This week a commentary, written by members of the University of Pennsylvania Department of Medical Ethics and Health Policy and titled “Improving Long-term Psychiatric Care: Bring Back the Asylum,” was published in JAMA Online. The senior author, Ezekiel Emanuel is former Special Advisor for Health Policy in the Obama administration and brother of Rahm, Mayor of Chicago and Obama’s former Chief of Staff. This commentary with its provocative title published in a high impact journal by a well connected physician is sure to garner considerable attention and influence.
As the title suggests, the authors recommend a return to asylum care, albeit not as a replacement for but as an addition to improved community services and only for those who have “severe and treatment-resistant psychotic disorders, who are too unstable or unsafe for community based treatment.”
The authors seem to accept the notion of transinstitutionalization (TI) which suggests that people who in another generation would have lived in state hospitals are now incarcerated in jails and prisons. This notion arose from two sets of statistics. The first is that as rates of psychiatric hospitalization declined rates of incarceration increased with the total in 2000 being about the same as it was in 1960. It gives the appearance that we just transferred people from one setting to another.
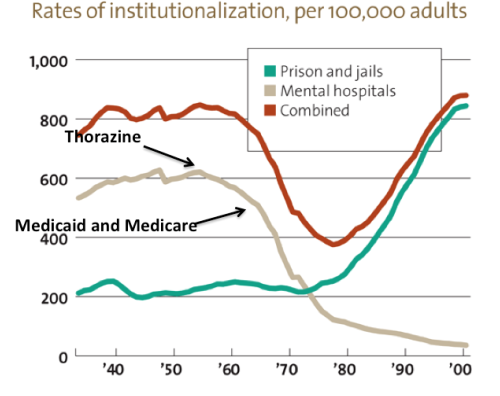
The other statistic referenced is the high rate of mental illness among those who are incarcerated. The JAMA authors conclude that we can not escape a certain level of institutional care. They are ethicists who argue that it is more humane to place those with mental illness in psychiatric hospitals than jails. Hence the call for asylums.
I have never been comfortable with this hypothesis because it did not comport with my experience. Although I knew that many in our state prisons were prescribed psychiatric drugs, their reasons for taking these drugs were not the same as those who were in our state hospital. The conditions they had fell more into the categories of substance abuse and dysphoria. Whereas the problems of those in our state hospital fell more into the category of psychosis. And while in the early 2000’s Seroquel was the most expensive cost for our state prison pharmacy, it was not by and large being used to treat psychosis; it was mostly prescribed as an alternative to benzodiazepines to treat insomnia and anxiety. At the time, this new (and highly promoted drug) was considered to be a safer alternative to the addictive benzos.
I wondered whether my experience generalized to our nation’s larger states and cities so it was with interest that I read the excellent series of posts by the blogger 1 Boring Old Man (here, here, here and here). Whereas in an earlier post he seemed to accept the notion of TI, he did some research which confirmed my impressions: it is simplistic to assume from the rates of institutionalization that prisons and jails have replaced state psychiatric hospitalizations. He cites several studies, including a comprehensive report by Seth J. Prins who researched the incidence of mental illness in prisons and jails. Prins found that much of the data are weak and based on self report but his conclusions supported my general observations.
It is too bad that Emanuel and colleagues did not look at this work. It appears that the authors of the JAMA commentary were influenced by the work of the Treatment Advocacy Center. Their first referenced article is by E. Fuller Torrey and Jeffrey Geller. The authors also give a nod to the hospital that Geller has recently helped to open in Massachusetts, the 320 bed Worcester Recovery Center and Hospital.
It is tempting to stop here. But I would not be honest if I did that. For I am living through a transition in Vermont and I see both sides of a certain dilemma. The authors write, “Even well-designed community-based programs are often inadequate for a segment of patients who have been deinstitutionalized.” While I am not sure they are right, I am also not sure they are wrong.
Three years ago, Hurricane Irene closed Vermont’s 50 bed state hospital in one eventful night. The hospital had been struggling for awhile. It lost its Medicaid certification in 2002 and for the next 9 years there was debate over what do. Many advocates claimed we did not need a state hospital while those on the other side argued we could not survive without one. There was no resolution until the legislative session following the flood when the discussion was forced into hyper drive. The Governor initially proposed a 16 bed replacement hospital while opponents argued for a full replacement or even a new larger hospital. As the authors of the Asylum paper note, the push for smaller hospitals comes from several quarters: “Progressive reformers, consumers, civil libertarians, and fiscal conservatives all advocated for a similar goal – the closure of publicly funded psychiatric institutions.” Vermont has no shortage of progressive reformers and the lure of reducing state costs appeals to both sides of the aisle. Due to the way the Federal government funds state budgets, a smaller hospital would bring in substantially greater matching funds for community programs. The hope was that these moneys would enhance our community system of care thus allowing for a smaller state hospital. The legislature ultimately approved a new 25 bed hospital and plans were made to develop enhanced community services.
The ensuing process has been simultaneously exhilarating, exhausting, and,at times, demoralizing. It took a long time to get programs up and running and during this time we had more people than ever before stuck in emergency rooms waiting for hospital beds to become available. This has stretched the limits and patience of our emergency room staff. However, we have also created some wonderful new programs. I now work with a peer crisis team who have taught me more than I could ever have gleaned from a book or paper about the power of peers to help their fellows in crisis. Just their presence in our agency has done more to promote the concept of recovery than any talk or lecture.
But there have been some unexpected and somewhat ironic consequences.
