As the schizophrenia/psychosis recovery research continues to emerge, we discover increasing evidence that psychosis is not caused by a disease of the brain, but perhaps may best be described as a last ditch strategy of a desperate psyche to transcend an intolerable situation or dilemma. To better understand how this understanding which is so contrary to the widespread understanding of psychosis has emerged, it will help if we break this discussion into two parts: (1) a summary of the research associated with the “brain disease theory” of schizophrenia/psychosis; and (2) a summary of the research that has given rise to this alternative understanding.
Part One: Taking a Closer Look at the Brain Disease Theory
In spite of over a hundred years of research and many billions of dollars spent, we still have no clear evidence that schizophrenia and other related psychotic disorders are the result of a diseased brain. Considering the famous PET scan and MRI scan images of “schizophrenic” brains and the regular press releases of the latest discoveries of one particular abnormal brain feature or another, this statement is likely to come as a surprise to some, and disregarded as absurdity by others. And yet, anyone who takes a close look at the actual research will simply not be able to honestly say otherwise. And not only does the brain disease theory remain unsubstantiated, it has been directly countered by very robust findings within the recovery research, it has demonstrated itself to be particularly harmful to those so diagnosed (often leading to a self-fulfilling prophecy), and it is highly profitable to the pharmaceutical and psychiatric industries (which likely plays a major role in why it has remained so deeply entrenched in society for so many years, in spite of our inability to validate it).
Deconstructing the Myths of Madness
The claim I am making here clearly runs counter to the mainstream understanding of schizophrenia, but we find that it’s a relatively straightforward task to back up this claim. We simply need to take the time to extract the actual research findings from the unsubstantiated assumptions and propaganda that are so often used to back up the brain disease theory. I’ll go through the most prevalent of these here:
Hypothesis #1: Schizophrenia is caused by a biochemical imbalance within the brain
This theory originated from the observation that drugs which block the transmission of the neurotransmitter dopamine within the brain (so called “antipsychotics,” originally referred to as “major tranquilizers”) appear to reduce the symptoms of schizophrenia. The reasoning behind the origin of this hypothesis was, since schizophrenic symptoms are reduced when dopamine transmission is suppressed, then perhaps schizophrenia is caused by excessive dopamine within the brain.
This hypothesis originally appeared quite plausible; however, it has since been seriously discredited:
First, although it is known that an individual’s dopamine receptors (the type of receptors most affected by antipsychotic drugs) are completely blocked within hours of consuming a sufficient dose of an antipsychotic drug, the actual antipsychotic effects often do not become apparent for up to several weeks (although a significant degree of apathy towards one’s psychotic experiences often does kick in quickly, as would be expected with any kind of tranquilizer; Bentall, 2004). If psychotic symptoms are the direct result of too much dopamine, then why don’t we see a more immediate abatement of these symptoms as soon as the dopamine levels have been effectively reduced?
Second, with the introduction of PET and MRI scans, the dopamine hypothesis was apparently substantiated when it was recognized that many “schizophrenic” brains do indeed seem to be set up to transmit excessive dopamine. However, it was eventually realized that the vast majority of brains studied had been exposed to long-term antipsychotic drugs, and it’s since been established that the effects of these drugs alone may very well account for these anomalies (Burt, Creese, & Snyder, 1977; Kornhuber et al., 1989; Mackay, 1982).
Finally, even many of the proponents of this theory have been forced to acknowledge that we still have not found any clear biochemical imbalance that we can associate consistently with schizophrenia or any of the “mental illness” diagnoses, and that all we can really say for sure is that psychiatric drugs themselves do lead to the development of a biochemical imbalance in one’s brain (Hyman & Nestler, 1996; Whitaker, 2002).
Hypothesis #2: Schizophrenia is caused by anomalous brain structures
This hypothesis essentially states that schizophrenia is a disease caused by something wrong with the actual structure of one’s brain, specifically with regard to the relative size of the cerebral cortex and/or other nearby regions of the brain. This hypothesis is generally supported by the actual findings of such anomalies of the brains of those so diagnosed. But again, upon closer inspection of the research, we find an empty hypothesis that quickly crumbles away:
First, we have discovered that there are many different factors that can lead to these abnormalities, including: depression, alcoholism, early childhood trauma (Read, 2004), water retention, pregnancy (Woodruff & Lewis, 1996), advancing age, variations in educational achievement, social class, ethnicity, and head size (Bentall, 2004). It was also discovered that the sizes of these regions of the brain can fluctuate quite rapidly within even healthy individuals, leading to varying results even within the same individual (Bentall, 2004). And once again, what do you imagine we have found that is probably the most relevant factor causing such anomalies in the brain? You guessed it… the use of antipsychotic drugs themselves. And virtually all of the research that has discovered such brain anomalies in those diagnosed with schizophrenia did not account for this very important factor, meaning that once again, most of the brains studied had most likely been adversely affected by the long-term use of antipsychotic drugs (Read, 2004; Siebert, 1999).
A second serious challenge to the validity of the abnormal brain structure hypothesis came when it was recognized that the majority of those diagnosed with schizophrenia do not show any obvious brain abnormality at all. Lewine found that “there is no brain abnormality in schizophrenia that characterizes more than 20-33% of any given sample. The brains of the majority of individuals with schizophrenia are normal as far as researchers can tell at present [emphasis added]” (Lewine, 1998, p. 499); and this in spite of the fact that most of these participants were likely exposed to other brain changing factors such as trauma and/or antipsychotic medications. Conversely, it is common to find healthy individuals who have no schizophrenic symptoms at all and yet have brain abnormalities similar to those sometimes found in schizophrenics (Siebert, 1999).
Hypothesis #3: Schizophrenia is a Genetic Disorder
This hypothesis is in close alignment with the two brain disease hypotheses mentioned above and suggests that this brain disease is transmitted genetically. But again we find some serious problems with the assumptions that have given rise to this hypothesis:
This hypothesis is based on a small handful of twin and adoption studies (Joseph, 2004) conducted many decades ago which, even when we ignore the many serious methodological flaws with these studies, the only conclusion that can actually be drawn from them is that there may be a hereditary component in one’s susceptibility to developing psychosis. However, this is not any different than the findings that there may be a hereditary component in intelligence, shyness, and other psychological characteristics that clearly are not indicative of any kind of physiological disease.
In other words, it’s an illogical leap to assume that a hereditary predisposition for a psychological trait or experience must imply biological disease. Yes, there does seem to be some evidence that some of us may be born with a temperament or other psychological characteristics which make us more vulnerable to experiencing psychosis at some point in our life; but no, this evidence does not lend any validity to the hypothesis that schizophrenia is a genetically transmitted biological disease.
Another important area of research discrediting the “genetic disease” hypothesis is the far more substantial research showing high correlations with environmental (non-hereditary) factors and the development of psychosis/schizophrenia. For example, One study looked at 524 child guidance clinic attendees over 30 years and discovered that 35% of those later diagnosed with schizophrenia had been removed from their homes due to neglect, a percentage twice as high as that for any other diagnostic category (Robins, 1974); another study found that 46% of women hospitalized for psychosis had been victims of incest (Beck & van der Kolk, 1987); another study of child inpatients found that 77% of those who had been sexually abused were diagnosed psychotic compared to only 10% of those who had not been so abused (Livingston, 1987); and yet another study found that 83% of men and women who were diagnosed with schizophrenia had suffered significant childhood sexual abuse, childhood physical abuse, and/or emotional neglect (Honig, Romme, Ensink, Escher, Pennings, & de Vries, 1998). Bertram Karon, researcher and acclaimed psychosis psychotherapist, has found evidence of a high correlation between the experience of intense feelings of loneliness and terror within childhood and the later onset of schizophrenia, a finding that is clearly closely related to the findings of these other studies (Karon, 2003).
Even the strongest proponents of the brain disease hypothesis acknowledge that it has not yet been validated
The National Institute of Mental Health, on its Schizophrenia home page, proclaims confidently that “schizophrenia is a chronic, severe, and disabling brain disorder” (NIMH, 2010a, Para. 1), a statement you find on nearly every major page or publication they have put out on the topic; and yet if you spend a little more time looking through their literature, you will find that they admit that “the causes of schizophrenia are still unknown” (NIMH, 2010b, Para. 1). Similarly, the American Psychiatric Association also confidently proclaims that “schizophrenia is a chronic brain disorder” (APA, 2010, Para. 1), but then they acknowledge on the very same page that “scientists do not yet know which factors produce the illness” (APA, 2010, Para. 10), and that “the origin of schizophrenia has not been identified” (APA, 2010, Para. 1). The strong bias towards the brain disease theory is clearly evident in the literature of these and other similar organizations, and yet the message comes through loud and clear that we still do not know the cause of schizophrenia. Even the U.S. Surgeon General began his report on the etiology of schizophrenia with the words, “The cause of schizophrenia has not yet been determined” (Satcher, 1999, Para. 1). It would appear, then, that it is simply not appropriate to claim with such confidence that schizophrenia is the result of a brain disease.
If schizophrenia really is a brain disease, then how do we account for the relatively high rates of full recovery from it?
One finding within the recovery research that is extremely robust is that many people experience full and lasting recovery after having been diagnosed with schizophrenia. We see this evidence in the vast majority of the longitudinal recovery studies (See Chapter 4 in my book, Rethinking Madness, for a complete list of all major longitudinal studies), including those conducted by the National Institute of Mental Health (Harrow & Jobe, 2007; Harrow, Jobe, & Faull, 2012) and the World Health Organization (Hopper et al., 2007). There is evidence of spontaneous recovery in between 5% and 71% of cases, depending upon the country of origin and other factors, and even as high as 82% with certain psychosocial interventions (Mosher, 1999; Seikkula, Aaltonen, Alakare, Haarakangas, Keränen & Lehtinen, 2006). It is illuminating to compare the high recovery rate for schizophrenia with the recovery rate for well-established diseases of the brain such as Parkinson’s, Alzheimer’s, Hungtington’s, or Multiple Sclerosis, in which there is no well documented evidence of even a single individual making a full recovery from any of these (Siebert, 1999). Furthermore, we see evidence that many of those who have experienced full recoveries from schizophrenia and other related psychotic disorders do not just return to their pre-psychotic condition, but experience profound healing and positive growth beyond the condition that existed prior to their psychosis, again in stark contrast to the well established diseases of the brain (Williams, 2011, 2012).
The mainstream paradigm of care may actually be creating a self-fulfilling prophecy of brain disease
While we continue to have no solid evidence that schizophrenia/psychosis is the manifestation of a diseased brain, we do discover one particularly tragic irony in that our very entrenched belief in this theory and the paradigm of care that has resulted from it is actually ensuring that enormous numbers of people actually do develop brain disease (see Figure 1).
.
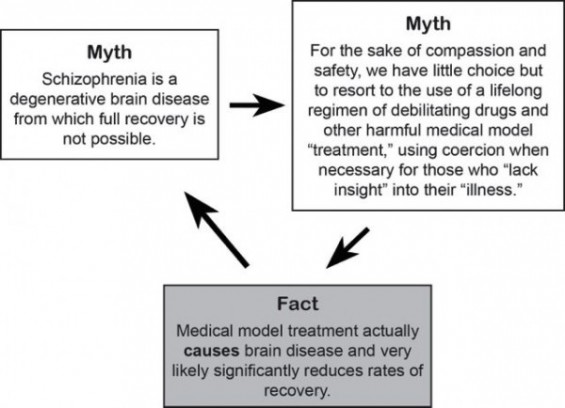
Figure 1. A vicious circle caused by the brain disease theory of schizophrenia
Isn’t it time, then, that we finally let go of the brain disease theory?
In summary, then, we find that in spite of well over a hundred years of research and billions of dollars spent, the brain disease theory remains entirely unsubstantiated; and that our persistent yet unfounded faith in this theory may very well be generally causing much more harm than benefit (or at least causing significant harm to those so diagnosed at the cost of great financial benefit to certain key players within the current mental health care establishment).
Part Two: Towards an Alternative Understanding of Schizophrenia/Psychosis
So, if schizophrenia/psychosis is not caused by a disease of the brain, then what does cause it? This is not a simple question, and it’s further complicated by the fact that there continues to be widespread controversy over whether or not the concept of “schizophrenia” as it is currently used is even a valid construct, an issue that needs to be addressed first before suggesting an alternative model for understanding schizophrenia and the other related psychotic disorders.
Moving from discrete “mental illnesses” to a continuum of experience
The debate about the validity of the concept of “schizophrenia” arises from recent research suggesting that (1) all of the various major psychotic disorders may simply be variations of one phenomenon, and (2) there may be not be distinct boundaries between psychosis itself and what we think of as sanity. The British Psychological Society (the BPS, Great Britain’s counterpart to the American Psychological Association), in its official report summarizing their understanding of “mental illness” and “psychotic experiences,” concluded that the various psychotic disorders may more appropriately be classified as variations of one phenomenon, a phenomenon that many have suggested we refer to simply as psychosis or madness.
Taking this conclusion one step further, the BPS suggested that “mental health and ‘mental illness’ . . . shade into each other and are not separate categories” (2000, p. 17). In other words, they suggest that not only are the various psychotic disorders best understood as merely representing different points along a continuum of a single phenomenon (see Figure 2), but that sanity and madness themselves are also best understood as being merely different points along a single continuum (see Figure 3). They cite evidence suggesting that psychotic experiences are merely extreme expressions of more ordinary traits found within the general population.
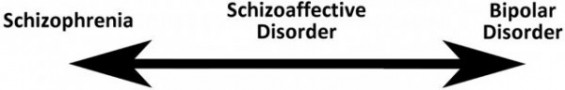
Figure 2. Seeing the major psychotic disorders as lying on a common continuum.
When psychotic experiences contain primarily cognitive features (so called delusions and hallucinations), a person is most likely to be diagnosed with schizophrenia; when affective instability predominates, a person is most likely to be diagnosed with bipolar disorder; and when a person experiences a significant combination of both of these, they are most likely to be diagnosed with schizoaffective disorder.
Based upon the findings of my own research and my review of the other relevant research, I’ve come to the conclusion that it can be helpful to see the “sanity/madness” continuum as being defined by essentially two factors: (1) the degree of resonance or dissonance of one’s experiences with consensus reality (where consensus reality is defined as the understanding of reality that is generally agreed upon as being the most legitimate within a given individuals’ society); and (2) for those having experiences that differ significantly from consensus reality (let’s call them anomalous experiences), the degree of distress, limitation, and/or instability that is associated with these experiences. With these two factors in mind, then, we can divide the sanity/madness continuum into four separate categories of experience, keeping in mind that these don’t represent discrete categories but merely act as place markers along a common continuum of experience; see Figure 3).
