up the whoopsie cure for schizophrenia.
Report comment
Well, Zeroxox, thanks for your complimentary remarks, but let me correct one misperception: I’m actually not young chronologically, but I’d like to believe that I’ve preserved a youthful spirit of inquiry and curiosity. I try to ask probing questions because I think the Socratic method can be useful in dispelling misguided and even harmful beliefs, of which there is certainly a plethora in the mental health field (just look at the recent MIA article on the self-serving rationalizations of psychedelic therapists who sexually abuse clients under the pretext of “healing” their traumas).
Report comment
The qEEG changed everything — it flagged excessive theta, PAC disruption, and frontal–temporal undercoupling. Instead of a vague DSM label, I had a mechanism. That shifted me from symptom-chasing to targeted NMDA modulation: Lamotrigine + Memantine, exactly what clinical logs from Dogris, De Ridder, and others show restores thalamocortical rhythms. I don’t accept that answering a PHQ-9 questionnaire should label me for life — I want objective data. For example, it’s no different than getting an X-ray to see if a bone is broken.
Report comment
OK, thanks for your response. I agree 100% that the PHQ-9 and other “assessment tools” are generally bullshit.
Report comment
I get that you looked at how the brain functions, and saw where reactions and responses were shut off. Absolutely, and when I guided my disabled brother through his adult life, when he was intellectually disabled and had sensory and balance issues and could not advocate for himself – I saw the chronic misunderstanding perpetuated in almost all care and support systems, which do not work in sync, they work separately, leaving frequent gaps that disrupted his participation – but nobody focused on those, they only focused on symptoms he showed when he felt lost and unable to keep up. Except me, who watched him over time, and saw his renewed efforts and new learnings, then his confusion over direction and meaning when he was left behind by glitches and no professionals noticed, or saw it clearly enough to fix, so the chronic misunderstanding that had been his life path from the start, would be repeatedly retriggered.
So, I get the principle. And your early childhood handicap – it distorts one’s abilities, but the people around us are not noticing, their focus is elsewhere.
I was a preemie baby, 1.5 months premature. That could have started my lifelong experience with being misunderstood, but my physical symptoms paled in the face of what my delay being sent home, meant to my start in life. My older sister, mother’s first girl, had been greeted with eager interest, by her, my father and older brothers. Not me: I was no longer special, and staying in that hospital in an incubator for 1.5 months, likely disconnected me as well, from my mother and our troubled home in the middle of life transitions, social class climbing, father ill and both parents drinking. My childhood, I felt peripheral, not one of the family. I was rescued by a British family neighbor – not realizing that this acceptance would be seen by my older siblings as “proof” that I did not belong to our home. Yikes.. Long story – but to note that the disconnections you mention, were not just “in your brain”, but in a world so focused on individuals and future goals, they miss the need for coherence and someone who watches and cares about that.
Report comment
Thank you for sharing—that’s exactly the problem. Psychiatry keeps chasing surface symptoms while ignoring root dysfunction. My qEEG showed circuit-level abnormalities backed by neuroscience, yet doctors only saw “depression.” Just like your brother, the system misreads the signals. Until psychiatry looks deeper, patients will keep falling through the cracks
Report comment
What you’re describing sounds like a iatrogenic brain injury. From your C section it sounds like. And I think you’re brilliant!! Way to go! You helped yourself instead of staying trapped in the mental system merry go round that is anything but merry! What I’d love to know is how did you advocate for yourself? How did you get the tests ordered? Did you pay out of pocket? How did you get the prescriptions? I can’t get an MD to respect me enough to see anything but a schizophrenic mental patient sitting before them. They all just refer me back to psychiatry. They will not test me for the brain injury I got from medical treatments because they claim their treatments could not possibly have given me a brain injury!
Report comment
No doctor ever understood my case — I was misdiagnosed for years. What changed everything was using AI to cross-reference my qEEG results with over 30 research papers and case reports from people showing the same brainwave abnormalities. That’s how I was able to identify the correct diagnosis and treatment path myself.
In my case, a qEEG was the turning point — it gave me the data I needed. That was the best brain scan in my situation to give me evidence of my disorder.
Report comment
So what did that change for you? What did you do differently once you got your qEEG results and the “correct diagnosis?” What was the new “treatment path?”
