I am going to back up Sera Davidow’s blog post with an examination of the research regarding Mental Health First Aid (MHFA), and how this literature details the weakness of relying on evidence-based practices. Now, MHFA is designated as an evidence-based practice, but what does that really mean? All it means is that the program has gotten enough grant money to get some research that proves it meets its designated outcome criteria. This does not mean the real-life outcomes for the people involved, or for society, are desirable or helpful.
What are the Potential Problems with Using an Evidence-based Practice Designation to Judge a Program’s Quality?

- We have made a mistake in correlating a program’s ability to reach its stated outcomes with the program’s ability to actually help people.
- Clinical outcomes are different than recovery outcomes. In other words, when you ask people what is important to their recovery, they say stuff like, “housing, a job, friends, having meaning and purpose, having a life.” But when you ask clinicians what is important they say stuff, like “regular checkups, staying on meds, avoiding hospitals, and having less symptoms.” But studies show that recovery doesn’t even correlate with clinical outcomes. So all these efforts that produce good clinical outcomes don’t do squat to actually support recovery. There is a great BRSS-TACS webinar archived that tells you how to use recovery outcomes.
- Most outcome measures do not include science-based user input into research design. Who’s evidence is in the base? Not neccessarily ours. There is a saying, “We are the evidence.” So why aren’t we being included in study design? The Patient Centered Outcomes research was designed to address this stuff, but based on their priority list for mental health, they forgot to include us in their program design.
- It takes a lot of money to get a program into the evidence-based practice registry and most programs fund this cost by selling rights to their program later. So, instead of focusing on what works, many programs are focused on what is copyrightable and what is marketable. Dennis Embry has a heavily cited research article showing that most evidence-based practices can be broken down into “kernals,” of cheap, free, effective interventions. And the rest of the “evidence-based practice” is just branding junk heaped on top of the effective kernal.
So how does this play out when we start looking at Mental Health First Aid? It may be an evidence-based program, but is it helpful? According to the listing in the SAMHSA’s registry of evidence based practice, the desired outcomes for Mental Health First Aid are:
- Recognition of schizophrenia and depression symptoms
- Knowledge of mental health support and treatment resources
- Attitudes about social distance from individuals with mental health problems
- Confidence in providing help, and provision of help, to an individual with mental health problems
- Increasing Mental health
So, Does Reaching these Outcomes as the “Evidence-based Program” Actually help people? The Million Dollar Question:
- Does disease-label education support people’s ability to get through hard times? Teaching disease-label awareness is counterproductive in many ways. The DSM-5 research committee found that trained pyschiatrists could only agree on disease labels 40-50% of the time, so teaching lay people and interested bystanders to identify these disease labels is a bit ludicrous. Making mental illness scary and serious reduces people’s ability to help each other, and reduces recovery outcomes. This is lost time that could be spent educating about wellness, trauma informed care, resilience, self-care, or peer support.

You can get together a roomful of bigwigs, here at the Carter Center social inclusion forum, but are they listening? - Is knowledge of mental health support helpful? Probably, but we could actually do this without the disease label education. The eCPR program certainly does. Is knowledge of treatment resources helpful? Well, only if the treatment resources do more good than harm. Careful examination of the data on the Mad in America site says that maybe getting them into treatment is not the best thing you can do for a friend in need.
- Does disease-label education actually improve attitudes about social distance/stigma? This depends on how you define stigma. Many disease-model advocates define stigma as “making labels acceptable.” Whereas a better definition is, “reducing prejudice and discrimination against people in distress.” MHFA obviously chooses the first definition. Specifically, MHFA used clinical vignettes to measure social distance, which means they gave a person a story about someone obviously in mental health crisis and said, “Would you want to hang out with this person, live next to them, hire them or marry them?” This type of research has a lot of weaknesses, but the biggest one is that really we should measure if someone is willing to hang out with/marry/employ someone NOT in crisis, maybe someone who recovered. (Am J Psychiatry 167:11, November 2010 p.1289) But more so, the number #1 and #2 sources of stigma are the disease labels and the mental health professionals. So why would re-inforcing a need for mental health labels and a need for mental health professional actually reduce stigma? It doesn’t. There are scads of research articles, starting with this one, showing that disease label identification only increases stigma.