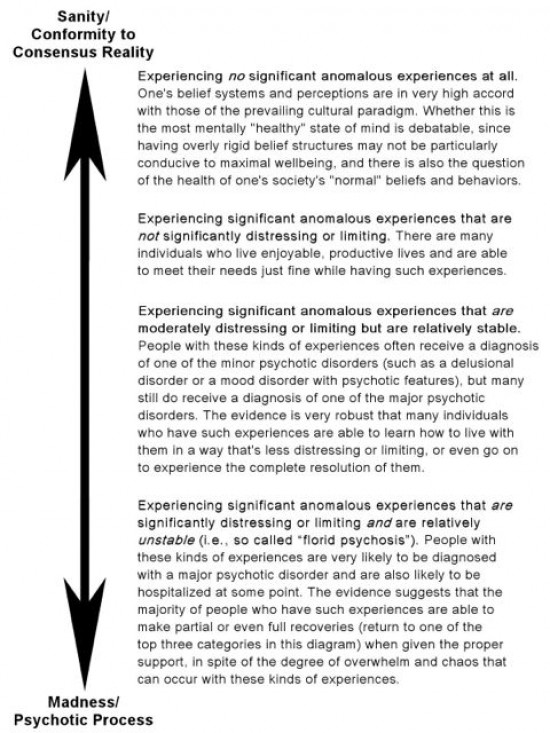
Figure 3. The “Sanity/Madness Continuum.”
By considering anomalous experiences from a continuum perspective, we arrive at some very different implications regarding how to best define such experiences and what is the best way to support those who experience them:
First, we recognize that the line between so called “sanity” and so called “madness” is somewhat arbitrary—that it’s not helpful and probably not possible to pinpoint any discrete “illnesses” along this continuum.
Second, we recognize that the problems associated with anomalous experiences are probably not due so much to the fact that they deviate from consensus reality, but rather are more likely due to the difficult relationship an individual may have with these experiences (e.g., distress caused by hearing persecutory voices or holding persecutory beliefs, along with unusual or even harmful behavior that may arise in someone’s attempts to deal with them). One implication of this is that it’s important to distinguish between those anomalous experiences that cause distress or limitation, and those that don’t. If they’re not causing any problems, then what’s the problem? Why call it psychosis? Considering these kinds of experiences to be “psychotic” or giving them a name such as “schizophrenia” or “delusional disorder” appears to be unhelpful and likely even harmful, especially if such individuals are inculcated into the unfounded belief that these are the manifestations of a diseased brain.
A second important implication of this idea is that, when these kinds of experiences do cause distress or limitation, it’s likely that the best support we can offer does not consist of trying to bring the individual’s experience back into alignment with consensus reality, but instead consists of helping them meet their needs from within the context of their own experiences. The literature is filled with research and biographical accounts supporting this idea (for example, Chadwick, Birchwood, & Trower, 1999; Romme et al, 2009).
Finally, as an individual’s experience does move further down the continuum into the realm represented by the two categories listed at the bottom of Figure 3, evidence from my own research (Williams, 2011, 2012) as well as that of other recovery research (e.g., Arieti, 1978; House, 2001; Karon & VandenBos, 1996; Laing, 1967; May, 1977; Mindell, 2008; Nixon et al, 2009, 2010; Perry, 1999) suggests that they may be entering a powerful psychological process entailing the transformation of their self and their personal paradigm at a very profound level (more on this shortly). This is the process that often gets equated with “florid psychosis” and is typically the hallmark condition that so often gets labeled as “schizophrenia” or as one of the other major psychotic disorders.
Since the term “schizophrenia” is so heavily laden with unfounded assumptions, as we’ve been discussing, I’ll simply refer to this process as “the psychotic process” or “psychosis” in order to maintain some congruence with the terminology already used within the field (while acknowledging that the term “psychosis” also comes heavily laden with problematic assumptions). After all, we can say that the condition that so often gets labeled as “schizophrenia” (or one of the other major psychotic disorders, depending upon the specific nature of the anomalous experiences) is essentially just long term psychosis.
So, what causes psychosis?
Returning, then, to the question of what causes psychosis, I’ll preface my discussion of this question hereby saying that I’ve devoted an entire book (Rethinking Madness—Williams, 2012) to a thorough exploration of this question, so unfortunately, it’s just not possible to adequately summarize and back up a thorough answer to this question within such a brief article. What I will attempt to do here, however, is to put forth the most essential concepts of this alternative understanding and hopefully encourage others to engage in fruitful discussion about this important topic.
While I don’t believe it’s a stretch to say that our attempt to validate the brain disease theory of these disorders has so far been a colossal failure, there is a very different line of research that I believe has had much more success in providing significant clues as to the cause of these vexing disorders. The line of research I’m referring to is the research that has inquired directly into the actual lived experiences of those who have personally experienced psychosis.My own recent research is particularly relevant in this regard, which includes a series of three studies inquiring deeply into the experiences of those who have experienced full and lasting recovery from long term psychosis (Williams, 2011, 2012).
I have found that the findings of this line of research have converged sharply upon a fundamental cause of these psychotic disorders that is perhaps best stated something like this: The individual we deem “schizophrenic” or “psychotic” is merely caught in a profound wrestling match with the very same core existential dilemmas with which we all must struggle. In other words, it appears likely that psychosis is not caused by a disease of the brain but is rather the manifestation of a mind deeply entangled within the fundamental dilemmas of existence.
So, what are these existential dilemmas?
The term “existential dilemma” essentially refers to the dilemmas inherent in finding ourselves in a state of existence—“Here I am, alive, conscious, and feeling. Now what?” These dilemmas, at their core, relate to our need to maintain our existence, and perhaps even more importantly, our need to create a life that is worth living—where the joys and rewards of living are strong enough to overcome the inherent pain and suffering of life and provide us with the will to go on living. Some of the most pertinent such dilemmas that have been named by various existential thinkers are: finding a balance between love/belonging and authenticity/autonomy; finding a balance between freedom and security; coming to terms with the fact that all of our decisions and actions come at some cost; coming to terms with our own impending death; and cultivating enough meaning in our lives so that we are able to rise out of bed every morning and greet each new day.
In virtually all of the research and case studies I have come across that have looked closely at the actual subjective experiences of those who have fallen into a psychotic process, we see evidence that, prior to the onset of psychosis, these individuals had found themselves in overwhelming existential dilemmas similar to those mentioned above, but to a far greater degree than that which the average person ordinarily experiences. In one of the most well-known such studies, R. D. Laing, a Scottish psychiatrist renowned for his pioneering research on schizophrenia and his clinical work with those so diagnosed, closely studied the social circumstances surrounding over 100 cases of individuals diagnosed with schizophrenia, and he concluded that “without exception the experience and behavior that gets labeled schizophrenic is a special strategy that a person invents in order to live in an unlivable situation [author’s emphases]” (1967, pp. 114-115).
Bertram Karon, one of the world’s most renowned clinicians specializing in psychotherapy for those diagnosed with psychotic disorders, stated his belief that any one of us would also likely experience psychosis if we were to have to live through the same set of circumstances as those of his psychotic clients (Karon & VandenBos, 1996). We see other evidence of this again and again in the plethora of biographical and autobiographical accounts that have been written and filmed (for example, Bassman, 2007; Beers, 1981; Dorman, 2003; Greenberg, 1964; Modrow, 2003).
The focus of my own research (Williams, 2011, 2012) was to explore the change that takes place with regard to one’s experience and understanding of the world and one’s self (one’s personal paradigm) throughout the entire psychotic process, from onset to full recovery. The findings that emerged with regard to the onset of psychosis were very much in alignment with the findings of the other research mentioned above—there is clear evidence that every participant in all three of my own studies had also experienced such an overwhelming dilemma prior to the onset of psychosis. After thorough analysis of the data in the final and most comprehensive of the three studies, I arrived at the conclusion that there were essentially two fundamental dilemmas that appeared to lie at the crux of both the onset and resolution of these participants’ psychotic process:
The need to achieve a sustainable balance between autonomy (personal choice/personal freedom/authenticity) and connection (love/belonging/acceptance)
The need to maintain a relatively secure and stable sense of self when the very fabric of one’s being and indeed of the entire universe is profoundly groundless, impermanent, and interconnected.
What is particularly interesting about these dilemmas is that they may be the very same dilemmas that lie at the core of all human experience, regardless of one’s degree of sanity or lack thereof. It’s likely that most of us can easily relate to the first dilemma—we only need to think of the various challenges we’ve had in our relationships with family members, partners, and other loved ones. We can also easily witness this dilemma occurring within toddlers as they struggle to find a balance between the drive to explore the world and assert their autonomy while still wanting to be unconditionally loved and accepted by their caretakers. And of course this dilemma never fully goes away for most of us.
The second dilemma mentioned above is probably a little more difficult for some of us to relate to, especially for us Westerners (many practitioners of some of the Eastern traditions such as Buddhism, Taoism, and Advaita Vedanta have thoroughly explored this dilemma). This dilemma generally lies a little more deeply beneath our conscious awareness than the first dilemma, though it often becomes conscious in unusual circumstances, such as during psychological/emotional crisis, intensive contemplative practice (such as mindfulness meditation), and hallucinogenic drug use.
So, if these existential dilemmas are universal, then why do some individuals become more overwhelmed by them than others, and go on to develop psychosis?
The research suggests that there are two main factors that may make someone vulnerable to experiencing one or both of these dilemmas to a very high degree:
With regard to being overwhelmed by the first existential dilemma (that of finding a tolerable balance between autonomy and relationship), developmental and/or acute trauma appears to play a particularly strong role. It has long been established in the field of developmental psychology that healthy childhood development requires that we find a healthy balance between our sense of autonomy and our trust that we are loved and accepted by others.
Attachment research has been exploring and validating this idea for decades. Childhood abuse (physical, sexual, and/or emotional), trauma, neglect, and a poor fit between the temperament of a child and her/his caretaker(s) all clearly interfere with establishing a healthy balance in this regard, and all of these are well established in predisposing someone to developing serious emotional and psychological problems, and in more extreme cases, psychosis (Karen, 1994; Mahler, Pine, & Bergman, 1973; Rathus, 2006; Schore, 2002; Slade, 1999; Wallin, 2007; Williams, 2011, 2012).
Recall that the second existential dilemma refers to our need to maintain the sense that we are a relatively secure and stable self living in a relatively secure and stable world, when the reality of our situation is very different than this. To better understand how someone can be overwhelmed by this dilemma, it will help to first touch on the concept of cognitive constructs. The term cognitive constructs refers to the belief systems and interpretations that each of us has constructed throughout our lives which allow us to make sense of the world.
They can act somewhat like a double edged sword for us. On one hand, they provide us with the means to distinguish one object or being from another, and they give us the general sense that we “kinda know what’s going on” so that we can meet our needs and navigate our way through life. They also give us a sense that there is some solid ground beneath our experience—in other words, that we are a secure and stable self living in a relatively secure and stable world. But on the other hand, our cognitive constructs can close our minds to other perspectives, and they create the illusion that the world and our self are much more stable and secure than they actually are.
For most of us, our cognitive constructs are fairly solid, changing only slowly over time. However, in certain cases, such as during acute crisis or trauma, or with the use of certain psychoactive drugs, one’s cognitive constructs can become highly unstable. On one hand, this can lead to the potential benefit of having a more open mind (less rigid belief systems) and the richness of experiencing a greater sense of interconnectedness with all (more about this in my book, Rethinking Madness); but on the other hand, the loosening of our cognitive constructs can also lead to the potential terror of experiencing just how precarious and ungrounded our existence and self really are, which can lead to profound shifts within our personal paradigm as we desperately attempt to find some “solid ground” to cling onto once again. Such radical personal paradigm shifting is closely associated with anomalous experiences—so called delusions and hallucinations—experiences that are generally equated with psychosis.
Why some people are more prone to the loosening of one’s cognitive constructs is still somewhat mysterious—it appears that certain drugs and psychological or physiological distress may play a significant role, and some individuals may even have some genetic or developmental predisposition for such experiences. However, even though some people may be more prone to the destabilization of their cognitive constructs, it seems likely that virtually anyone has the potential to experience this if exposed to an overwhelming dilemma, situation, or trauma. It’s all too easy to find cases of extreme neglect, abuse, torture, or other trauma that have profoundly shaken up one’s experience of one’s self and the world and led to psychosis or at least psychotic-type experiences (those within the bottom three categories of Figure 3 above).
The research suggests, then, that both of these factors play an important role in the development of psychosis—an overwhelming existential dilemma and unstable cognitive constructs. The research also suggests that these two factors are very closely related, in that the experience of such an overwhelming dilemma makes one more susceptible to experiencing unstable cognitive constructs, and vice versa. It’s also important to emphasize that it is the individual’s own subjective experience of their situation that is most relevant. Sometimes, it’s easily evident to an observer that an individual is experiencing such an overwhelming dilemma (again, think of overt trauma, abuse, torture, etc.); but at other times, the individual’s crisis is not so apparent to an onlooker, though it is often all too apparent to the individual her/himself.
So, we finally arrive at the final and perhaps most important question in this discussion: “Why would an individual’s psyche intentionally initiate psychosis?”
In other words, how can something as chaotic and as potentially harmful as psychosis act as a strategy to aid someone in transcending an otherwise irresolvable dilemma? To understand this, it helps to use as a metaphor the process of metamorphosis that takes place within the development of a butterfly. In order for a poorly resourced larva to transform into the much more highly resourced butterfly, it must first disintegrate at a very profound level, its entire physical structure becoming little more than amorphous fluid, before it can reintegrate into the fully developed and much more resourced form of a butterfly.
In a similar way, when someone enters a state of psychosis, we can say that prior to the onset of psychosis, for whatever reason, they have arrived at a way of being in the world and experiencing of the world that is no longer sustainable (i.e., is poorly resourced), and it seems that their predicament cannot be resolved using more ordinary strategies. As a desperate last-resort strategy, then, one’s own psyche may initiate a psychotic process. As the individual enters into a psychotic process, we can say that their very self, right down to the most fundamental levels of their being, undergoes a process of profound disintegration; and as we have seen in the recovery research, with the proper conditions and support, there is every possibility of their continuing on to profound reintegration and eventual reemergence as a renewed self in a significantly changed and more resourced state than that which existed prior to the psychosis.
This is why the intentional destabilization of one’s cognitive constructs may be so beneficial, although of course very risky. It is this very loosening of one’s personal paradigm—of one’s experience and understanding of one’s self and of the world—that allows an individual to undergo such a profound transformation at such a deep level of their being. When such a process resolves successfully, the potential amount of growth and/or healing that this allows is enormous; but of course, when such a process does not resolve successfully, an individual’s personal paradigm may remain unstable and chaotic indefinitely (think florid psychosis).