Report comment
How did you get this test prescribed and by who? Who does one approach to have this test. When I have brought up similar requests I’ve been dismissed and issue dropped. Please advise on this question. Please don’t avoid me as I’ve been in the past. I have not heard this question answered
Report comment
Very interesting. Makes sense all should be tested. Great article. Would appreciate locations available for this test. Please advise. Thank you.
Report comment
Michael,
I think your research is brilliant. Auditory processing disorder is associated with having MTHFR C677T mutations (which cause low folate).
https://www.sciencedirect.com/science/article/pii/S0969996125000798
Marijuana also lowers Folate (and when you stop using it dysregulates Folate).
Low Folate, MTHFR C677T mutations and drugs like marijuana increase homocysteine and that causes NMDAR activation and excitotoxicity. Look at the Figure 1 picture on this paper.
https://www.mdpi.com/2072-6643/15/17/3859
P.S. If you get tested and turn out to be positive for MTHFR mutations please let me know, I’m trying to prove something.
Report comment
Thanks for sharing this. I’ve already had my folate, B12, and homocysteine levels tested — all normal — and I supplemented folate daily with no effect on symptoms. That pretty much rules out MTHFR or folate metabolism as the driver in my case.
My qEEG shows clear circuit-level abnormalities (PAC, frontal–temporal undercoupling, theta overdrive), which line up with thalamocortical dysrhythmia literature. That points directly to NMDA/AMPA dysregulation at the circuit level, not a systemic folate issue.
Report comment
You mean like the dysregulation seen in people with auditory processing disorder
who exhibit elevated glutamate-related proteins and reduced GABA-related proteins in the cortex ..and alters basal cortical activity
Report comment
Yes, exactly — that’s the same mechanism I was describing. Elevated glutamate activity with reduced inhibitory balance shows up in auditory/cortical circuits and creates the basal dysregulation my qEEG flagged. I focused on the circuit-level effects (theta overdrive, PAC loss, frontal–temporal undercoupling) rather than the upstream contributors like MTHFR/folate metabolism, but we’re really pointing to the same chain of dysfunction — excess glutamatergic drive leading to disrupted cortical rhythms.
Report comment
Why did you stop weed?
Report comment
Just wanted to stop and live a better life going to the gym everyday. I never knew the consequences of what was hiding underneath.
Report comment
So you couldn’t work out while you were smoking?
Report comment
It’s not about whether I could physically work out while smoking — it’s that weed was suppressing glutamate and masking the symptoms of my underlying condition. Once I quit, the suppression lifted and the real dysfunction showed up. That’s a neurochemical reality.
Report comment
Thank you for sharing your story. It’s a good reminder that there can be a half dozen different etiologies behind a similar set of experiences, and a half dozen ways of making meaning of them. It makes me feel both appreciative and sad that you had to do so much research yourself to help understand what was going on for you, when many of us don’t have the time, skill or resources. Psychopharmacology might not always be the answer, but we should have better options that hopefully stories like yours can help spur. Thank you for sharing your piece of the puzzle!
Report comment
I would like to hear from a psychiatrist as to what they think. Can someone show this article to a psychiatrist?
Report comment
Psychiatrists aren’t trained to interpret qEEG patterns or thalamocortical dysfunction. Their training is built on DSM checklists and symptom clusters, which is why so many people like me get mislabeled or given the wrong drugs. My case is not about vague categories — it’s about measurable abnormalities (PAC deficits, frontal–temporal disconnection, theta overdrive) that neuroscientists like Llinás, De Ridder, and Vanneste have already demonstrated and treated successfully. To say we should just ‘ask a psychiatrist’ is missing the point: the profession isn’t equipped to handle circuit-level evidence. That’s why research and clinical neurophysiology, not symptom lists, are what actually drive recovery. evidence.
I would love for psychiatry to understand this…but right now, they don’t
Report comment
We’re all doomed, are we not, if our brains (left, right and middle) are generators of consciousness; all capable of what not if our brains act as receivers and transmitters of Consciousness.
Given humanity’s inbreeding, prenatal intoxications, and birth traumas, our postnatal depressions contributed to by ethnic/racial/cultural/societal/human conditioning, out poisonings with prescription and recreational psychotropics, mercury, lead, arsenic, all kinds of -enes, insecticides, pesticides, nano plastics, phyto and other estrogens etc. etc. etc., it is no wonder, is it, that each of our brains can all only function exactly and precisely as they need to at any moment….to endure that
“No doubt, the universe is unfolding as it should,”
“Life will give you whatever experience is most helpful for the evolution of ‘your’ consciousness,” etc?