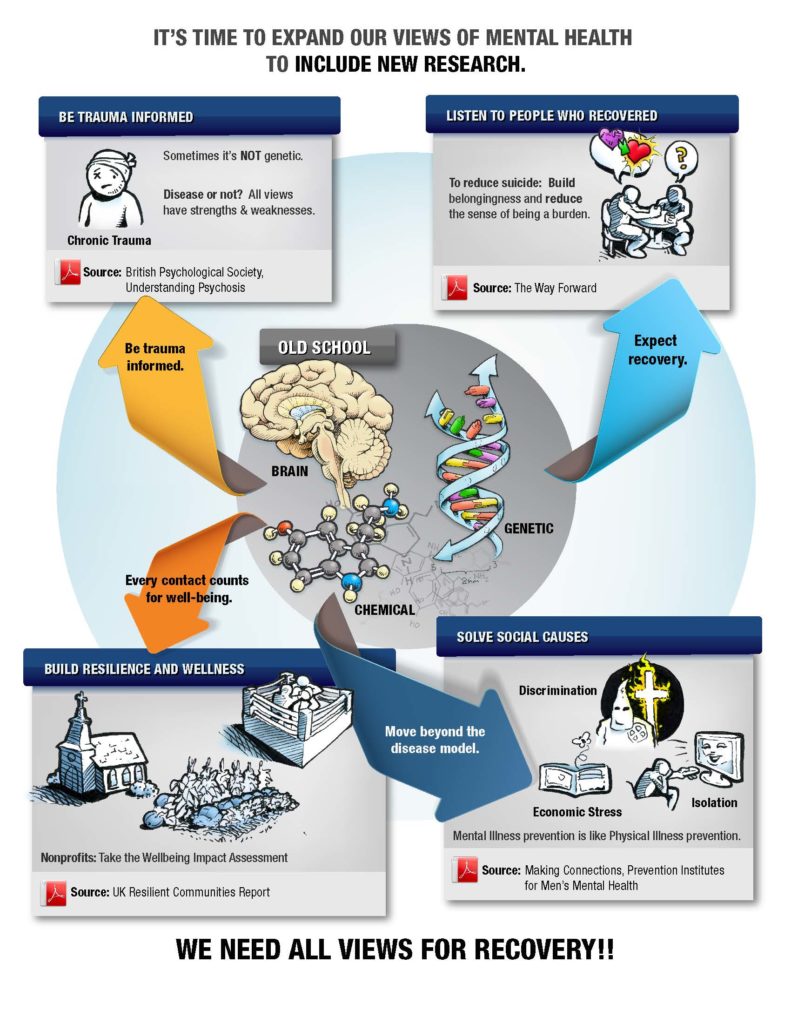
- Does Disease-label Education Increase Confidence in Providing Help: The biggest barriers to help-seeking are fear of labels (32%), negative social judgments (22%), employment discrimination (21%) and stigma (9%). So, education on disease labels will actually REDUCE help-seeking. Another study by Morrison showed that countering the biogenetic model made it easier to provide help. I have started replicating that study with good results in the community. All the disease-label, chemical, genetic stuff makes this a lot more scary. We tell our trainees that everyone goes through hard times, and they already have the answers. We use the infographic below and say the four corners are peer support, dealing with trauma, building wellness stuff, and addressing social causes. All the nonprofits in town already know how to do that stuff. So this is an empowering rather than a disempowering message.
- Increasing mental health: Does Mental Health First Aid increase the mental health of people who go through its program? For one thing, this was assessed using those vignettes/stories about people in crisis, and for another thing, it was about work done in the last four weeks. Both of those are pretty weird definitions of well-being.