This idea is well supported in the recovery research in the findings that many people who make full recoveries from psychosis often experience a degree of wellbeing and ability to meet their needs that far exceeds that which existed prior to their psychosis (Arieti, 1978; House, 2001; Karon & VandenBos, 1996; Laing, 1967; May, 1977; Mindell, 2008; Mosher, 1999; Mosher & Hendrix, 2004; Nixon et al., 2009, 2010; Perry, 1999; Williams, 2011, 2012). It’s important to keep in mind, of course, that such resolution is not always successful, and that an individual may remain in a psychotic condition indefinitely. But we must also not lose sight of the very hopeful findings from the recovery research that suggest that such a successful resolution from a psychotic process is surprisingly common, and may even be the most common outcome given the proper conditions and support (Hopper et al., 2007; Perry, 1999; Mosher, 1999; Mosher & Hendrix, 2004; Seikkula et al., 2006).
Finally, one particularly compelling implication of these findings is that if it turns out to be true that those who have experienced psychosis have struggled profoundly with the universal existential dilemmas that most of us have only barely consciously grasped, then these individuals may have the potential to contribute greatly to the very important human quest to understand what it is that really drives us.
Dr. Paris Williams, author of Rethinking Madness, works as a psychologist in the San Francisco Bay Area. He offers the rare perspective of someone who has experienced psychosis from both sides—as a researcher and psychologist, and as someone who has himself fully recovered after struggling with psychotic experiences. He can be reached at: www.RethinkingMadness.com/contact.
You can find a much more thorough discussion of these and related topics in Dr. Williams’ recently published book, “Rethinking Madness” (Sky’s Edge Publishing), which is available through Amazon.com and most other major retail outlets. More information is available at www.RethinkingMadness.com
References
American Psychiatric Association [APA]. (2010). Schizophrenia. Retrieved from The American Psychiatric Association Healthy Minds, Healthy Lives website: http://www.healthyminds.org/Main-Topic/Schizophrenia.aspx
Arieti, S. (1978). On schizophrenia, phobias, depression, psychotherapy, and the farther shores of psychiatry. New York, NY: Brunner/Mazel.
Bassman, R. (2007). A fight to be: A psychologist’s experience from both sides of the locked door. New York, NY: Tantamount Press.
Beck, J., and van der Kolk, B. (1987). Reports of childhood incest and current behavior of chronically hospitalized psychotic women. American Journal of Psychiatry, 29, 789-794.
Beers, C. W. (1981). A mind that found itself. Pittsburgh, PA: University of Pittsburgh Press.
British Psychological Society [BPS]. (2000). Recent advances in understanding mental illness and psychotic experiences. A report by The British Psychological Society Division of Clinical Psychology. Leicester, UK: Author.
Chadwick, P., Birchwood, M. J. & Trower, P. (1999). Cognitive therapy for delusions, voices and paranoia (Wiley series in clinical psychology). New York: John Wiley and Sons.
Dorman, D. (2003). Dante’s cure. New York, NY: Other Press.
Greenberg, J. (1964). I never promised you a rose garden. Chicago: Signet.
Hagen, B. F., Nixon, G., & Peters, T. (2010). The greater of two evils? How people with transformative psychotic experiences view psychotropic medications. Ethical Human Psychology and Psychiatry: An International Journal of Critical Inquiry, 12(1), 44-59.
Harrow, M., & Jobe, T. (2007). Factors involved in outcome and recovery in schizophrenia patients not on antipsychotic medications: A 15-year multifollow-up study. Journal of Nervous and Mental Disease, 195(5), 406-414. Retrieved from http://www.madinamerica.com/madinamerica.com/Schizophrenia_files/OutcomeFactors.pdf
Harrow, M., Jobe, T. H., & Faull, R. N. (2012). Do all schizophrenia patients need antipsychotic treatment continuously throughout their lifetime? A 20-year longitudinal study. Psychological Medicine, First View Articles, 1-11. doi: 10.1017/S0033291712000220
Honig, A., Romme, M., Ensink, B., Escher, S., Pennings, M., & de Vries, M. (1998). Auditory hallucinations: A comparison between patients and nonpatients. The Journal of Nervous and Mental Disease, 186, 646-651.
Hopper, K., Harrison, G., Janca, A., & Sartorius, N. (2007). Recovery from schizophrenia: An international perspective: A report from the WHO Collaborative Project, The International Study of schizophrenia. New York, NY: Oxford University Press
House, R. (2001). Psychopathology, psychosis and the kundalini: Postmodern perspectives on unusual subjective experience. In I. Clarke (Ed.), Psychosis and spirituality: Exploring the new frontier (pp. 75-89). London: Whurr Publishers.
Hyman, S., & Nestler, E. (1996). Initiation and adaptation: A paradigm for understanding psychotropic drug action. The American Journal of Psychiatry, 153(2), 151-162. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/8561194
Joseph, J. (2004). Schizophrenia and heredity: Why the emperor has no genes. In J. Read, L. R. Mosher, & R. P. Bentall (Eds.), Models of madness: Psychological, social and biological approaches to schizophrenia (pp. 67-83). New York, NY: Routledge.
Karen, R. K. (1994). Becoming attached: First relationships and how they shape our capacity to love. Oxford, UK: Oxford University Press.
Karon, B. P. (2003). The tragedy of schizophrenia without psychotherapy. Journal of the American Academy of Psychoanalysis, 31(1), 89-119. doi:10.1521/jaap.31.1.89.21931
Karon, B. P., & VandenBos, G. (1996). Psychotherapy of schizophrenia: The treatment of choice. Lanham, MD: Rowman & Littlefield Publishing, Inc.
Laing, R.D. (1967). The politics of experience. New York: Pantheon Books.
Lewine, R. (1998). Epilogue. In M. F. Lenzenweger & R. H. Dworkin (Eds.), Origin and development of schizophrenia (pp. 493-503). Washington, DC: American Psychological Association.
Livingston, R. (1987). Sexually and physically abused children. The Journal of the American Academy of Child and Adolescent Psychiatry, 26: 413-415.
Mahler, M. S., Pine, F., & Bergman, A. (1973). The psychological birth of the human infant, New York: Basic Books.
May, R. (1977). The meaning of anxiety. New York: W. W. Norton & Company.
Mindell. A. (2008). City shadows: Psychological interventions in psychiatry. New York, NY: Routledge.
Modrow, J. (2003). How to become a schizophrenic: The case against biological psychiatry. Lincoln, NE: Writers Club Press.
Mosher, L. R. (1999). Soteria and other alternatives to acute psychiatric hospitalization: A personal and professional review. The Journal of Nervous and Mental Disease, 187, 142-149.
Mosher. L. R., & Hendrix, V. (with Fort, D. C.) (2004). Soteria: Through madness to deliverance. USA: Authors.
National Institute of Mental Health [NIMH]. (2010a). Schizophrenia. Retrieved from http://www.nimh.nih.gov/health/publications/schizophrenia/complete-publication.shtml
National Institute of Mental Health [NIMH]. (2010b). How is schizophrenia treated. Retrieved from http://www.nimh.nih.gov/health/publications/schizophrenia/how-is-schizophrenia-treated.shtml
Nixon, G., Hagen, B. F., & Peters, T. (2009). Psychosis and transformation: A phenomenological inquiry. International Journal of Mental Health and Addiction. doi: 10.1007/s11469-009-9231-3
Nixon, G., Hagen, B. F., & Peters, T. (2010). Recovery from psychosis: A phenomenological inquiry. International Journal of Mental Health and Addiction. doi: 10.1007/s11469-010-9271-8
Perry, J. W. (1999). Trials of the visionary mind. State University of New York Press.
Rathus, S. A. (2006). Childhood and adolescence: Voyages in development. Belmont, Canada: Thompson Wadsworth.
Read, J. (2004). Biological psychiatry’s lost cause. In J. Read, L. R. Mosher, & R. P. Bentall, (Eds.), Models of madness: Psychological, social and biological approaches to schizophrenia (pp. 57-65). New York: Routledge.
Robins, L. (1974). Deviant children grown up: A sociological and psychiatric study of sociopathic personality. Malabar, FL: R. E. Krieger Pub. Co.
Romme, M., Escher, S., Dillon, J., Corstens, D., & Morris, M. (2009). Living with voices: 50 stories of recovery. Herfordshire, UK: PCCS Books.
Satcher, D. (1999). Etiology of schizophrenia. Retrieved, from http://www.surgeongeneral.gov/library/mentalhealth/chapter4/sec4_1.html
Schore, A. N. (2002). Advances in neuropsychoanalysis, attachment theory, and trauma research: Implications for self psychology. Psychoanalytic Inquiry, 22, 433-484.
Seikkula, J., Aaltonen, J., Alakare, B., Haarakangas, K., Keränen, J., & Lehtinen, K. (2006). Five-year experience of first-episode nonaffective psychosis in open-dialogue approach: Treatment principles, follow-up outcomes, and two case studies. Psychotherapy Research, 16(2), 214-228. doi: 10.1080/10503300500268490.
Siebert, A. (1999). Brain disease hypothesis for schizophrenia disconfirmed by all evidence. Retrieved from http://psychrights.org/states/Alaska/CaseOne/180Day/Exhibits/Wnotbraindisease.pdf
Slade, A. (1999). Attachment theory and research: Implications for the theory and practice of individual psychotherapy with adults. In J. Cassidy & P. R. Shaver (Eds.), Handbook of attachment: Theory, research, and clinical applications (pp. 575-594). New York: Guilford press.
Wallin, D. J. (2007). Attachment in psychotherapy. New York: The Guilford Press.
Whitaker, R. (2002). Mad in America. New York: Basic Books.
Williams, P. (2011). A multiple-case study exploring personal paradigm shifts throughout the psychotic process from onset to full recovery. (Doctoral dissertation, Saybrook Graduate School and Research Center, 2011). Retrieved from http://gradworks.umi.com/34/54/3454336.html
Williams, P. (2012). Rethinking madness: Towards a paradigm shift in our understanding and treatment of psychosis. San Francisco: Sky’s Edge Publishing.
Woodruff, P. W. R., & Lewis, S. (1996). Structural brain imaging in schizophrenia. In S. Lewis & N. Higgins (Eds.), Brain imaging in psychiatry. Oxford, UK: Blackwell.












This is very good.
I agree with most of it. I think “hearing voices” should/could be described in less passive terms, if one wants to change people’s minds about the medical model. Self-conversations that one doesn’t attribute to coming from oneself, is more like it. Or self-conversations disowned, character narratives involving internal conversations between self-generated speakers, is more like it.
There is a reason these thoughts are conversations and “voices” instead of the sound of jet engines, or car-crashes. They have to be voices, and talking, and conversations, because that is how we think, in narratives and words. Of course, the rare exception would be if the trauma had something to do with a car-crash or jet engine.
My point is, when the “hearing voices movement” doesn’t explain this, and just uses language that is so, well, passive, it tends to be interpreted in the public’s mind as “auditory hallucination caused by a brain disease”, now I ask, if it is an “auditory hallucination”, why wouldn’t it be a jet engine noise as often as it is a persecutory conversation? Of course, there is much more to the story than just the simple and passive, “hearing things”, what is heard most is words, conversations, and these are actively participated in, and are a thread of the narrative that the individual is running in their mind in this crisis, or just daily life.
We all talk to ourselves, and hear our own mental “voice” all the time, it can be a strategy to disown a portion of this inner self conversation and assign its origin “elsewhere” as in, to “a voice”, or “one of several voices”, but just generally, I feel the so called “hearing voices movement”, has done a very poor job at communicating these facts, and has left themselves open to appearing dangerous, as if to appear under the control of external forces, using such passive language as “hearing”, when it is in fact a “participation” also. I think the stigma and mainstream media Hollywood narrative around people with psychiatric labels being controlled by “voices in their head”, could potentially be fueled and fed, in a damaging way, by the continued, deepening, and firming of the passive language of that the “hearing voices” movement uses, I’m also concerned about this exceptionalism that creeps in, as though people with psychiatric labels are a special breed apart, as though every human being doesn’t have conversations with themselves, or every child too, I know to some extent this movement has tried to point out that it is a “common experience”, I would say this is where I disagree most with the hearing voices movement, I say inner voice is a universal experience, it is just that only people with psychiatric labels are the ones who mostly seem to disown these inner voices, fall into the strategy of disowning them, disembodying them from their own inner voice, splitting them off into character narratives and conversations of more degrees of separation that the most people’s inner voice.
When the mainstream public hears of a movement trying to normalize so called “auditory hallucinations”, they think of a brain auditory system gone haywire, and think of biology, hearing, ear drums, and brains, and a chaotically diseased brain randomly throwing up all sorts of sounds and noises. When in fact this is not the case at all, these are narratives and conversations with oneself and conversations with thoughts and disowned character narratives about your internal narrative.
People who wind up being labeled by psychiatry with the “psychotic” label, tend to conversationalize the inner narrative of the mind a lot more than the average person, but I really do worry sometimes about what choosing to use the passive phrase “hearing voices” is doing to us. It seems to also contain an element of potential for its own self-fulling prophecy.
I had been marginally aware of your book, hadn’t read it, but after this article, it appears to be a must buy.
The first 75% of this article, is among the top 20 short form pieces of writing on this I’ve ever seen. It’s tight, taut and carefully organized prose. I’m not a fan of butterfly analogies though.
When the mainstream public hears of a movement trying to normalize so called “auditory hallucinations”, they think of a brain auditory system gone haywire, and think of biology, hearing, ear drums, and brains, and a chaotically diseased brain randomly throwing up all sorts of sounds and noises. When in fact this is not the case at all, these are narratives and conversations with oneself and conversations with thoughts and disowned character narratives about your internal narrative.
“The British Psychological Society (the BPS, Great Britain’s counterpart to the American Psychological Association), in its official report summarizing their understanding of “mental illness” and “psychotic experiences,” concluded that the various psychotic disorders may more appropriately be classified as variations of one phenomenon, a phenomenon that many have suggested we refer to simply as psychosis or madness.”
How about they are variations on the phenomenon of THINKING! Everybody thinks thoughts sometimes that are, some of us, at various points, more extreme thoughts. I’m never going to identify as “psychotic” or “mad”. Each of those words are hate-speech to my ears, ears carefully honed after years of saturation in degrading stigma.
The experiences that get labeled “psychotic” are indeed not brain diseases. And while point by point refutations of psychiatry’s crap are necessary, one simple, taut, and elegant proof is available to every single human being in the world if they want to personally test psychiatry’s insight into the brain:
Take yourself to a psychiatrist and ask him to examine your brain. When you leave his office brain unexamined, as millions before you have, just reflect on that for a moment, reflect on the fact that this quack never examined your brain, or your genes, and then ask yourself, if this profession has any special insights into how YOUR brain is functioning. It doesn’t.
If anything you’ve read above in this article (not this comment) is news to you, and you are starting to be convinced this profession (psychiatry) can’t prove distressed people have brain diseases, it might be decent of you to reflect on the fact that your government, in your name, forcibly confiscates the brains of many of your fellow citizens and hands these brains, over to this quack profession (while the person is living and conscious), it’s called forced drugging. It’s abhorrent, horrific and the most invasive thing your government does to innocent people by force as a matter of public policy. It is horrific to live through, it traumatizes its victims for life, and it must stop.