Wishing you love, light, laughter, comfort, joy, mirth and merriment and more – or all you’d wish yourselves with your broken brains AND much more, galore.
Tom.
Report comment
Wow: ice-pick migraines 24/7 for how many 7’s I wonder?
Best wishes.
Tom.
Report comment
Every day, nonstop — until Lamotrigine finally stabilized the glutamate chaos driving the thalamocortical misfiring.
Those “ice-pick” migraines weren’t random — they were the brain’s warning sign of excitotoxic overload and rhythm instability. Once the circuits were stabilized, they stopped.
Report comment
For how many weeks, please, Michael?
And how EVER could you think straight then, please?
PEACE!
Tom.
Report comment
I didn’t think clearly at all I had to go to the Emergency room twice… The headaches I had were on the same level as cluster headaches — which neurologists consider the most painful condition in medicine. It was like having an ice pick driven into my skull, nonstop, until Lamotrigine finally calmed the glutamate chaos.
Report comment
How many weeks of 24/7, nonstop, ice-pick headaches, please, Michael?
And do you propose any pathophysiology for them, please?
And you said it took the lamotrigine (more) weeks to calm your headaches?
Thank you, again!
Peace and joy!
Tom.
Report comment
I think we may be circling back to a rebranding of “phrenology” with the tools we have today. My point is this: even though we now know phrenology was wrong, the underlying intuition that sparked it—a gut feeling that there’s something deep in the brain’s topology worth investigating, that the structure of our physical brain holds a map to the self—that part is not mapped out. It was a feeling that there was a code to be cracked.
I agree with a lot of what you are saying. I am just pointing out that you are extending the original call. Modern neuroscience, with its powerful brain mapping technologies like fMRI, is finally answering that call with real data. But in doing so, it risks repeating phrenology’s and psychiatry reductionist mistakes by assigning complex human traits to specific, neatly defined brain circuits. While the tools are scientific, the temptation to create a new, digital phrenology – where we ‘read’ a person’s character, aptitudes, or risks from their brain scan – is a serious ethical concern.
So let us pursue this map, but let us not completely totalize it. The map is not the territory. The scan is not the soul. We are finally investigating the deep topology they felt was there, but we must remember that a circuit for an activity is not the same as the meaning of the experience itself.
This means a diagram of the brain is not the same as a living, thinking, feeling human being. You can study the wiring of a computer (the brain), but that doesn’t explain the beauty, chaos, and meaning of the internet (the human experience).
Report comment
Thank you Dogworld for raising this point. I agree that modern brain mapping risks becoming a kind of digital phrenology / if we overstate what scans can reveal. That’s why I clarified in the discussion that my claim is narrower: a circuit signature can guide care, but it is not the whole of human experience.
In my case, brain mapping was critical for moving past a mislabel of “bipolar” and finding the right treatment path. You are right that no two brains are the same, but this is exactly why psychiatry needs tools beyond the DSM. Advances that combine objective biomarkers with lived experience can help prevent misdiagnosis and lead to more accurate, individualized care.
Psychiatrists also need more tools to distinguish when a patient’s problems are neurological versus psychological. In my own journey, my psychiatrist even apologized, admitting that the field needs a bridge between these two worlds. Brain mapping gave me that bridge.
Report comment
And what does it mean, please, for one’s brain to “bind consciousness,” as you mentioned?
Comfort and joy!
Tom.
Report comment
Great research work! Thank you for sharing your inspiring story.
Report comment
If indeed lamotrigine ever actually helps anyone’s brain function – by which I suppose I may mean in the sense of facilitating one’s accessing of “higher,” more humorous levels of consciousness – other than via the presumably unlimited potential power of placebo, I mean, something which may render an attempted accurate assessment in any animal impossible to attain – then I suggest it may be by addressing the same underlying causes as those which some cases of lithium supplementation (or poisoning) address – an underlying deficiency of magnesium in form/s the brain can use?
If it’s true that (nonvascular) brain matter has no sensory nerves endings (or those so-called but non-existent nociceptors), then presumably headaches are caused by sensations affecting the skull and/or intracranial blood vessels, so that any “ice-pick migraines” or “ice–pick cluster headaches,” like a majority of trigeminal and occipital neuralgias, more likely, I suggest, be psychosomatic in origin.