So what to do about this? Let’s stop fighting “stigma” and start promoting wellbeing. Let’s increase resilience, but let’s define resilience as well-being, not awareness of trauma biology. Let’s address trauma with concrete action items, not disease mongering. Let’s look at how people can access peer support. Let’s build and promote programs that do these things. Let’s stop disease-mongering in hopes that somehow compassion will increase. (See: Eric Maisel’s list of awesome programs.)
Vote for the Western Mass RLC to get $25,000. Vote with all of your email address. We are making progress. Keep voting for real change. Keep fighting disease mongers!
* * * * *
Share this infographic:















Got got in a good online fight with someone that said that assisted outpatient coerced drugging was good cause the evidence showed less hospitalizations and arrests…
Well of course chemically disabling people so basically all they can do is vegetate in from of the TV getting fat will create evidence that it “helps” people.
I have never lost a argument with a pro psychiatry person online or offline on any MH topic.
Anyone care to try me ? http://www.madinamerica.com/forums/forum/rethinking-psychiatry/
Report comment
And because of that I got booted from most of those websites LOL
Report comment
I absolutely agree, the best way to reduce stigma is to get rid of the scientifically invalid DSM stigmatizations. One does have to wonder how long it will take for this to happen, it strikes me it should have happened back when Insel defunded research into the DSM disorders.
Report comment
Thanks so much for this post, Corinna. It articulates so well what rarely gets stated amidst all the EBP-mania. I like how you’ve used the term disease label education vs. people in distress. The current anti-stigma approach seems like saying people have “cooties” (diagnostic label), and then try to educate to not feel so fearful, avoidant, judgmental about cooties.
The infographic is excellent.
Report comment
I know of at least one innocent person falsely imprisoned for life as the result of an “evidence-based” conviction.
Report comment
Yes, I do not go along with this evidence based movement either, as it gets into an area where there really never can be any evidence.
People forced to live in hostile environments become more and more defensive and rigid in their ways. People in open and accepting environments grow multidimensionally. So that is what we should be working to build.
Those who are being labeled and placed into bad situations, or who’s lives have been effected by such need to organize and start fighting back. This is the way to recover what was lost.
Nomadic
Report comment
How this disease labeling thing is supposed to accomplish anything is beyond me, if something like the DSM-5 is supposed to play an important role. That multitude of disorders in there are nothing but behavioral descriptions, good only for entering as numbers on forms. You might as well just use the numbers on the patients’ forms in lieu of the descriptions, when “educating” them about their alleged illnesses.
It is useful to discuss illnesses if you can quantify the things you could and maybe should do and what you shouldn’t do to help your recovery, but that requires a lot more discrimination than the DSM’s will ever provide and for psychiatrists to get the ability to recognize abnormalities outside the brain that induce “mental ” illnesses and also recognize them in practice.
Report comment
some of all this nonsense about evidence base is about haveing marketable product.
So firms find something to measure that they can use to get money from a funder.
What they measure, as you point out, is not what people suffering mental anguish actually want or find useful.
Hey ho
Report comment
No, the balance sheet once their drug goes into production is the criterion for success for the pharmaceutical company.
Report comment
but also for the service provider.
There are a lot of Mickey Mouse providers out there. I had a freind who worked in drug and alcohol services. He was told to traffic light the clients. Red was ready to go, easy clients who would have got better with a few chats with freinds, orange for more difficult, green for very difficult. The manager said to mainly work with the Red clients as it looked good for the result but have one or two green ones for workers satisfaction.
He had similar stories of other services.
Once the treatments are monitised the neoliberal agenda comes in: assess on dodgy criteria, write glowing report, ask for more funding from commissioner of service, do down competitors, never seriously consult with service users.
Report comment
Hi Corinna,
Decent Recovery abandoning of the Disease Model, and a return to a Full Life for the ‘users’ would mean mass unemployment for the ‘clinicians’.
I also think a Klu Klux Klan type logo could be used to represent ‘mental health’ prejudice.
Report comment
Good post Corinna, keep fighting.