Report comment
“How about they are variations on the phenomenon of THINKING!” — I so agree. As I, in part, do with your criticism of the HVN (which I’m a member of). The point is, the HVN has, at least to some extent, the same problem that “the movement” in general has: its members represent all kinds of views on their experience. So, when you, as a member of the HVN, state that you view your experience of hearing voices as a way of thinking, there will always be a number of other HVN members who will tell you that they view their experience in a different way, that they don’t quite agree. On the other hand, the HVN still stands somewhat stronger than “the movement” in general, because its official message is that the experience of hearing voices, no matter how it otherwise is interpreted, is a meaningful one seen in context with the person’s life story. While “the movement” in general can’t even agree on the basics, i.e. whether to believe in meaningless brain diseases, or meaningful reactions to life.
Report comment
Thank you. I agree the HVM has done a lot of good. I am just concerned about this message of passivity versus acknowledging active participation in the internal conversation.
That is the first time I’ve ever tried to write anything about the HVM, I could be clearer if I spent more time on it, but since it kind of stuck out at me when I read the original article above, I thought I’d throw in my two cents.
Report comment
Thanks for sharing your important thoughts and insights.I really appreciate your desire to “normalize” experience such as hearing voices.
You may already be aware that there is some interesting research that, for many people who hear voices, some research has shown that micro-movements are occurring in the mouth/jaw muscles that seem to match the words the person is hearing. This suggests that, at least for some people, the voices they hear most likely really are just their own inner speech (that we all have, as you say), which has merely become mistaken as coming from a non-self source (i.e. has become ego dystonic).
On the other hand, when we look more closely at the recovery research, we find that for many people, what’s most important is that they have the freedom to personally explore the meaning of their voices or other anomalous experiences and develop the meaning that personally resonates for them, even though this process of meaning-making is often ongoing.
Also, it does seem true that for some people, hearing voices may stand alone as a simple and relatively self-contained anomalous experience, and simply learning to recognize that they’re mistaking their natural inner speech as being something alien to the self is enough for them to make peace with this experience and regain relative wellbeing. However, for many other people, hearing voices is merely one manifestation of a deeper struggle or split occurring within one’s psyche. In this case, hearing voices may be merely one sign that a powerful transformative process has begun and that it requires some resolution in order for the person to regain a sense of real peace in their life — this brings us to the idea I tried to illustrate with the “butterfly metaphor” that you weren’t particularly fond of 🙂 Using the “sanity/madness continuum” (Figure 3 in the article), we could say that the former individuals would be somewhere in the second or upper part of the third categories listed next to this continuum, whereas the latter individuals would be deeper into the third or even fourth categories. You can find one good example of a person in this latter category in Chapter 24: “The Case of Cheryl.”
Paris Williams
Report comment
I agree. I look forward to reading your book!
Report comment
Regarding psychosis, the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) classifies psychotic illnesses as “Psychosis Due to General Medical Conditions”, and “Substance Induced Psychosis”. (DSM-IV Codes 293.81 & 292.11).
Psychosis Due to a Medical Condition involve a surprisingly large number of different medical conditions, some of which include: brain tumors, cerebrovascular disease, Huntington’s disease, multiple sclerosis, Creitzfeld-Jakob disease, anti-NMDAR Encephalitis, herpes zoster-associated encephalitis, head trauma, infections such as neurosyphilis, epilepsy, auditory or visual nerve injury or impairment, deafness, migraine, endocrine disturbances, metabolic disturbances, vitamin B12 deficiency, a decrease in blood gases such as oxygen or carbon dioxide or imbalances in blood sugar levels, and autoimmune disorders with central nervous system involvement such as systemic lupus erythematosus have also been known to cause psychosis.
A substance-induced psychotic disorder, by definition, is directly caused by the effects of drugs including alcohol, medications, and toxins. Psychotic symptoms can result from intoxication on alcohol, amphetamines (and related substances), cannabis (marijuana), cocaine, hallucinogens, inhalants, opioids, phencyclidine (PCP) and related substances, sedatives, hypnotics, anxiolytics, and other or unknown substances. Psychotic symptoms can also result from withdrawal from alcohol, sedatives, hypnotics, anxiolytics, and other or unknown substances.
Some medications that may induce psychotic symptoms include anesthetics and analgesics, anticholinergic agents, anticonvulsants, antihistamines, antihypertensive and cardiovascular medications, antimicrobial medications, antiparkinsonian medications, chemotherapeutic agents, corticosteroids, gastrointestinal medications, muscle relaxants, nonsteroidal anti-inflammatory medications, other over-the-counter medications, antidepressant medications, neuroleptic medications, antipsychotics, and disulfiram . Toxins that may induce psychotic symptoms include anticholinesterase, organophosphate insecticides, nerve gases, heavy metals, carbon monoxide, carbon dioxide, and volatile substances (such as fuel or paint).
The BMJ published guidelines for Best Practice Assessment of psychosis, accordingly, even the routine use of over-the-counter cold medicine can induce a psychotic episode clinically indistinguishable from paranoid schizophrenia.
http://psychoticdisorders.wordpress.com/bmj-best-practice-assessment-of-psychosis/
Report comment
I’ve seen you copy and paste the same long-winded list on this site before. Perhaps next time you could come up with something specifically for our comment conversation instead of copying and pasting the entire contents of your blog.
The mental confusion this list of drugs might contribute to, is by no means the same thing just because the BMJ, or you, decided to label it all “psychosis”.
Next time a simple link to your blog, which you have included, would be better than pasting every word that can be found at that link.
Report comment
Dear Anonymous,
Thank you for pointing out that you find my comments long-winded and that you do not feel they are specific to your comment conversation. I rarely post comments on this site so I am a bit surprised that you seem to have taken such offense to posting this information.
Please accept my appologies as I will try to clarify my position for you and why I would feel it is important to distribute this information on a post regarding schizophrenia/psychosis and brain disease.
My goal as a mental health advocate is to create awareness of underlying medical conditions and substances that can create what appears to be a manic/psychotic state and can lead to an individual being MISDIAGNOSED as having bipolar disorder/schizophrenia. As an advocate, I also support the Participatory Medicine movement in mental health care.
“The mental confusion this list of drugs might contribute to, is by no means the same thing just because the BMJ, or you, decided to label it all ‘psychosis’.”
I am not a mental health professional and I am not responsible for labeling psychotic disorders. The BMJ is just a journal and is not responsible for labeling psychosis either. Information regarding medical conditions and substances that can induce psychosis/mania is listed in the DSM, unfortunately it is ignored by most mental health professionals.
The mental confusion caused by this list of drugs might be MISDIAGNOSED as bipolar disorder/schizophrenia by a medical professional, this is why I feel it is important to try and create an awareness whereever and whenever possible.
Advocacy is needed to prevent individuals with mental confusion because of these underlying conditions from being misdiagnosed “mentally ill” and mistreated with psych meds.
“A best practice is a method or technique that has consistently shown results superior to those achieved with other means, and that is used as a benchmark. In addition, a ‘best’ practice can evolve to become better as improvements are discovered”
The British Medical Journal is a trusted source of information and the best practice guidelines they have established to assess the mental confusion that presents as psychosis support integrative psychiatry, functional medicine and an Orthomolecular approach.
If an individual is suffering from mental confusion and what presents as psychotic/manic state and seeks treatment, often they are labeled as schizophrenic/bipolar and very little testing is done to rule out underlying causes.
I copy and paste the entire list of underlying causes where I think it is appropriate so that key words and phrases are available for those searching for information online.
My main goal is to get the key words and phrases out there to help individuals who might be helped by this information, as I was.
I did not realize it would annoy individuals like yourself who do not care about this information. A simple copy and paste is quick and easy as it is rather time consuming to elaborate with a comment and usually leads to long-winded point-counterpoint discussions.
Certain individuals may be misdiagnosed and entitled to malpractice, or worker’s compensation, as well as alternative therapies paid for by their insurance company.
For example, if an individual is suffering from symptoms that appear to be mania/psychosis because of past exposure to lead, they should be entitled to chelation therapy paid for by their insurance.
In my opinion, mental health advocates should be fighting for the rights of patients to be provided alternatives paid for by their insurance companies. I feel the gateway for this is through integrated care, which the APA appears to be embracing.
I created the blog linked above as a way to collect peer-review articles and case studies that recognize underlying causes of what presents as psychosis/mania because this helps support cases of malpractice and worker’s comp. I started collecting articles during my own worker’s comp case and putting them on a blog just seemed easier to share them with others who were pursuing worker’s comp cases from toxic exposure.
With so many bloggers adding content, the Mad in America site generates a lot of hits. I don’t think many of the writers support integrative psychiatry, functional medicine, an Orthomolecular approach, or even mention the work of Dr. Abram Hoffer.
Considering the diverse perspectives and conflicting opinions in mental health care, acknowledging a best-practice approach is fundamental.
Once again, my appologies. For my own worker’s comp case I dug through the medical library the old fashion way. Since then I have helped 5 other individuals who were originally labeled with bipolar disorder establish worker’s comp cases because of long-term chemical exposure. That may not seem like much but it’s better to light a candle than to curse the darkness.
Below is a link to a narrative I wrote that outlines my position further.
Kind Regards,
Maria Mangicaro
http://www.jopm.org/perspective/narratives/2011/03/28/psychosis-possibly-linked-to-an-occupational-disease-an-e-patient%E2%80%99s-participatory-approach-to-consideration-of-etiologic-factors/
Report comment
I have similar thoughts to you on the subject, but I occasionally take heat from some of the bloggers, myself, usually because they’re unfamiliar with the subject you’ve been writing about, perhaps because they devote a lot of energy going after psychiatric pseudo-medicine with all its arcane disorders of one kind or another.
Report comment
I think that your comment brings up an interesting point that would be important to further explore: How exactly do we distinguish the distressing/limiting anomalous perceptions and beliefs (so called “delusions” and “hallucinations”) that occur in correlation with well known physiological disorders such as Alzheimer’s, certain types of strokes, traumatic brain injury, etc., etc. from the anomalous experiences that are correlated with the so called “psychiatric psychoses” that have not so far been correlated with clear physiological disorders. And is such a distinction possible or even helpful?
My own thoughts on this are that the existential dilemmas I refer to in the article are essentially universal and always present, so long as there is consciousness, regardless of serious physiological disorder or lack thereof. However, as I alluded to in the article, it appears that certain stressors (some predominantly physiological and others predominantly psychological) may make one vulnerable to being overwhelmed by these dilemmas. For the relatively “healthy and well functioning” individual, our constructs/personal paradigm do quite a good job of keeping these dilemmas mostly out of the conscious mind and relatively tamed. However, powerful stressors can rock the boat, so to speak, and then we suddenly found these dilemmas flooding into our experience, resulting in our psyche resorting to desperate strategies to cope with these and attempt to re-integrate them.
I spent some time working in a regular (non-psychiatric) hospital, on the post-acute ward filled with people suffering from severe physiological and neurological disorders (Alzheimer’s, strokes, etc.). And I realized that many of these people were indeed struggling with these same core existential dilemmas. The main difference I saw between these people and those diagnosed with “schizophrenia” or the other major “psychiatric psychotic disorders,” was that in those with neurological disorders, they were also struggling with experiences clearly caused by some damage in the “wiring,” such as various types of paralysis, aphasia (inability to speak), significant memory deficits, sensory deficits (blindness, tactile disability, deafness, etc.), etc., many of which were not likely to improve. Those who have been diagnosed with a “psychiatric psychotic disorder” are fortunate in that they generally don’t struggle with these other kinds of physiological deficits, and so have the potential to return to the level of functioning/wellbeing that existed prior to their psychosis (or even beyond that).
In short, then, I believe that there are core existential dilemmas to which we’re all dealing with all of the time (although for most of us, these are primarily unconscious), regardless of one’s degree of physiological functioning. Then, separate from this although certainly in interaction with these, physiological and neurological disorders add their own set of problems, though these other problems certainly interact with one’s struggle to maintain peace with the various existential dilemmas.
One final caveat: I believe that for the sake of effective communication and providing support for people in need, such distinctions are important. But I believe it’s also important not to lose sight of the profound interdependence of all aspects and experiences that occur within a living organism.
Report comment
My God. I really need to buy your book now.
Listen I uncharitably told this lady to stop repetitively copying and pasting her thing about this, maybe I could have been more police. But I have seen that exact same text, multiple times on other articles, with zero further tailored comment from this person, so I just told her to expand what she had to say next time. The comment I left had been bothering me.
But your answer. Was 98% perfect.
You addressed physiological and neurological disorders, in the lady’s pasted and extensive list of things, you didn’t address drugs.
What is your opinion about the contribution of drugs to thoughts/actions, and responsibility.
This site plays host to a number of writers and readers who believe that psychiatric drugs cause suicides and massacres.
I have long asked them why they believe in the power of drugs to cause people to make the choice to kill themselves, but not in the power of drugs to cause someone to purchase an automobile. Bear in mind, in recent days we have had plenty of people on this site claim that the Colorado shooter, who planned his attack for months, falls into this category. I mention this to head off at the pass any question you might have about impulsive actions.
Report comment
Thanks for bringing up the “drug” issue, which of course is complex and diverse. Regarding the correlation between certain types of psychoactive drug use and psychosis (especially stimulants, marijuana, and hallucinogens), from the perspective of the model I’ve presented here, I would say that these kinds of drugs can loosen one’s cognitive constructs, which can be both beneficial when used carefully (there has been significantly hopeful research on the potentially therapeutic benefits of LSD therapy, for example), and potentially harmful when not (e.g., the potential for leading to an overwhelming “psychotic” condition).
Regarding the topic of the harms and benefits of antipsychotics for those experiencing psychosis, here is a concise summary of what I believe are the most relevant findings from the research:
• The use of antipsychotics helps reduce the positive symptoms of psychosis and the associated distressing emotions for many people in the short term (during the first six weeks or so).
• The long-term use of antipsychotics increases the likelihood of the development of a chronic psychotic condition and significantly reduces the likelihood of recovery, as well as carrying the high likelihood of causing other serious physical, cognitive, and emotional impairments. The specific effects of such use clearly vary significantly from one individual to another, but generally speaking, this has been a strikingly consistent and reliable finding.
• Those individuals who are never exposed to antipsychotics have the highest chance of recovery.
• Regardless of the treatment method, it seems that there is always some percentage (although relatively small—apparently about 15%) that is likely to remain in a chronic psychotic condition indefinitely.
• The medical model paradigm, with its associated beliefs of brain disease and terminology such as “mental illness,” can significantly increase stigma, fear, hopelessness, and other associated distressing emotions and behavior.
• Residents of so-called developing countries have much higher recovery rates than those in so-called developed countries, and the use of antipsychotics and the medical model paradigm of treatment is inversely correlated with recovery rates.