I can provide some references if anyone is interested.
“Oh, what a tangles web we weave
When first we practice to deceive.” – Walter Scott.
“Methought I heard a voice cry, ‘Sleep no more!
Macbeth does murder sleep: the innocent sleep,
Sleep that knits up the ravelled sleeve [or “sleave”] of care,
The death of each day’s life, sore labor’s bath,
Balm of hurt minds, great nature’s second course,
Chief nourisher in life’s feast.”
(Macbeth, Act 2 Scene 2)
Comfort and joy!
Tom.
Report comment
I never claimed Lamotrigine works for everyone.. I’ve only spoken about my case. My qEEG was flagged with clear abnormalities, and Lamotrigine addresses the exact glutamatergic/sodium channel issues that showed up in my scans. That’s not placebo, and it’s not magnesium speculation. dismissing headaches or neuralgias as ‘psychosomatic’ ignores decades of neurovascular and electrophysiological research. If you want to debate, at least keep it grounded in real data.. not guesswork
Report comment
While still lacking blood/serum/plasma or other accurate, reliable, convenient, cheap and readily available appropriate blood or other tests for levels of magnesium ions likely to cross our blood-brain barriers, there is reason to suspect that the usual diets of many of us in the West may nowadays be at best marginal in their daily magnesium sources and masses optimal for brain/neuronal function.
Please see last ref. (7) below.
If this is the case, then I suggest we might anticipate that anyone whose regular diet/intake deteriorates in this regard – as it may be anticipated to do during bouts of “anxiety/depression,” angst, agitation and/or of “weeks-long ice-pick migraines,” might be expected to have any previous deficiencies in magnesium exacerbated, or new ones provoked.
I suggest that ions such as those of phosphorus, calcium or lithium which are understood to interact with serum magnesium, along with molecules/drugs such as the Vitamins D or lamotrigine which affect serum and cellular calcium levels, may be expected to vary our levels of available magnesium within and outside the brain.
1. https://www.madinamerica.com/2024/07/desperate-measures-ghaemi-lithium/#comment-308913 MIA Article where lithium admitted by Ghaemi to perhaps alone among psychiatric drugs to have been shown to have brought better outcomes – a conclusion rebutted by Moncrieff and Plöderl:
“In a previous paper, Ghaemi declared that lithium ‘is the only drug in psychiatry which is proven to be disease-modifying,’ by which he meant that it affects the pathophysiology of the disease process and the course of the illness, including mortality due to suicide. In contrast, other psychiatric treatments are non-specific, ‘symptomatic’ treatments, according to Ghaemi, which have no effect on the underlying condition (Ghaemi, 2022).”:
2. https://pubmed.ncbi.nlm.nih.gov/35653111/
3. https://pmc.ncbi.nlm.nih.gov/articles/PMC9533115/
– “Conclusion: Evidence from randomised trials is inconclusive and does not support the idea that lithium prevents suicide or suicidal behaviour. More data are needed to estimate the effect of lithium with more precision in general, and in subgroups of patients, specifically.”
4. https://youtu.be/0VyH1laOd2M?si=c3Pk147lsbzoERdP
– Breakthrough with Healing Chronic Pain | Howard Schubiner | Talks at Google, but please see any of Howard Schubiner’s presentations or papers on chronic pain, “anxiety/depression,” insomnia, fatigue and a host of other conditions such as tinnitus, vertigo, idiopathic epilepsy…
5. https://link.springer.com/chapter/10.1007/978-1-4612-3324-4_10
– The Interaction of Lithium with Magnesium-Dependent Enzymes
6. https://www.sciencedirect.com/science/article/abs/pii/S0924977X96003847
– “A calcium antagonistic effect of the new antiepileptic drug lamotrigine”
Lamotrigine, Calcium Channels in Context of Low Magnesium
7. https://journals.sagepub.com/doi/10.1046/j.1468-2982.1996.1604257.x
– Prophylaxis of Migraine with Oral Magnesium: Results From A Prospective, Multi-Center, Placebo-Controlled and Double-Blind Randomized Study
A Peikert, C Wilimzig, and R Köhne-Volland – as referenced in an article by Danielle Wilhour, Assistant Professor of Neurology, University of Colorado Anschutz Medical Campus in “The Conversation” (US), “Migraine sufferers have treatment choices – a neurologist explains options beyond just pain medication
Published: July 11, 2022 8:29am EDT:”
8. https://www.youtube.com/watch?v=GIVqou1znMQ
– “Subclincial Magnesium Deficiency: Brain Health and Beyond,” by Bassem El-Khodor, PhD.