“Evidence-based” is a tired term that needs to be retired. In American mental health settings it has hardly anything to do with getting to know a person in depth, building a therapeutic relationship, focusing on what matters to them, looking at subjectivity and desire, etc. It usually means giving someone a few weeks of CBT (then stopping just when they start to respond) and a psychiatric drug to be continued indefinitely.
By contrast, long-term family and individual interventions outside the disease model have yielded real life-transforming results for people in great distress. But our sorry institutions with their biomedical-dominated viewpoint have lost their souls and cannot remember that loving and understanding people is what heals.
Here below I’m going to copy in a bunch of references I have for truly transformative approaches to people in extreme distress (commonly called “schizophrenia”). These will beat the “evidence-based guidelines” for “treating schizophrenia” anyday. This is one of my posts off the ISPS listserv in which I was trying to help out with some research for the Healing Voices movie:
——————
I have some leads on hopeful data for your researchers:
•The 388 program in Quebec, Canada, has worked with over 250 psychotic young people, most diagnosed with “schizophrenia” and many already having had multiple hospitalizations, over the last 3 decades, in 2-3 times per week psychotherapy with limited drugging, at a residential center. They have excellent results with over 75% of people returning to work and social life. They record their data, since they receive government funding and need to justify their work, but have not formally published it. Their leader is Lucie Cantin; have a look at the website http://www.gifric.com/388.htm . They work in French so if you speak to them you may need a translator (I interviewed her myself on Skype). Here’s a talk by another director there, Danielle Bergeron, with subtitles describing the program: https://www.youtube.com/watch?v=mmqT-4W4Cvg
•Bent Rosenbaum has a 2012 study showing that two years of psychotherapy produced significantly better social and work functioning than drugs alone. Thep paper is “Supportive Psychodynamic Psychotherapy versus Treatment as Usual for First Episode Psychosis”. It was a randomized study of about 150+ people in Denmark. Here it is – https://www.researchgate.net/publication/278033241_Supportive_Psychodynamic_Psychotherapy_versus_Treatment_as_Usual_for_First-Episode_Psychosis_Two-Year_Outcome
•The largest study I know of is William Gottdiener’s 2002 meta-analysis of psychotherapy for schizophrenia – the one that contains pooled data on 37 studies of outcome for people diagnosed schizophrenia and given psychotherapy. The 37 studies include 2,642 people, given psychotherapy an average of 1.5 times a week for an average of 20 months (across all studies). 19 of the studies are randomized and 18 non-randomized. The data consistently show that getting psychotherapeutic help is associated with significant improvements in functioning for people diagnosed schizophrenic. In one way the meta-analysis considers the data, the effect size is such that about two-thirds of those getting the therapy significantly improve their functioning, whereas only one-third of those without improve. Interestingly, the meta-analysis finds that getting drugs in addition to psychotherapy yields no additional improvement beyond psychotherapy alone. So Gottdiener notes that his results are an argument for offering social support without drugs, counter to the wisdom of the time. This paper is available for free on psychrights.org ( http://psychrights.org/Research/Digest/Effective/BGSchizophreniaMeta-Analysis.htm ), or I have it. Many of the individual 37 studies in Gottdiener’s meta-analysis are worth reading in their own right; they include a few of the other papers listed here.