• Residential facilities that offer continuous empathic support and freedom, and which minimize the use of antipsychotics, have demonstrated the ability to provide significantly better outcomes for their residents at significantly less cost than what the standard psychiatric model of care has been able to provide. However, these alternative approaches may reduce some personal benefits for many professional caregivers and others in the psychiatric drug industry (e.g., personal income, job security, sense of order and control in the environment, etc.), and it is likely that this is a major factor in our mental health care system’s resistance to change.
Paris Williamsw
Report comment
“Regarding the correlation between certain types of psychoactive drug use and psychosis (especially stimulants, marijuana, and hallucinogens), from the perspective of the model I’ve presented here, I would say that these kinds of drugs can loosen one’s cognitive constructs, which can be both beneficial when used carefully”
I’m more interested at this point in your opinion of the contention that psychiatric in and of themselves, cause, violence and suicide.
Not weed or LSD, psychiatric drugs.
Thank you.
Report comment
Regarding the correlations between violence/suicidality and the use of antipsychotics, here is some relevant research to consider:
Recent research suggests that schizophrenia patients who are given antipsychotic treatment today commit suicide at a rate twenty times higher than that of schizophrenia patients prior to the introduction of antipsychotic treatment. This is an astonishing figure, and it is important to keep in mind that this represents a correlation, and not necessarily causation; nonetheless, given the magnitude of this correlation, it would be difficult to deny that antipsychotics almost certainly play a significant role in this greatly increased suicide rate.
Regarding violence, akathisia is a term used to describe the condition in which one feels overwhelming agitation and restlessness on the inside while feeling trapped in a body that is heavily sedated and unresponsive, a common side effect of antipsychotic drug use. Those who have experienced akathisia often describe it as the most severe torment, the severity of which is virtually impossible for those who have not experienced it to fully grasp. Research has shown high correlations between akathisia and suicidality, homicidality, and other violent behavior.
For further discussion of the link between violence and psychosis/schizophrenia, and between violence and the use of antipsychotics, I recommend listening the following interview with Robert Whitaker on “Madness Radio”:
http://www.madnessradio.net/madness-radio-2006-10-11-robert-whitaker-violence-and-madness
Regarding the link between the recent Colorado massacre and the “medical model” understanding of psychosis/schizophrenia, I recommend the following blog post by David Oaks of MindFreedom Interational:
http://www.mindfreedom.org/mfi-blog/2012/07/21/holmes-biomarkers-psychiatric
Paris Williams
Report comment
That is a good answer. I still say those who are quick to blame heavily planned and clearly not impulsive crimes on drugs, are jumping the gun.
Clearly too, there is much more hopelessness injected into the lives of people labeled SZ and this and many other facts should be factored in to the increased suicidality.
I have experienced akasthisia, it was an unpleasant sensation, but I retained my ability to see right and wrong, and didn’t commit a massacre.
Report comment
One of the things most of the bloggers don’t know, is that the various attempts by mainstream guys to understand psychoses came from attempts to disprove another biological notion- that the syndrome isn’t a brain disease at all, but a metabolic disorder in which one’s own body produces hallucinogens, especially under stress, which can come from any number of stressors.
Report comment
Sean Blackwell also has an interesting perspective on bp/schizophrenia
http://www.youtube.com/watch?v=Db8AYSrs2kk&list=PLC41AE6B1DB0C0EA0&feature=plcp
Report comment
Thanks for your great work, and for sharing it here. I haven’t read your book yet (but did order it).
I am very convinced by everything you say, and your model seems powerful when applying it to at least some “mad” people I have befriended.
You associate delusions with a loosening of cognitive structures (during some crisis). I would say it is important to distinguish unstable breaks with reality (corresponding to a loose structure with no self-consistency over time), from very stable delusions (possibly lifelong) that form an extremely logic/rational/self-reinforcing perception of reality (and that can develop in a rational non-traumatic way) with hardly any more contradictions that “consensus reality” (I love that expression).
For instance, some paranoid people are often very logical/rational/intelligent, and have developed a dog-eat-dog model of their environment that is hard to disprove without the possibility of mind-reading (any act of good-will is seen as being a conscious and purposeful malevolent grooming-manipulative act), and don’t have significant dilemmas about their place in it.
Report comment
Thanks for your comment and insights–these are important points.
I briefly refer to the distinction you suggest (relatively stable/even lifelong anomalous experiences vs. relatively unstable experiences)in Figure 3 of the article, suggesting this distinction as not being black and white but perhaps lying along the “sanity/madness continuum” from the second to the fourth categories.
I also go into this distinction in much more detail in my book, Rethinking Madness, and give specific case examples to draw a distinction, while also not losing sight of the continuum nature of this and also the relative nature of this. For example, we can argue that members of one religion, political orientation, or culture may appear to maintain long-term “delusions” to members of a different religion, political orientation or culture. Yet there is clearly something a little different going on in this case than with someone whose constructs of reality are clearly quite loose and fluctuation in a fairly wild manner (so called “florid psychosis”). And there’s something to be said for questioning the health of people on both ends of this spectrum–those experiencing particularly loose cognitive constructs on one end, and those experiencing particularly rigid and dogmatic constructs on the other.
Paris Williams, PhD
Report comment
Hi Paris,
Wow! What a pleasant surprise to wake and find this substantial op-ed piece, after re-reading your Doctoral Dissertation last night. I really appreciate your efforts to bring our focus of attention onto what the experience of psychosis actually is, instead of the usual focus on how to treat an assumed illness.
It is a substantial contribution which sadly may be under-appreciated by many readers in our innate need for the quick grasp and easy digestion of knowledge. Hence people are enamored with poetic phrases and their transitory affect, as an example of the metabolic (chemical) fueling of subjective states of awareness?
We all seem to have our preferred world-view when it comes to interpreting the existential nature of our life, as we look through slightly differing len’s at the same phenomena? The neuroscientist and psychologist vying for a differentiation of self within the social matrix?
Having experienced the divine madness, otherwise known as mental illness for 32 years now I agree 100% that psychosis is triggered by an existential crisis, however I think the notion of intention is confusing? Rather I believe it to be a question of circumstance, in which your metaphor analogy of the butterfly is so apt, on more than one level?
Since documenting my flights into bipolar type1 mania, for over five years now. Attachment, loss and separation anxiety, is the guaranteed trigger to my six week long bouts of euphoric ecstasy. Separation from my grounding attachment to a lover, has been the butterfly effect to my most potent mania’s were I’ve been through all the the usual savior self-referential ideas of a special person destiny, down to the realization of species metaphor in individual experience?
“In order for a poorly resourced larva to transform into the much more highly resourced butterfly, it must first disintegrate at a very profound level, its entire physical structure becoming little more than amorphous fluid, before it can reintegrate into the fully developed and much more resourced form of a butterfly.”
Or we could use the acorn metaphor of all we are meant to be in our evolved nature, contained in the butterfly effect of that chaos & chance instant, when a particular sperm penetrates a fertile egg? Can such levels of existential reality be captured in language, like “cognitive constructs & personal paradigm?”
It would seem that while trying to view the same phenomena neuroscience uses the language of neuropeptides while psychologists prefer cognitive constructs and even older world terminology like psyche and soul. Yet is any of our thus far evolved language, capable of grasping the essence of the actual experience?
You use the language of psychology really well in your re-examining of the evidence on psychotic experience, and in your proposal of a new model, yet like all of us in our particular world-view, do we make it fit by leaving out most of the bigger picture? Are we trapped in a gestalt of foreground attention, in our need of immediate function?
Six weeks after my last six week long psychosis, the euphoric sense of oneness grasped on an unspeakable level of being, does not translate easily in my immediate need of articulation? What helps me go through it now, in my efforts to understand it, is the sensate awareness of Peter Levine’s somatic-experience techniques, which allow me to sense the actual sensations of nervous system orientation described so well by Allan N Schore and particularly Stephen Porges.
So these days when I read a brilliant paper like Roland Fischer’s, I can sense what he’s on about within my physiological being, rather than my cognitive constucts?
Five years ago, when I first began to read the literature of neuroscience, I fully expected to learn how my brain was responsible for my bipolar type 1 condition. How my consistent experiences of spiritual Ecstasy in euphoric mania were stimulated by my faulty and diseased brain chemistry? I did not expect to read consistent references to my body, and its autonomic nervous system (ANS), in relation to symptoms in mental illness, and spiritual experience. Yet over and over again I read about the sympathetic and parasympathetic branches of my (ANS). Unexpected, because such information is hardly ever part of mainstream reporting on research into mental illness experience and causation?
How is my nervous system responsible for my perceptions of a Cosmic Oneness?
Consider an excerpt from Roland Fischer’s brilliant paper on hallucination, delusion and the role our autonomic nervous system plays in both our normal and abnormal perceptual awareness;
“During the ”I”-state of daily routine, the outside world is experienced as separate from oneself. With increasing ergotropic (sympathetic nervous system) and trophotropic (parasympathetic nervous system) arousal, however, this separateness gradually disappears, apparently because in the “Self”-state of ecstasy and samadhi, cortical and subcortical activity are indistinguishably integrated.
This unity is reflected in the experience of Oneness with everything, a Oneness with the universe that is oneself.
Space and Increasing Hyper and Hypoarousal
We call man’s symbolic interpretation of his CNS activity “perception-behavior” and regard creative, “hyperphrenic,” and ecstatic states, as well as Zazen and samadhi, as perceptual-behavioral interpretations of ergotropic and trophotropic arousal, respectively.
We may now consider some of the perceptual-behavioral changes, or transformations, that gradually develop as the level of arousal increases and decreases along each continuum. One of the most conspicuous transformations is that of “constancies”, which in the normal state of daily routine form a learned structure of primary ordering of space and time “out there.”
Although the newborn infant’s only reality, in the beginning, is his CNS activity, he soon learns, by bumping into things, to erect a corresponding model “out there.” Ultimately, his forgetting that his CNS activity had been the only reality will be taken by society as proof of his maturity, and he will be ready to conduct his life “out there” in (container) space and (chronological) time.
The adult interprets his CNS activity within this structure of similarity criteria, or “constancies,” and thus experience can be said to consist of two processes: the programmed (subcortical) CNS activity; and the symbolic or perceptual-behavioral (cortical) interpretation, or metaprograms, of the CNS activity.
It should be emphasized that the projection of our CNS activity as location in the physical dimension of space and time “out there” was learned at, and is hence bound to, the lower levels of arousal characteristic of our daily survival routines. All of this is to say that the constancy of the “I” is interfered with as one moves along the perception-hallucination continuum from the “I” of the physical world to the “Self” of the mental dimension; Analogously, the perception-meditation continuum also involves a departure from the “I” to the “Self.”
The further we progress on the perception-hallucination continuum from the normal through the creative, psychotic, and, ultimately to the ecstatic state, the more complete is the transformation, or “unlearning,” of the constancies of the physical dimension. Input, or outside information in general, is gradually reduced along this continuum.
Thus, Saint Teresa of Avila tells us in her autobiography that, at the peak of a mystical experience, “… the soul neither hears nor sees nor feels. While it lasts, none of the senses perceives or knows what is taking place”. Space, then, which was gradually established in ever widening circles during childhood, gradually contracts with increasing arousal and ultimately disappears.
“Self”: The Knower and Image-Maker; and “I”: The Known and Imagined.
At the peak of trophotropic arousal, in samadhi, the meditating subject experiences nothing but his own self-referential nature, void of compelling contents. It is not difficult to see a similarity between the meditative experience of pure self-reference and St. Teresa’s description of her ecstasy: in both timeless and spaceless experiences the mundane world is virtually excluded. Of course, the converge is true of the mundane state of daily routine, in which the oceanic unity with the universe, in ecstasy and samadhi, is virtually absent.
Thus, the mutual exclusiveness of the “normal” and the exalted states, both ecstasy and samadhi, allows us to postulate that man, the self-referential system, exists on two levels: as “Self” in the mental dimension of exalted states; and as “I” in the objective world, where he is able and willing to change the physical dimension “out there.” In fact, the “I” and the “Self” can be postulated on purely logical grounds. See, for instance, Brown’s reasoning that the universe is apparently … constructed in order (and thus in such a way as to be able) to see itself. But in order to do so, evidently it must first cut itself up into at least one state which sees, and at least one other state which is seen. In this severed and mutilated condition, whatever it sees is only partially itself… but, in any attempt to see itself as an object, it must, equally undoubtedly, act so as to make itself distinct from, and therefore, false to, itself.
In our terminology, the “Self” of exalted states is that which sees and, knows, while the “I” is the interpretation, that which is seen and known in the physical space-time of the world “out there.” The mutually exclusive relation between the “seer” and the “seen,” or the elusiveness of the “Self” and the “I” may have its physiological basis in the mutual exclusiveness of the ergotropic (sympathetic nervous system) and trophotropic (parasympathetic nervous system)systems.
Such “I”-“Self” communication is the creative source of art, science, literature, and religion.” _Roland Fischer. “A Cartography of the Ecstatic and Meditative States.”
http://www.born2psychosis.blogspot.com/p/chp-12.html
Lastly, can we consider the cultural aspect of our world-view when look through our varying lens at the same phenomena? Would you consider that your immersion in American culture affects your world-view, in what you can and cannot take into consideration, in a need to belong?
As Peter Levine points out “there is an almost violent schism lurking in our cultural zeitgeist. Lets face it; the fight against evolution by the proponents of “creationism” and “intelligent design” is not really about professed gaps in the fossil records; its about whether or not we are basically animals.”
And yet it this acceptance of my evolved nature and the power of sensation awareness, which sees me drug free and developing and increased ability to go through the process of psychosis to seek its natural metamorphosis. Example:
“THE TRANSFORMATIVE POWER OF SENSATION:
To understand the transformative power of direct sensate experience, it is necessary to “dissect” certain emotions such as terror, rage and helplessness. When we perceive (consciously or unconsciously) that we are in danger, specific defensive postures of protection are mobilized in our bodies. We prepare to fight or flee and when escape seems impossible, we freeze or fold into helpless collapse. All of these are specific innate bodily responses, powerfully energized to meet extreme situations.
These survival energies are organized in the brain and specifically expressed as patterned states of muscular tension in readiness for action. However, when we are activated to this level and are prevented from completing that coarse of action- as in fighting or fleeing, then the system moves into freeze or collapse, and the energized tension actually remains stuck in the muscles.
In turn, these unused or partially used, muscular tensions set up a stream of nerve impulses ascending the spinal cord to the thalamus (a central relay station for sensations) and then to other parts of the brain (particularly the amygdala), signaling the continued presence of danger and threat. Said simply, if our muscles and guts are set to respond to danger, then our mind will tell us that we have something to fear.
Our minds will stay on overdrive, obsessively searching for causes in the past and dreading the future. We will stay tense and on guard, feeling fear, terror and helplessness because our bodies continue to signal danger to our brains. These red flags (coming from non-conscious parts of the brain) will not disappear until the body completes its coarse of action. This is how we are made, it is our biological nature, hardwired into brain and body.