Kindest regards and wishing everyone health, comfort and joy,
Tom.
Report comment
Hey Tom,
Perhaps I missed it but I am sure someone with the knowledge you have on all this that you know how many different types of magnesium there are and how not all are well tolerated by the individual human body. Certain forms for instance magnesium citrate destroyed my stomach lining for the brief time that I took it from a massive bottle that I ended up having to throw in the garbage because I clearly could not handle at least at that particular time for whatever reason although I’m not gonna try again cause it was so painful this particular version versus other Mag forms although I realize you covered a lot more than simply magnesium in the above post so maybe you felt it too cumbersome to go into since you were already talking about so many other substances and/or supplements in your comment but don’t you think it’s important to delineate?
Here is a list of common magnesium types:
Magnesium Citrate: A common and affordable form with high bioavailability, often used for constipation due to its natural laxative effect. (Not for me but who knows if it was a reputable company that was making that particular one since not even the unimpressive FDA regulates these much as I understand so maybe it was a bad batch?)
Magnesium Glycinate (or Bisglycinate): Known for its excellent absorption and calming effects, it’s a good choice for sleep, anxiety, and stress, with minimal laxative effect.
Magnesium Oxide: A common and inexpensive form with poor bioavailability, it can cause stomach upset and is often used as a laxative.
Magnesium Malate: Another highly absorbable form that may help relieve chronic pain and is sometimes used for conditions like fibromyalgia.
Magnesium Chloride: Easily absorbed and used in oral supplements, it is also common in topical applications like oils and lotions.
Magnesium Sulfate: Also known as Epsom salts, it is primarily used in bathwater to soothe sore muscles.
Magnesium Taurate: Combined with the amino acid taurine, it may help regulate blood sugar and blood pressure and has calming effects.
Magnesium L-Threonate: This form is noted for its ability to cross the blood-brain barrier and may support cognitive function and brain health.
Magnesium Orotate: May promote heart health by helping to produce energy in the heart and blood vessels.
Magnesium Lactate: A gentler option on the digestive tract with good bioavailability, also used as a food additive.
Magnesium Carbonate: A common form of magnesium found in antacids.
Magnesium Hydroxide: Found in liquid form and used as an antacid and laxative.
Magnesium Aspartate: Used for cellular energy and overall health, it is well absorbed.
Nonetheless considering there are literally 13 different types of magnesium I believe it’s important for us to discuss which ones are best or at least discuss the fact that there is not just one single way to get magnesium and depending on which one of the 13 you decide to choose and use could make or break your experience on the needed mineral or supplements or substance whatever you wanna call it , no?
Apologies if I missed where you broke all 13 of these down since I didn’t really click on all of your links but maybe one of them contained all of this info and I just didn’t notice?
However even if a link did happen to discuss not only all 13 but to go into detail on all of them individually I think that would’ve been important to include in the body of the text but no one‘s perfect and I think now that I’ve pointed it out we are hopefully all now all the better for having it reiterated just in case. : )
(by the way I put a “ throwing up emoji but it doesn’t allow me to actually post it even though it does pretend to let me place it in the body of the text but it doesn’t actually save so I just want you to know there was an emoji projectile vomiting next to “all American diet” lol!
And I’m sure everyone, including me , appreciates how thorough you have been otherwise (if I’m not already wrong here lol) on pretty much all other topics regarding your preface or thesis about what I think to be the rightful ilk in the “All American diet” lol !
Report comment
Michael, please accept my very sincere apologies.
No disrespect in the very least intended.
I fully accept your sincerity and desire to help others with your own fascinating and intriguing essay and comments above.
My very, VERY kindest regards and warmest wishes for your future.
Tom.
Report comment
https://youtu.be/rYz_ApWYeg0?si=sj7KX4lbYB8nGwBZ
Plenty more ref’s and data on psychosomatic medicine and also on
calcium,
lamotrigine,
magnesium
and lithium
coming up shortly, if Steve McCrae is ok with that, please.
Much love
Tom.