•Lewis Madrona’ 2014 paper, “Results of a Transpersonal, Narrative, and Phenomenological Psychotherapy for Psychosis”, lists results of psychotherapy given by his therapy group to 51 psychotic people for an average of 2.5 years. The results are very impressive with 80% plus of the group, mostly being labeled bipolar or schizophrenic initially, having good functional outcomes, working/volunteering, without continued use of antipsychotics. I spoke to Madrona on the phone to find out some background data I’m quoting here. In the actual study Madrona tracks the decreases on the PANSS, HAM, BPRS, and other scales. This is a non-randomized study but the within group improvement is very impressive. The problem in this study was that the majority of the beginning group (who are not included in these results) had to drop out due to family interference, the effects of already being on strong drugs for a long time, or lack of money. This was less an issue in other studies, especially more holistic programs like Open Dialogue, 388, and the Psychosis Therapy Project. Here it is – http://www.transpersonalstudies.org/ImagesRepository/ijts/Downloads/IJTS_33-1-07_pp_57-76_Mehl-Madrona_et_al_2014_Results_of_a_Transpersonal_Narrative_and_Phenomenological_Psychotherapy_for_Psychosis.pdf
•
•Roberta Siani and Orazio Siciliani have an impressive randomized study of intensive psychtherapy for schizophrenic clients, reviewed in the book Psychosis -Psychological Approaches and Their Effectivness by Martindale. The outcomes for about 50 clients, (only a subset of whom were labeled “schizophrenic”, some were “borderline” or another serious diagnosis,) are tracked on several psychological-functioning scales over a two year period in which the people received over 100 therapy sessions. It is a randomized study and the differences are clear. The schizophrenic people getting therapy improve enough that they are diagnostically in a range between borderline and neurotic functioning (according to the psychodynamic model of the authors), with a lot of improvement in ability to have intimate relationships. Here is the book which is available for as low as $3 used – http://www.amazon.com/gp/product/1901242498/sr=8-3/qid=1461679604
•Dorothy Bonigal-Katz runs the Psychosis Therapy Project out of Islington Mind, London. They have not published formal data yet, but it is an example of an innovative project where psychotic people (about 45 are in the program getting therapy at any one time) can get low cost psychotherapy and not be forced to take drugs. They do have data showing clients are very satisfied with the approach, which is usually 1-2x per week psychoanalytic psychotherapy. Here is their site – http://www.islingtonmind.org.uk/psychosis-therapy-project.asp#.Vx92j4-cF9A
•If enough time I would recommend interviewing one or more of the following: Lloyd Ross (New Jersey), Bert Karon (Michigan), Gustav Schulman (Finland), Gary Van den Bos (US, Washington DC), Brian Koehler (New York), Ira Steinman (San Francisco), Riccardo Lombardi (Rome, Italy). These authors each have much experience with intensive psychotherapy of psychosis, including in many cases without using drugs much or at all. For example, the former APA publisher and psychodynamic therapist Gary Van den Bos has kept case notes and recorded (unpublished) outcome data for over 100 schizophrenic people he treated over his 40 year career, with about 80% of those who stayed for at least one year recovering the ability to function, and in many cases becoming essentially normal and not symptomatic, according to Van den Bos. Again this data is not formally published, but formally published papers don’t have a monopoly on what is real or valid information (and may in fact be less valid than information given by people who are not subject to the pressures and distorting influences of the academic processing process). Most of these authors’ contact information is available on isps.org or via searching the internet.
•The NIPS program in Scandinavia had some good results for psychotherapy of psychosis. Brian Koehler has this data; I have not been able to locate it yet (and Hi Brian, I still want to get it!). Also the Need Adapted approach of Alanen, which was a precursor to Open Dialogue in Scandinavia, had some good data… you might look into the ISPS book series for that, or this book – http://www.amazon.com/Schizophrenia-Its-Origins-Need-Adapted-Treatment/dp/1855751569/
•
•British CBT for psychosis also has some good data. Their results are surveyed in several randomized studies of psychotherapy versus drugs only for psychosis given for periods of up to 1 year by Kuipers, Tarrier, Drury, and Kingdon in the book Psychosis: Psychological Interventions and their Effectiveness, by Martindale, linked above.