These bodily reactions are not metaphors, they are literal postures that inform our emotional experience. For example, tightness in the neck, shoulders and chest and knots in the gut or throat are central to states of fear. Helplessness is signaled by a literal collapsing of the chest and shoulders, along with a folding at the diaphragm and weakness in the knees and legs.
All these “postural attitudes” represent action potentials. If they are allowed to complete their meaningful coarse of action, then all is well, if not, they live on in the theatre of the body. (p, 183)
Trauma is the great masquerader and participant in many maladies and “dis-eases” that afflict sufferers. It can perhaps be conjectured that unresolved trauma is responsible for a majority of the illnesses of modern mankind. (p, 184)
Trauma is transformed by changing intolerable feelings and sensations into desirable ones. This can only happen at a level of activation that is similar to the activation that led to the traumatic reaction in the first place. (p, 208)
My approach to healing trauma rests broadly on the premise that people are primarily instinctual in nature – that we are, at our very core, human animals. It is this relationship to our animal nature that both makes us susceptible to trauma and, at the same time, promotes a robust capacity to rebound in the aftermath of threat, safely returning to equilibrium. More generally, I believe that to truly understand our body/mind, therapists must first learn about the animal body/mind because of the manner in which our nervous systems have evolved in an ever changing and challenging environment.”
Excerpts from “In an Unspoken Voice” by Peter Levine, PhD.
I believe there is emerging clarity within the latest science, as articulated by people like Allan N Schore & Stephen Porges, and to really help the younger generation, by-enlarge the most educated generation in human history. We need to leave behind old-world language, like “psyche” which is about as helpful in clarifying actual experience, as “chemical imbalance” and get more real and honest about what really makes us tick?
Like how we say that word Evolution, yet fail to embody its essential meaning? Just why are the words “animal & instinct” purged from our socialized definitions, of what is to be a functioning human being? Why has this strange experience historically affected about 1% of humanity? What does that figure mean in terms of our evolution?
Does an existential crisis mean;
“One might say that the Self wants to know itself, or that God is trying to discover himself, the Anthropos we are living in is trying to wake up, the collective unconscious is trying to express itself or the universe is evolving in such a way as to make us more aware of the meaning of life.” _ Mindell (2008)
If we change our metaphors of self-definition to “chemical” will the reality of the the Universe within, begin to make sense? Why an epidemic of divine madness, otherwise known as mental illness,at the beginning of a 21st century A.D.
Perhaps there is a bigger picture, than the immediately obvious reality, we tend to categorize & label? That nit-picking tendency of the left-hemisphere, in search of the Devil in the detail?
With gratitude to your huge effort to shift the focus of debate to where it belongs, in the individual experience of each and every one of us. I do firmly believe we are emerging into a zeitgeist (spirit of this age) in which science and spirituality are truly merging now? Just depends how big our viewing lens is? Are how deep, the subtle sensate awareness?
Report comment
I admire the depth to which you’ve explored this topic! I also appreciate your challenging the Descartian dualistic notion that mind and body are separate. I agree with you very much in this regard, also being a fan of the work of Peter Levine, Allan Schore, and Stephen Porges (though not so familiar with Fischer’s work). In my own psychosis/crisis, by far and away the most important “anchor” that prevented me from drowning in the chaotic hurricane of experience that swept through me was the diligent practice of mindfulness of my own physical sensations. While everything else in my experience was so often out of control and groundless, I could always count on the presence of my body and the sensations within it to keep me grounded to the here and now.
Also, as you alluded to, I also recognize that there is a real challenge in trying to communicate (which requires concepts, which are fundamentally dualistic) about issues that fundamentally nondual. I do believe that such communication is very important, especially around the issue of how best to support each other finding peace in life; however, it helps to keep in mind that the words themselves are not the thing, the map is not the territory.
Thanks for your thoughts and a peek into your own journey.
Paris Williams
Report comment
You might also consider a large Scandinavian study of some years ago that found the only statistically significant variable that differentiated those with a diagnosis of “schizophrenia” from those without that dx, was poverty— Consistent with your existential crisis hypothesis. Also the fact that cultures other than white European or American cultures find recovery rates without medication, far greater and of lesser duration than US & Europe with medication. The concept of “schizophrenia” as a disease is a fiction created by big pharma, the APA’s, and governments to justify repressive and injurious treatment of individuals who are different than, or appear threatening to the mainstream, because of their differences.
Jasenn Zaejian
http://relatedness.org
Report comment
Hey, friends!
I came across this forum by a mentioning on facebook.
I am member of the German user / self-help movement since 1994.
After both my (younger) brothers had died by suicide – the youngest 1987 and the other in 1992 – I started to look for reasons / origins as well as for ways of healing mental disorders. In 1992 I was still afraid that the suicide could happen to me, too.
Today I think I can say that I am healed – although in 1997 i got the diagnosis “Depression” after something like “burn out”. It took abt. 8 years to realize, that I was a “workaholic” and to realize also some other disorders since my childhood.
From 1994 to 2010 I visited at least one self-help-group per week, some periods I visited 2 different ones: One for psychiatry (ex-)users and the other for self-development / holistic health etc.
I feel sure now that I know the most important origins of all mental disorders, consisting of individual AND – in the civilized society – of collective origins.
About individual origins you can find lots of books writing about. But about the collective origins you will not find very much. The main reason for that is that the majority of the scientists / psychiatrists dont have a holistic view of the world, but a “reduced” – typical scientific – view of the world.
Since 1991 I have knowledge about the Collective Neurosis of the civilized society and I named it the “Collective CIVILIZATION Neurosis” (CCN), of which abt. 99,9% of the people in the civilized society are affected.
Let me try to explain what I see:
A) The CCN exists for abt. 10.000 years now, appx. same time as the “civilization”.
B) The CCN went through several peoples, cultures, nations and all of them did FALL. (see: Oswald Spengler).
C) Finally, the Romans brought the civilization AND the Roman religion to the rest of Europe; and from Europe it was “exported” to overseas countries.
a) There is much stress, fear and other negative factors and due to that is a severe lack of spiritual love / life force energy in the civilized society. Due to that, babies suffer – even before they are born. (See: Michael Balint).
All through the years of childhood children cannot build up a really good potential of life force energy.
b) People do not get really adult in the civilized society.
They do not go through the spiritual part of the puberty, like it is still done in non-civilized societies.
The young people do not learn to overcome fear;
they do not get in contact with their subconsciousness, do not get to know their “higher / true self”, their higher dimension / level of consciousness, they do not identify with it, they will not be in a position to dispose of the spiritual love / life force energy and they will not clean their subconsciousnesses from the old suppressions from the childhood.
Due to that, they will NOT get the basis for being really healthy and being unconditional happy.
Having developped the rational thinking does NOT make a real adult.
Sorry for my poor English. I hope you understand what I tried to explain.
We have no choice to ignore the Collective Civilization Neurosis (CCN) or not. Because in distances of a couple of decades the CCN “explodes” in a Collective Psychosis. The things happened between 1933 to 1945 (from Germans’ view) has been called “Collective Psychosis”.
And I think, we should do our very best to avoid another one – expecially because it could be the very last one…
Report comment
Willst du mich verarschen? Ihr Englisch ist toll!
Bitte mailen Sie mir an
[email protected]
I have many questions heureka47
Report comment
I believe that you’ve hit a number of nails right on their heads. However, most Americans have no idea what you’re talking about here. You point out some very interesting things about so-called “primitive” civilizations and what their coming of age irutals do for them. I agree, we are not adults in so many ways. Your English was just fine. Thanks for posting.
Report comment
I also agree with your making good contact with some important nail! I haven’t come across the term “Collective Civilization Neurosis (and psychosis” but they resonate well with me. Thanks for sharing them. Several of the authors whose theoretical models I summarized in my book (“Rethinking Madness”) have also spoken of importance of seeing the often relevant nature of madness, and the ironic question of who is actually more “mad,” the individual diagnosed with a psychotic disorder or the individual who chooses to put his/her head down and blindly conform to the norms and beliefs of a profoundly destructive society.
Some of the authors that immediately come to my mind who have discussed this idea are R.D. Laing, John Weir Perry, Arnold Mindell, Isabel Clarke, and Richard House (most of whom I mention in my book).
Thanks for bringing up this very important topic,
Paris Williams
Report comment
Paris
A great contribution to understanding the true nature of what gets labeled as brain diseases. Both you and Dan Fisher have made a significant attempt to be very scientific about deeply personal and psycyhological experiences of extreme emotional stress.
Questions and comments: You make clear reference to those things in the environmental experiences of people that are more often the beginning of the existential crises that lead to what gets labeled as psychosis. You especially reference several forms of trauma and cite statistics to prove its vital role in producing the conditions for psychological damage. Don’t we need to take things a step further and carefully examine the types of environments that produce the greatest amounts of trauma?
Trauma (except for accidents and natural disasters etc.) does not arise out of a vacume. There are certain economic and governmental systems that produce more fertile ground for personal trauma. Patriachy, racism, poverty,for example, are systemic problems that traumatize people on a daily basis. If we can create environments that radically reduce this type of fertile ground for oppression will we not be taking a major step towards ending the materail basis for extreme existential crises, as you call them? Perhaps you make reference to this in your book.
And on the issue of “consensual reality.” Is there not “consensual reality” and reality itself, independent of any one person’s perception? For example, in this country not so long ago the “consensus reality” was that Afro-Americans were considered inferior. This in itself did great damage to people of color but we can also say it damaged other white people as well, especially poor whites. They were taught to accept their lot in life by looking down on another group of people and it also denied both groups valuable allies in a common struggle against a mutual oppressor.
Don’t we want to create environments (new societies) where the “consensus reality” more closely appoximates the true reality, especially when itcomes to issues of economic and political equality, that is, no institutions that produce material conditions for taumatizing people; environments that reduce extreme states of emotional stress?
Report comment
Thanks, Richard, for bringing up these excellent point.
Regarding environmental factors associated with trauma and other distressing experiences that appear to play a role in the development of psychosis and other psychological distress, I agree with all of the factors you mentioned. The research I have seen has been very clear on the high correlation of poverty, socioeconomic disparity, racism, sexism, heterosexism, etc., with rates of psychosis and other manifestations of severe distress (other types of mental disorders). I think there’s no doubt that if we don’t address these and closely related factors on a broad societal level, then we’ll only continue to see continuation of the epidemic of psychosis and other disorders. And I do go into these issues further in my book; and they also are brought to life somewhat in the narrative case stories spread throughout the book.
Regarding your suggestion that there may be an “true” reality in contrast to “consensus reality,” while I think that this is an interesting topic, I also believe that it’s a real “rabbit hole” topic, that can spin us off into intense philosophical and theoretical debate–such as what we see between the “positivists”/”materialists” and the “constructivists”/”post-modernists.” My own approach to this topic has generally been more pragmatic. Regardless of whether or not there is some “true” reality, there’s no doubt that all societies/cultures and subcultures have constructed their own framework for understanding reality. And different constructions bring with them different harms and benefits. From this perspective, then, we can explore what these constructions are and how well they’re meeting the needs for the members of that group as well as the world at large, and if we’re willing to look at these honestly, then hopefully we’ll be willing to work towards a construction and a set of “norms” that maximize the ability for all members to meet their needs. You can see this process taking place to some extent, as you pointed out, in the gradually increasing rights of minority members and others who are similarly marginalized. However, unfortunately, we often seem to see movement in the other direction–increasing the benefits of the few at the expense of the many. Democracy has been an attempt to minimize this latter movement from happening; but unfortunately, it seems we have a long way to go before we have a real democracy…
Paris Williams
Report comment
Your point was so important, the power systems that rule us, in many ways, breed the mental health problems of society and when there is an overload, they put the mentally ill into prisons for there is nowhere else to put them.
Report comment
Paris,
I am currently reading your book, Rethinking Madness, and must thank you for articulating a scientific challenge to the erroneous medical model of biological psychiatry! It is unfortunate that their pseudo-science dominates psychiatry and psychology since it is so counter-productive!
I agree thoroughly with your assessment that psychosis is a product of natural, “normal” biology, and that psychosis is a desperate response to an intolerable situation. I also agree with your criticism of dualism.
However, I believe that natural, “normal” brain biology produces psychosis as a natural reaction to intolerable situations for natural purposes, as part of a process that promotes species survival.
Thank you again for your community service in writing Rethinking Madness.
Best wishes, Steve Spiegel
Report comment
Hi Steve,
I think that’s a really important point regarding psychosis/extreme altered states as having the potential to offer great benefit for the evolutionary process of our species. Several of the different theoretical models I presented in Rethinking Madness integrated this idea, and I also mentioned it in the Conclusion. I believe it was R.D. Laing who said that the “mad person is drowning in the same ocean in which the mystic is swimming.”
We find evidence in virtually all indigenous societies of people who go through powerful transformative processes which take them well beyond the confines of consensus reality (e.g., “shaman illness,” etc.). And these people are generally highly respected, as they are considered to take on a very important role in these societies–holding an understanding of the world beyond the confines of consensus reality, which offers the potential for great individual and social healing, and also ensuring that the society doesn’t become hopelessly stuck within an inflexible, dogmatic paradigm.
It’s unfortunate that in Western societies, we have generally lost our respect for this important role, either trying to force such individuals back into consensus reality or seriously marginalizing those who are unable or unwilling to do so.
One tragic result of this is that, in the West, those who do drift outside of consensus reality and find themselves beginning to “drown” in these deeper waters rarely receive the support they need to learn how to “swim”; though miraculously and thankfully, many still learn how to do exactly that. This is a major part of my own personal vision of a genuinely supportive mental health care system–utilizing the wisdom from those who have “been there” and have learned how to swim to support those who are still on the verge of drowning. This is why I am such a big fan of Soteria-type houses, peer support groups, the Windhorse project, and Open Dialogue/systems approaches. Rather than just condemning these individuals to a life of isolation and stigmatization, these alternative approaches honor the potential for positive growth and transformation within these experiences, as well as recognize that these individuals often act as the canary in the coal mine for serious problems occurring on a larger systemic level, such as within a family, a community, or even an entire society.
Paris Williams
Report comment
Paris,
I’ll head back into your book to better understand your perspective of psychosis as it relates to evolutionary theory.
I certainly agree with your vision of a genuinely supportive mental health care system! The current system is typically counter-productive because it has little understanding of the experience of psychosis and provides little true empathy.
Best wishes, Steve
Report comment
My experiences (three episodes of psychosis and a diagnosis of schizophrenia) exactly tally with your theories. I did undergo childhood trauma – and I smoked dope – I found myself in an impossible sitation socially, financially and emotionally as a young person, and consquently I broke down.
I recently learned that anxiety is often at the root of psychosis – I wish I had known this when I was younger, because I had no idea that the high state of anxiety I lived in, and the panic attacks which often engulfed me, were what made me susceptible to further breakdowns.
I have been relatively well for a long time now – I have taken no medication for about eleven years and I have a husband, young children and a wide circle of friends – but the final step in my healing came recently after a course of cognitive behavioural therapy which helped to lay my anxiety to rest.