Report comment
Is this like a Crash Course and functional medicine basics?
Report comment
Jason, thank you very, very, very much, indeed, for your most kind remarks.
No, I don’t believe that is like a crash course in functional medicine basics, which I think might look more like this:
At a human being’s most functional, that is to say when at her highest levels of human consciousness, nothing can disturb the physical or psychic harmony of that being, of that human who has transcended from a state of mostly human doing (thinking and emoting very much included) to a state of human…being.
Maslow may have been among those who intuited this, perhaps?
If the Buddha succumbed to a fatal dose of food poisoning – and I am not saying he did – this may only have been possible if he was no longer in a state of pure enlightenment, and so utterly immune to slings and arrows and all sorts of toxins, much as in:
Mark 16:18
King James Version:
“They shall take up serpents; and if they drink any deadly thing, it shall not hurt them; they shall lay hands on the sick, and they shall recover.”
If any Vietnamese monk self-immolated not just without showing but also without feeling any pain or discomfort, perhaps he may have been in such a transcendent state at the time, as I am hoping Joan of Arc may have been during her burning at the stake?
https://en.wikipedia.org/wiki/Th%C3%ADch_Qu%E1%BA%A3ng_%C4%90%E1%BB%A9c
https://en.wikipedia.org/wiki/Th%C3%ADch_Qu%E1%BA%A3ng_%C4%90%E1%BB%A9c
I suspect we may be still far from being capable of estimating what any human’s optimal diet might be but, in the understanding that “LIfe will give you whatever experience is most helpful for the evolution of your [our, the] consciousness,” as Eckhart Tolle put it, as per my original comments above, I trust that all our seeming poisonings and dietary deficiencies must serve some Cosmic Purpose/s, or something far, far grander than we can anything we can yet understand by “purpose” or “meaning.”
I look to the examples of John of the Cross and of Viktor Frankl to see what can be achieved despite or because of being imprisoned and fed truly awful diets..
The Findhorn Foundation/Community or phenomenon may point to how we may be guided towards actions which enable us to intuitively grow the most nutritious produce, as well as how best to “cultiver nos jardins?”
https://www.youtube.com/watch?v=tuAOQ9KQLE0
https://www.youtube.com/watch?v=QT4xwLwxi9o
…and, speaking of “crash courses!”:
https://www.youtube.com/watch?v=vOetKgNPs4Y
and, wherein “crash course” is mentioned, I think:”
https://www.youtube.com/watch?v=e0D1_Vh13oI
Acute magnesium deficiencies tend to manifest themselves immediately and in magnificently florid dramas in cows, capable of transforming the most docile and bovine of bovines into the least bovine of raging, murderous maniacs in moments, and then very quickly into cadavers if not expeditiously and successfully treated
One cow, apparently early in a hypomagnesaemic episode, fooled my newly qualified veterinarian cousin who treated her elevated temperature with some antibiotic (not exactly “functional veterinary medicine,” it must be conceded!). Later that night, she went so berserk as to pull the metal stanchion from the stone wall of the cow byre in which she was tied by chain, collapse the rubble the wall separating that space from the master bedroom wherein had been sleeping his client and his wife, charge around the bedroom, threatening to kill the couple before collapsing and dying right there, on the floor. After that, Dick tried his best to miss no more early hypomagnesaemic tetanies, needless to add. And yet other cases presented merely as a subdued, dull animal – as this cow may have done when Dick saw her.
Funny thing, magnesium; less funny, perhaps, lithium…and not funny, at all, those unfunny funny pharms filled with involuntary and other detainees which states still sanction.
That we should ever have had any medicine, such as psycho pharmacilogy, which was other than “functional” medicine may seem very funny very soon, too, don’t you think?
By the way, curiously, magnesium deficiencies in humans seem to be an awful lot more subtle, more complex and more variable than in cattle, and, while Howard Schubiner suggests, I believe, that approximately 90% of migraines may be psychosomatic, or “neuroplastic” in origin – emotionally based – I do think that more than 10% may indeed respond to generous Mg supplementation above any placebo-based responses, although some, at least, of those migraines may have more than one causal factor involved, I suspect. I say this based on decades of firsthand experience of severe headaches.
Heartfelt thanks again for your very generous praise, which means much more to me than I think you can imagine, Jason!
Comfort and joy, and everimproving health!
Tom.
Report comment