•for older studies, there are two impressive ones: Barbro Sandin’s work with 14 men labeled schizophrenic, surveyed in the studies “Effects of Psychotherapy in Schizophrenia: A Retrospective Study” by Sjostrom (1985) and “Fully Recovered Schizophrenic Patients who Received Intensive Psychotherapy” by Cullberg (1991). These papers are older but still valid. I have both papers. The initially psychotic men given therapy were tracked for 6-8 years after intake and were functioning and feeling far better than men given drugs only. Here are links to the abstracts – http://onlinelibrary.wiley.com/doi/10.1111/j.1600-0447.1985.tb05065.x/abstract
and https://www.researchgate.net/publication/232051046_Fully_recovered_schizophrenic_patients_who_received_intensive_psychotherapy_A_Swedish_case-finding_study
•If you want to get these papers for free just ask me (email – bpdtransformation (at) gmail (dot) com), and to people on this list don’t tell the Feds that I am passing them around behind the journals’ backs 🙂
•Lastly there is Benedetti’s chapter in his book Psychotherapy of Schizophrenia, “Individual Psychotherapy for Schizophrenia.” This is where Benedetti surveys the results of 50 psychotic people treated an average of 3x per week for an average of five years. The results were excellent with over 80% of the group functioning well, having good relationships, and “often leading to complete healing”, according to Benedetti. This paper is not online; I have the book which is available used on Amazon for cheap. Here is a link to an older version of the book which is cheaper used – http://www.amazon.com/Psychotherapy-Schizophrenia-Gaetano-Benedetti/dp/0814710875/ – and another book by the same author surveying some other valuable data – http://www.amazon.com/Psychotherapy-Schizophrenia-Effective-Approaches-Controversies-Recommendations/dp/088937077X/
•There are some other good Italian family therapy studies but I am not sure which they are. Maybe some others on the list can help with that.
•Your researchers know about Open Dialogue, I would only tell them to emphasize that the excellent results in that approach were achieved over 3 separate Finnish cohorts (from about 1993 to 2005) and thus “replicated” at least for that geographic area. The issue now is obviously to have similar results in different locations, and with several major efforts underway to try out OD in different countries (see the recent article in MIA “Love is Dialogical” by Kermit Cole) that will hopefully happen.
I hope this helps your researchers. I would even suggest they could list many of these resources in a bibliography so that more professionals and laypeople could become aware of the hope that is out there. If they have some links to further reading, I would further recommend including the following books: Rethinking Madness by Paris Williams and Treating the Untreatable by Ira Steinman for laypeople. And for professionals, Weathering the Storms by Murray Jackson and The Infantile Psychotic Self by Vamik Volkan. Find these books used for cheap on Amazon.
Lastly, Brian Koehler recently posted on the listserv about his research showing that the neurobiology of schizophrena is really the neurobiology of chronic isolation, fear, loneliness, stress, and trauma. I recommend strongly highlighting this link… it is hopeful as these realities, while sad, are modifiable and healable, unlike a chronic brain disease. Brain Koehler has some formal academic writing about this so maybe he can share that with your researchers.
Report comment
I think it is about the money and neoliberalsim. Turn things over to the market, have service providers compete for money to provide a service, have dodgy outcome measures that justify the money, do not actually look at what works or help workers support each other or really listen to clients.
This happens in all privitised services; education, transport, housing power, water etc etc.
Report comment
Yes, I agree. America is the epicenter of poor “mental health” practices because of its capitalistic profit-focused obsession. Another factor is that severely distressed people are rarely able to fight back or speak up when or after the money is being made. In the other sectors you mention, I think poor/minority/abused/in crisis people are not overrepresented so much. People in serious distress, physically or mentally, are thus a particularly ripe target for profit-seeking corporations.
Report comment
Hi BPD, John,
What you really want is to have young people up and functioning again and the medication dependent system doesn’t achieve this. It might be hard otherwise at the start – but so what.
Report comment
Yes I agree. Like many things in American culture, our “mental health system” results in short-term “gains” (of billions of dollars of profit annually for drug companies from drugging young people) and long-term losses (of millions of young people unable to function who cost society hundreds of billions in disability payments over decades).
Report comment
I really enjoyed this piece – very neatly explained!
Report comment
Great article. I totally agree that good outcomes have different definitions. The drug industry standard of taking drugs regularly ( a chemical lobotomy) is NOT in my definition of a good outcome. That would be a living death, and if you are not perfect, many are not perfect, an emotional outburst can force ( court order) people to be poisoned (medicated) for the rest of their life. A “normal” person can make a mistake and be punished in civil court or criminal court, a person with a history of mental illness needs “medication” for his/her mistakes. ( for the rest of their life). We are HELPING people! . right. not.
Report comment