The other thing that helps me nowadays is to believe that there is a higher purpose to this life. I baulk at formal religion – one set of tenets seems as good as another to me as long as they are based on kindness, compassion and so on – but it helps me to believe that there is a God of some kind, a reason why we are here, a plan. None of us knows what will happen when we die, but it seems to me that there must be some further element to such a rich and varied world, and it gives comfort to hold this thought. It seems harmless, and it helps!
All the best
Louise
Report comment
Thank you for sharing your inspiring story. It sounds like you would have really appreciated some helpful direction a little early on, but in reference to what I just wrote in my post above, it seems clear that even though you were on the verge of “drowning” for a long time, you have finally learned how to “swim” and ride the rapids of life with some confidence. Very inspiring. Thank you,
Paris Williams
Report comment
“I have taken no medication for about eleven years”
Very good. You’ve got it figured out. Congratulations.
Report comment
Hi Paris,
As you know, I am very sympathetic to your model, especially to the idea that madness involves a process of experimenting with different ways of looking at the world in a fundamental way. I was happy to see you summarize your model in this blog post. I think “nutshell versions” of theories can be very important in influencing the ways people think, so I wonder what you think of the following summary I wrote this morning:
What we see as madness is typically the result of a process of experimenting with different ways of understanding or looking at the world, and different ways of approaching the world and of behaving, that don’t appear to be working out well to either the person or to those around him or her, and in which the person seems to be entrenched – either unwilling or unable to change.
It may seem strange to associate madness with a process of experimentation, when so many who are labeled mad appear caught in repetitive patterns, and they don’t seem able to experiment with ways of getting out of those patterns. But this avoidance of experimentation can be understood as also the result of having experimented and then suffering from the result, and fearing that more experimentation would lead further into the abyss. Fear of madness, fear of one’s own creativity and imagination, becomes a key part of the madness.
Society manifests its fear of madness by supplying antipsychotic drugs, and these drugs themselves inhibit experimentation, and keep people stuck in repetitive patterns. They seem to “work” when they keep people from doing further experimentation that causes trouble, but they also inhibit the continued experimentation that is needed in order for the “lost” to find their way to a pattern that works, to recovery.
I think this summary is consistent with your model, while maybe going a little further to explain some of the patterns we see in “chronic psychosis” and in “negative symptoms.”
Report comment
Beautiful, Ron. This resonates very will with my own personal experience. I recall being stuck for a long time in very confusing and powerful cognitive and affective patterns–patterns that I had clearly generated myself by my own experimentation (some quite conscious, others more semi-conscious)–and not knowing how to get out. In other words, finding myself in a place where I felt like I couldn’t (and didn’t really want to) go back to where I was; and yet the way forward also appeared extremely precarious and frightening. There really was a sense of being suspended over an abyss of unimaginable “madness” and that the wrong move would send me plunging headlong into it–absolutely terrifying at times. Yet at the same time, there was generally a sense of hope that there was the potential to find real peace and resolution if I found the courage to continue moving ahead.
During that time, there were two “mantras” that I used to maintain my courage:
The first was a constant reminder to myself to maintain a two-fold intention with regard to my present experience–awareness of present experience (primarily body sensations, as these were the most grounding), and equanimity/acceptance of my present experience (any struggle against present experience at that time immediately led to intense suffering). This intention seemed to be the only thread at times that prevented me from falling into the “abyss.”
And the second mantra was a constant reminder to myself that “the way out is through.” As you mentioned with regard to the use of antipsychotics and attempts to bring an individual back to consensus reality, it was all too clear to me that trying to go back or trying to force this process to stop prematurely would only keep me in this “lost” condition indefinitely. I knew I had to keep going forward, which within the context of your post, meant continuing to maintain open eyes and open arms and a willingness to remain open to new and often further ungrounding possibilities regarding the nature of myself and the world, with the faith that this path would eventually take me to relatively peaceful and stable ground once again–which thankfully it has!
Paris Williams
Report comment
This gives me so much hope as a mother, my son talks about the need to keep pushing. Reading that this was your mantra and hearing the same from from my son will sustain me on our journey.
Report comment
I often hear music in my head. What is the diagnosis?
Report comment
It depends on how much you like it 🙂
Report comment
Music creator.
Report comment
Good article, but you’re missing the biological causes that are linked to mental illness: chronic inflammation and glutathione depletion.
Report comment
When we observe an anomalous mental experience co-occurring with an anomalous physiological condition, I think it’s really important that we ask ourselves–is this causation, or is it simply correlation? …and if causation, what is the direction of the causation? Leaping to conclusions in this regard very often leads to serious problems, IMHO.
Paris Williams
Report comment
I have been told by other readers that our perspective is in harmony and I can see from reading this op-Ed and the comments following it that indeed it is true. I am only sorry that as far as I know, and judging by your references, that you have not referenced the most important recovery research, by our recovery movement. I do not say this to detract from your important contributions. I say it more from the hope that you can join with our movement in its need to deeply question the dominant paradigm.
One note about the first existential dilemma you state , the need to balance between autonomy and connection. I have come to realize this may be based on a false dichotomy. The longer I live and experience the more I find that it is precisely deep, loving connection which makes autonomy possible. As my two daughters move great distances from our home, I believe it is because they feel securely rooted in the love that my wife and I have given and continue to give, and receive from them. I have also concluded that most deep emotional distress is based on failures to achieve the security of love which I feel supersedes most cognitive paradigms. Pierre Tielhard de Chardin posited love was the source of all life and I would agree.
Report comment
I’m happy to hear from you, Dan. I am familiar with some of your work and the National Empowerment Center, and I really admire and appreciate all that you’ve done.
I’m not sure of the recovery research you’re referring to–can you please direct me to it? In my book, “Rethinking Madness,” I referred to every major longitudinal recovery study that I was able to find, though I’m aware that there are many other equally valid types of research (such as biographical and autobiographical accounts), which I generally referred to and/or directed readers to, but of course couldn’t cover all of it.
Regarding your suggestion of the “autonomy/connection with others” dilemma being ultimately a false dichotomy, with love essentially bridging the gap and ultimately cutting through this dilemma altogether, I couldn’t be in more agreement with you. This is why I termed the model I present in “Rethiking Madness” the “Duality/Unity Integrative” model, suggesting that we find ourselves in an apparent paradox that some of us have more or less difficulty coming to terms with: On one hand, there is clearly some validity to the subjective experience of myself (“self”) being separate from “other” — in other words, a dualistic experience in which I find myself with needs related to both autonomy (those associated with “self”) and also relationship (connection with “other). On the other hand, however, it appears that there is a deeper truth/experience that transcends this dualistic experience–the truth of fundamental interconnectedness (associated with feelings of unconditional love, selflessness, compassion, etc.)–an experience I refer to as “unity”. And herein lies the second dilemma: how do I maintain a sense of “self” in a world that is so fundamentally interconnected and nondual (selfless). And I believe this is also why we have the capacity to experience both profound terror (terror of the loss/disintegration of self) as well as profound unitive experiences (the bliss and freedom associated with a loosening of our isolating ego/self) when we contact the world at this deeper, more “raw” level.
These concepts can be a little challenging to grasp, particularly because the very “concept” of unity is beyond concepts altogether (concepts being fundamentally dual), and yet I believe these are at the crux of what occurs within psychosis (as an individual finds oneself “drowning in” and desperately attempting to integrate these core existential dilemmas. And indeed I believe these same dilemmas/experiences are at the core of all human experience, whether or not it is considered “sane” or “mad.
I didn’t have the room to go into these ideas here in this short article; however, I go into them in great detail in “Rethinking Madness,” where I attempt to bridge both Western and Eastern understandings of human experience, as I believe Western psychology has contributed greatly to the self/other dilemma, whereas the existential contemplatives of the East have contributed greatly to the exploration of unity/no-self/nonduality.
I plan to look at your own recent post and comment on that within the next day or so. Thanks for your interest in my work.
Paris Williams
Report comment
Paris, Thanks, very interesting and I look forward to reading your book.
My other question: have you cnnected to our consumer/survivor movement. California
Has a long tradition of speaking up to the abuses the system perpetrates
ThNks especially to the persistence of the false medical model.
Your insights could help in our historic struggles. I can connect you
As far as other research I am referring to the interviews we carried out
at the the NEC which we used to explore the factors essential to recovery.
We incorporated them into our recovery training project, Personal
Assistance in Community Existence (PACE). It was published and is
On our website. Mainly though we used the data to advocate for
Recovery and establish the concept in the New Freedom Commission
Report. The rest of our research has been in personal stories of
recovery as we want to give hope and counter hopelessness.
Report comment
My son was diagnosed SZ in 45 minutes and is on antipsychotic medication. For a few years prior to his diagnosis he exhibited many behaviours which caused me concern. I turned to the medical profession as a concerned mother and because I thought it was the right thing to do. I now realize it was a HUGE mistake. I have alway felt that he was undergoing a spiritual crisis, he was an overly scrupulous child and was very conscious of doing what was right. Because of this scrupulous thinking he continues to take anti psychotic medication because he feels that his psychiatrist is a trained professional and knows more than he does. I woe the day I got involved with the medical system and am now desperately trying to back track.
The challenge as a mother is recognizing what my son is going through and finding the systems that can assist him in dealing with his psychosis.
Report comment
Thanks for sharing your story. I’m sorry to hear of the difficulties you and your son have gone through. It can be difficult to find non-“medical model” support for people struggling with distressing anomalous experiences, but there is such support out there if you take the time to look for it (such as peer support groups, therapists who practice alternative approaches, and alternative residential facililities).
You can begin by looking at my own resource page here:
http://rethinkingmadness.com/#/clinicstherapists/4563430115
…and on the resource page of this website (“Mad In America”) here:
http://www.madinamerica.com/resources/
…also if you send me a personal confidential email with your son’s location, I can put the word out to other alternative therapists/psychologists/psychiatrists who may be able to work with him. For my email, go to:
http://rethinkingmadness.com/#/contact/4540113778
Paris Williams
Report comment
I hear voices – it is definitely not a passive experience. Nor is “hearing voices” passive language: it is simply descriptive of a wide range of experiences that many of us have in our lives. And believe me saying publicly “I hear voies ” is far, far from a passive act: requiring a deal of courage and confidence and is an asserting self over dogma and oppression. It is perhaps a shame that some amongst us find it necessary we all agree a single terminology: I don’t understand what tdrives some to have that need in themselves. Some of us think that there are seven billion unique expriences of being human alive right now and that this offers a richness of understanding that a single precisely worded tightly controlled definition ruber stamped by some self appointed committee cannot. Would that not be same operational dynamic that’s gotten us into this unholy mess in the first place? To have one group insisting their understanding is the “right one” and all others must adopt? We already know what that world looks like and I for one want a different one. One of the key strengths of “hearing voices” as an approach approach is that people are free to make their own understanding of their voices, yet whatever that is, the approach can still work. It is neither a fix nor a therapy. Whatever the cause of the voices I hear – and there are many voices and likely at least a few causes, what I’ve learned to change is the way I treat them and so in turn the way they are with me… in other words what’s changed is my relationship with them. Where they actually come from makes no significant difference in that. You could, should you choose, make a semantic argument that I learned to shift from hearing my voices to listening to them, from trying to ignore and fight them to working with them and getting them to work with me in a way I can work with so I can figure out and interpret their meaning. You could, if you like make a argument that that is shifting from “passive” to “active” stance and if you want to then go ahead: your choice. I wouldn’t want to tell you how to describe your experience, I’d be grateful if you’d offer equal respect and allow me and others who hear voices to do the same and simply choose our own language to describe our own experience. Kevin
Report comment
Hi Kevin, please help me understand. I don’t recall ever saying that hearing voices or any other anomalous perception is “passive.” Quite the contrary, my suggestion is that as living organisms, all of our behavior is quite meaningful and entails very “active” responses to the world and to our experiences in an attempt to either cope, heal, grow and/or ultimately thrive. And I am all for people developing their own understanding of their experiences, whatever they may be. My entire thesis here is an encouragement to reject the rampant inculcation of the “brain disease” theory of anomalous experiences as if it’s “fact,” and encouragement to everyone oppressed by this dysfunctional system to reconnect with their own truth and reclaim their power. (Of course, if someone chooses to believe that their anomalous experiences are the result of a brain disease, then who am I to convince them otherwise, though I am likely to ask them how they came to such a conclusion, and challenge them to consider if that really is their own truth, and not an introject of someone else’s.)
Here’s an article on the factors of recovery that have emerged within my own research that I think you may appreciate:
http://brainblogger.com/2012/05/29/full-recovery-from-schizophrenia/
Paris Williams
Report comment
…btw, I appreciate your sharing that your own recovery process has consisted of changing your relationship with your voices (or other anomalous experiences), rather than “getting over” them. This is very much in alignment with how I like to define “recovery”: “The condition of experiencing a diminishment of the distressing and/or limiting aspect(s) of one’s anomalous experiences, and not necessarily the diminishment of the anomalous experiences themselves.”
It sounds like you’ve come a long way with making peace with these experiences. Your story’s an inspiration to me and I imagine to others who are challenged by similar experiences,
Paris Williams
Report comment
“The mainstream paradigm of care may actually be creating a self-fulfilling prophecy of brain disease
While we continue to have no solid evidence that schizophrenia/psychosis is the manifestation of a diseased brain, we do discover one particularly tragic irony in that our very entrenched belief in this theory and the paradigm of care that has resulted from it is actually ensuring that enormous numbers of people actually do develop brain disease (see Figure 1).”
BELIEF = POWER? Power to cause and create? Scientific fact?
Hallucinations are quite real, by the way. Illusions are also real. It makes no sense to say that a hallucination is “not real”. If it was not real, no person would ever be able to experience a “hallucination”. Because we are able to experience a hallucination, something is very quite real about it. Same with illusion. Illusions exist; we are aware of them, we can experience them and we can explain them. Typically, we never ever forget a “hallucination”. We will always remember it and it becomes a permanent part of our reality.
Everything has a basis in reality. It is not correct, nor is it considerate, judicious or fair, to call a person “disordered” or “diseased” when they experience that eerie, fantastical, terrifying, supernatural part of life that we so WISH was not real or true.
Refer to Deepak Chopra who wrote a book about a spirit manifestation that accompanied him for 4 days. He is my FAVORITE example. Is he is a liar? Delusional? A severely mentally and psychologically handicapped person?
http://www.equip.org/articles/dangerous-spirituality-for-teens/ “At the end, Chopra realizes that Baba is just an extension of himself. This is not hard to believe given that what Baba teaches here corresponds with what the adult Chopra has taught for years.”
If Deepak Chopra is not Judged by the world as a sick, “insane”, delusional, psychotic man – should he be, or should we not be?
—
My own personal choice term / word for “psychosis” and “psychotic” is “psyche-active”. I chose this descriptor because the vowel sound between “o” and “e” changes the vibrational energy AND the mind-set. “E” is higher; “O” is lower.
I have a serious problem being called “psycho”. The word “psycho” makes me violent; it is a source of abuse (which is socially acceptable). The words psycho and psychotic cannot and will not ever be conducive to a state of Health.
Psyche-active is EASE and constructive. Psycho and psychotic are dis-ease and destructive.
If Obama changed “mental retardation” to “intellectual disability”, then psychotic and psychosis can also be renamed. The words we use make all the difference in the world. We are FORMED by words (information). Words can hurt. Words can heal.
Oh. And illusion artist such as Mind Freak and David Blaine are experts on the Laws of Nature and Universe, which is what allows them to perform acts that we call “illusions”. There is a real science to what they do, and what they do is miraculous. It is quite possible that some MENTAL people have raw, natural talent, skill, gift and ability – and they aren’t even aware of it – or they’re brainwashed into believing they’re sick, wrong and mentally handicapped.
What if schizophrenia is a lack of vocabulary and articulation, and psychosis is spiritual travel through acid warped realms and dimensions that all too easily blend with ground-level reality?
Maybe psychologists need to study parapsychology, atmosphere, air and gravity. Levitation is not the breaking of the Law of Gravity; it is the utilization of the Law which allows Levitation.
Report comment
You have some good points here, many of which I resonate with, but it seems you are misinterpreting some aspects of the points in my article, so I’ll try to clarify these here:
Regarding this quote from the article:
“While we continue to have no solid evidence that schizophrenia/psychosis is the manifestation of a diseased brain, we do discover one particularly tragic irony in that our very entrenched belief in this theory and the paradigm of care that has resulted from it is actually ensuring that enormous numbers of people actually do develop brain disease (see Figure 1).”
…what I mean is that the main treatment methods (toxic drugs, ECT, etc., are well established to cause long-lasting and sometimes permanent damage to the brain.
(2) I never try to claim what beliefs/perceptions are “real” and which are not. In fact, to the contrary, I’m using language such as “consensus reality” and “anomalous beliefs” to try to step away from the debate about what’s real and what’s not, and simply acknowledge that every society or group of individuals tends to have an consensually agreed version of reality (“consensus reality”), and that many members of these societies/groups diverge significantly from these in their beliefs or perceptions (“anomalous beliefs and perceptions”). I’m suggesting that all beliefs and perceptions are individually constructed attempts to make meaning of the raw data we take in from the world, whether someone is considered “sane” or “mad.” The beliefs/perceptions of the “sane” ones just happen to be more in accord with “consensus reality.” Who’s to say what’s actually “real.”
What I think is most important is not to try to determine whose truth is most “real,” but rather how effective one’s truth is in contributing to meeting one’s needs and creating a sustainable and fulfilling life.
Paris Williams
Report comment
I was honing in on “belief” specifically, and not methods of treatment. I should have been more clear, since I quoted the entire paragraph instead of the piece that I took from it.
—
If people believe that I’m sick, they will treat me like I’m sick and I will be empowered by that energy and I will actually BE sick, in part or in whole.
If people believe that I’m healthy, they will treat me like I’m healthy and I will be empowered by that energy and I will actually BE healthy, in part or in whole.
There are emotions and beliefs about Deepak Chopra which ALLOW him to have a spiritual manifestation (hallucination) without being considered a sick man.
Deepak Chopra is a CRAZY man! and if people BELIEVED that about him, they would effectively CREATE him to be exactly that. They would treat him like a sick man who is not to be believed, and they would demand that he needs help (help to make him stop having hallucinations, because hallucinations are a sign of SICKNESS and DISEASE). People would not buy his books and his entire world would crumble.
His life would be destroyed. HE would be destroyed.
If people BELIEVE that hallucinations are a disease and disorder, they haven’t met Deepak Chopra. If it isn’t a disease or disorder for him, then it isn’t for us either.
—
One universal aspect in “schizophrenia” and “psychosis” is that we are said to experience a sort of “non-reality”. If something is “non-reality”, it cannot be experienced. Since we CAN experience, there is something REAL about it.
While driving, I had a disembodied, external female voice speak from behind my left shoulder. She said, “accident”. Less than a minute later, I saw the accident but could not avoid it. Crash!
The voice was NOT “non-reality”. The voice IS reality. If somebody said, “there was no voice” – I would say that person is in error. If there was no voice, I would not have heard anything.
The “voice” could not have been a “hallucination” because hallucinations CANNOT BE CORRECT. And if it IS correct, it is not a disease or a hallucination – it is something else.
—
In another long, drawn out story (meant to illustrate a few things) – I’ve been “invisible” to people. Huh? That doesn’t make sense, right?
I was standing directly in front of people, jumping up and down and waving my arms, but they didn’t notice me. WHY?
That was actual reality. That actually happened. No, I wasn’t “dreaming”. I know how and why the people failed to see me, though. None of us were diseased or disordered. Nothing was “wrong”, but there was a gigantic space ship in the sky! O.o
Except that when I change the words, it changes the mind-set: there was an AIR CRAFT in the sky. It was remarkable. And real. And terrifying.
But it wasn’t so terrifying FOR ME, actually. I was astounded and I felt electrified. I jumped up and down, waving at people who were driving by in their cars. I stood there on the sidewalk in front of my house yelling at them to look up at that gigantic, hovering thing – which I kept pointing to. Not only were they not looking at IT, but they also failed to look at me!
They appeared to be in a trance and it was because of their chemistry. They KNEW something was in the air. They could feel it – sense it – just as I did. I was washing dishes or something when I suddenly “felt something”, so I instinctively looked out the window. WOW. I ran outside and had the show of a lifetime!
It was one of the most amazing experiences in my life. It wasn’t a delusion, mass hallucination or any other “mental” psyche-trick. It was an absolute reality.
NO, I was not “seeing things” – where “seeing things” implies that something is “not there” when it actually IS there.
*** It is a matter of the people who DON’T see what they SHOULD be seeing. And the people who failed to see me and that freak air craft thing were in shock: a natural, fear-based, chemically induced hypnotic trance ***
I had an absolute BLAST! It was AWESOME!
BELIEVE ME? Do you believe my story? It’s all real and true. But the common, average, every day person would verbally attack and abuse me – calling me nuts, crazy, schizo, psycho, etc. – while “doctors” and “professionals” would use their “proper” language for those violent terms.
Sigh…
It took very many years for me to process that experience. I concluded that it is entirely logical, reasonable, rational, possible and MOST LIKELY that the air craft was by Human Design. If human beings can create incredible space shuttles, they certainly CAN create low, hovering air craft with pretty lights.
I <3 you, Deepak. Stand up for me – I'm tired of being trapped in negation (Hell). And psychiatry? FKU.
Report comment
“. . . in certain cases, [the loosening of our cognitive constructs] . . . . can lead to the potential benefit of having a more open mind (less rigid belief systems) and the richness of experiencing a greater sense of interconnectedness with all . . . . . but on the other hand . . . .can also lead to the potential terror of experiencing just how precarious and ungrounded our existence and self really are . . ”
the “loosening of our cognitive constructs” can be achieved artificially by the use of psychotrpic drugs, but it is important to realise that states of mind so induced only mimic, and cannot be equated with, psychosis. Furthermore it is important to understand that the term “schizophrenia” was coined by the German psychiatric tradition over a century ago in an attempt to delineate what the tradition’s practitioners, through very painstaking observation and listening to the subjective experiences of many hundreds of patients, (remember there were no antipsychotic medicines then) saw as one particular and relatively rare, but very personal-independence-crushing and chronic type of psychosis. So “schizophrenia” as such has only been with us for little more than a century, but madness, which the term schizophrenia was an attempt to understand a little more systematically, has always been with us. The German tradition regarded schizophrenia as pathologically understandable and conceptually separable from the vast majority of other forms of psychosis, many of which undoubtedly can be understood in terms of life crises and stresses.
Mr Williams now asks us to reconsider these attempts to delineate madness along psychopathological lines, and instead in some ways return to a more amorphous pre-nineteenth century madness concept, and then understand it, not in the light of any kind of pathology, but instead in the light of what he calls the “existential dilemmas” of being a human being in the world.
Now I’m not sure that the first of the two dilemmas he outlines really qualifies as an existential dilemma, but let that be; it’s the second which is altogether more interesting, and more probably would, in Sartres understanding of the word, qualify as an existential dilemma. This, as I understand it, (and I have worked full-time for over 25 years with hundreds if not thousands of the very most chronically disabled schizophrenia-afflicted persons) pertains to the very core of the schizophrenic experience. These people generally cannot pull themselves up by their own bootstraps from the swamp of psychotic chaos and confusion, as has Mr Paris Williams and thousands of others who, like him have experienced Recovery with the big R, because if they could then they surely would have done so.
And, I’m sorry to say, it very rarely is a help to these people to take the position that they simply are overwhelmed in a wrestling match with this existential dilemma, and just need to be shown the deeper meaning of their psychosis, in order to be able to “live it through” so as to come out the other side a stronger and richer human being. (Sigh!) It’s a lovely idealism – if only it had anything to do with the terrible reality of this disability.
Paris Williams defines (rather weakly in my opinion) the dilemma thus:
“The need to maintain a relatively secure and stable sense of self when the very fabric of one’s being and indeed of the entire universe is profoundly groundless, impermanent, and interconnected.”
This definition seems to say everything and nothing all at once, but if we fillet out the two key elements, “stable sense of self” and “fabric of one’s being ” then we can immediately relate this to what seems give the schizophrenic such extraordinary difficulty in navigating the relational aspects of what should be (and indeed are for most of us) the most simple social interactions. It is perhaps not so much that the sense of self is lacking but more that the sense of self in a profoundly solipsistic way permeates everything within the schizophrenic’s range of sensory and intellectual input. A schizophrenic man with quite marked ideas of omnipotence I once went out for a walk with, replied to my comment about it being a fine day, “Thanks.” He took my comment as a compliment since it was implicitly understood that he was responsible for the fine weather.
In some quirky way you might almost say that a more stable sense of self you could not wish for, and as for the fabric of his being it was as if he felt that the fabric of the world was the fabric of his being. And it does seem that this is the core of the schizophrenic subjective psychotic experience. The schizophrenic is not in and of this world, but almost the other way about – the objectivity of the world is somehow irrelevant to the schizophrenic, because it is the subjective experience alone which has any meaning. Thus anyone at any time can get some fleeting idea about “being watched” but we almost immediately and without thinking refer such ideas to our inbuilt reality testing apparatus, and quickly dismiss them if there is nothing real to build them on. But to a schizophrenic just the fact that such an idea could arise in consciousness is in itself profound and therefore meaningful, and he will therefore build freely upon it without any concern about reality, until he becomes fully blown paranoiac.
I would say that Paris Williams little diagram (figure 1) is very misleading, because not since Emil Kraepelin’s preliminary description of schizophrenia as “dementia praecox” back in the nineteenth century, has mainstream psychiatry regarded schizophrenia as a dementia or progressive degenerative brain disease. Indeed it is well known that schizophrenics as well as anyone retain cognitive function into advanced age; it is just the ability to put these functions to use in any socially cohesive context which is lost.
To his credit Paris Williams does ask the pertinent question:
“So, if these existential dilemmas are universal, then why do some individuals become more overwhelmed by them than others, and go on to develop psychosis?”
Yet part of the answer he comes up with –
“it appears that . . . . .some individuals may even have some genetic or developmental predisposition for such experiences. ”
. . seems more or less precisely to abrogate his very own argument for a biologically free understanding of the phenomenon generally known as psychosis, and in particular that specific form of psychosis known as schizophrenia. For I would definitely argue that it is precisely this “genetic or developmental predisposition” (notwithstanding the fact that scientific investigation into this complex area is far from complete) which accounts for why it is that only “some individuals” and not every individual who grapples with the existential dilemmas Williams outlines, “go on to develop psychosis (more precisely schizophrenia)”.
Big Pharma has undoubtedly much on it’s conscience, but one of the things it does not have on it’s conscience is the invention of the schizophrenia diagnosis. This took place in an era before Big Pharma even existed. And even if it is true (and I believe it is so) that science has no incontrovertible evidence to back up the thesis that schizophrenia is solely down to dysfunction in the brain’s biochemical signal system, then it is equally true that there is just as little evidence to back up the thesis that schizophrenia is nothing other than the “manifestation of a mind deeply entangled within the fundamental dilemmas of existence.”
Report comment
Paris,
Excellent work and thanks for sharing here. I look forward to reading Rethinking Madness. –Vanessa
Report comment
Paris,
Thank you for your work and perspective. I find your work both very clear and profound. Hope you can make your way to New York one of these days:)
Report comment
Dear Dr. Williams,
Thank you for your work, it is important and needed in a era where SSRIs rule psychiatry and fill the pockets of Big Pharma. My brother has schizo d disorder (or so they say). I tried to apply your ideas to his life and it works, I pinpointed the dilemma, its manifestation, and how he dealt with it. He was a young teenager, but psychiatry quickly moved in and drugged him like no tomorrow.
Now, years later (and after being hospitalized more than once), he is finally stable, yet he still never went back to school and remains without a job. The schizophrenic thinking has largely ceased, but the OCD is unrelenting and debilitating.
My question for you is that, you mentioned that “The long-term use of antipsychotics increases the likelihood of the development of a chronic psychotic condition and significantly reduces the likelihood of recovery”
Do you think that is what might have occurred in my brother’s case? I am not asking for medical advice so please do not shy away from my question, simply your opinion.
You see, I feel that when the dilemma occurred, we could have dealt with it properly, but instead, they medicated him and now here we are years later, he is 32 years old, and I do not see a way back. Olanzapine is his staple and now they are trying SSRIs to deal with the OCD, which is not working at all, we have tried everything.
He is highly functioning, incredibly intelligent, he could talk to your for hours about life and philosophy, but he is essentially stuck, and he has so much hope that another concoction could alleviate the OCD, but nothing seems to help.
Any thoughts?
Thank you kindly,
Lisa
Report comment
Paris – I found this very worthwhile, most especially since your reduction or condensation of the existential dilemmas to the two dualities isn’t carved in stone: various syntheses and rewordings stay available for moving back and forth perspectivally between the discourses.
One thing that struck me in the first part was the substantial shorthand component to the phrase “relationship with experience”. Relationship with feelings may sound more basic, but which relationship is more fundamental. Simply discovering that Sartre puts feelings themselves legitimately into the category of possessions changed my ability to relate to my experiences. But getting away from the system takes unbelieveable effort, and not getting away prevents natural healing and growth. I cannot believe the pretense about this in the caring professions.
Thanks for staying on the hook and opening pathways to something better. You have sold me on your book.
Report comment
Where was this just linked to make it so suddenly popular after all this time (not that I’m complaining)?
Report comment
The CrazyWise Facebook page on 2/23/17:
https://www.facebook.com/CRAZYWISEFILM/posts/1136530239802288
Report comment