Vermont has fairly strict laws governing the circumstances under which people can be forced to take psychiatric drugs. It is not uncommon for people to be in a hospital for months while their cases are litigated. In years past, those who sought to change the law found their efforts thwarted by advocates with opposing views. When we had a state hospital those individuals who refused drugs were treated there but now they were held in community hospitals. This brought the attention of a powerful force – the community hospital system -to the debate. For the first time in over a decade, changes in the law were made to speed up the process in which people held in hospitals could be forced onto psychoactive drugs. So an effort to increase personal autonomy by reducing access to state hospital beds, has also led to a more rapid legal process for giving a person drugs against his will.
During this same period of time, I have increased my own resolve to try to limit exposure to neuroleptic drugs. Whether you think it is a recurrence of some underlying condition or a withdrawal phenomenon, reducing the dose of neuroleptic may still land a person back in a hospital. When there are few hospital beds, there is more pressure to discharge people as quickly as possible. Avoiding or minimizing exposure to psychoactive drugs involves going slowly – waiting before starting them and increasing the dose gradually. Those principles – caution with drugs vs. rapid discharge – can both be viewed as promoting personal liberty and autonomy but they can also be at odds.
In addition, if a unit has a higher density of highly agitated patients – another consequence of reducing beds – doctors are not comfortable waiting or going slowly with drugs. It does not feel safe. In an attempt to reduce the risk of long term exposure to drugs, I am increasing the risk of hospitalization where a person may end up on a higher dose than when we started. In an attempt to reduce the number of people in our hospitals, we have created units where there is a high density of more volatile and agitated individuals.
But there are ironies that go in other directions. In the Asylum article, they suggest an increase use of “assisted treatment in the community” a euphemism for forcing people to take drugs in community settings. Although there seems to be increased Federal interest in this, there is less enthusiasm in Vermont where when someone does not follow an outpatient commitment order the only recourse is to put him in a hospital. When there are few hospital beds, there is little enthusiasm to pursue this.
I have learned that I do not have an answer. I do not think we fully understand what is happening in Vermont in the sense that many programs are new and this complex system is still adjusting.
I am sympathetic to the concerns and fears of my colleagues who work in the inpatient setting and are struggling with volatile wards. I understand the pressures they are under. And to be clear, I am also sympathetic to the concerns of people I know who are admitted to these units and are sometimes frightened by the behavior of the other patients. The incidence of assaults on these units is rising and while I do not think my colleagues discount my talk about being more humanistic in our work, I wonder if they think that I and others do not fully appreciate their predicament. If I am not successful in keeping 100% of the people I see out of hospitals, if I turn to hospital level care when I think someone is not able to be helped safely in the community, it seems hypocritical of me to blame them for the actions they take to keep themselves and others on their units safe.
It increases my resolve to keep people out of hospital and in that way, I seem to be aligned with everyone on all sides of this debate. But then I circle back to the dilemma about reducing the dose of drugs and increasing the risk of the person being hospitalized once again.
There are some who lay the blame back onto psychiatry. If we had done this right in the beginning perhaps people would not be on drugs. Soteria Vermont was one of the programs funded post Irene and many of us wish it well. But as I read the literature, even those approaches do not work for everyone. And, at least from my vantage point, it seems there will still be individuals who decline every option or are too agitated to be in a community setting.
I communicate with many people who take all sorts of positions on this. For better or worse, I seem to be sympathetic to views that are not in alignment with each other. Lately, I find myself coming to the notion of both/and. Maybe I am misunderstanding or misappropriating that concept to this discussion but it seems we need to hold on as much as possible to a humanistic person-centered approach to helping people in extreme distress. At the same time, we can acknowledge that we will sometimes fail. Maybe some of you would not fail but we are a system of people like me and I know I fail. But then I try again. I am thinking of some people who I have worked with for years. Over and over again, I have tried to work in a way that is as close as possible to that person’s wishes and perspectives. For some, this was always easy and for others we have gradually worked it out. We have found a way to work together collaboratively. But in other cases, I have not been able to figure this out.
This started out as a discussion of asylum. Sometimes, I also wish there was a safe place for people to stay while they work through their crisis. We tried to build that into our system in Vermont and those programs are outstanding. But from where I sit, there continue to be people who can not live safely in our communities. Some do not seem to have the wherewithal to care for themselves adequately and others appear to pose a risk to their neighbors. In some cases, they refuse what we have to offer and for others, we do not have adequate resources. The issue of resources is not trivial. For state budgets, these services are a huge part of their expenditures and we can not do it all. Choices need to be made. The public loses interests in our issues and it can appear to them that our needs are unending.
For me, this remains an ongoing, difficult, and unresolved quandary.












Dr. Steingard, thank you for an intersting and thoughtful article.
In your articles, you repeatedly bring to discussion the topic of people whose behaviour is “anti-social”, yet they refuse ANY known model of treatment.
I want to ask you one important thing, however. So, my question is: does such description fit devoted rebels, dissidents, non-conformists etc.? These are people who are usually described (and treated) as “asocial” and/or “antisocial” not only by authorities, but also by the “silent majority” compliant to authoritarian dominance. Should their protest and resistance be labeled as “delusional” (which, by the way, happens quite often)?
As I have said here already, I’m neither “antipsychiatrist” nor even “anti-drug”. I’m, first and foremost, “anti-coercion”.
Well, in today’s quite coercive society, we can, at the very least, make coercion flexible. I mean that people accused of deeds which are considered “criminal” should be given a choice between trial and treatment. It will let them to decide whether they consider themselves right and want to persist in their conflict with the current societal order, or they evaluate their mental state as problematic and distressful, regret the behavior which they manifest because of this undesirable state, and want a professional help. In such a case, they should be presented with a full spectrum of possible theraupetic options – biomedical, psychosocial, spiritual – with full information of their pros and cons, and make an informed choice. And they should have the right to stop the treatment if they find it unsuitable for them, and face a judicial trial.
Such choice would be better both for principal contrarians who are adamant in thier uprising against the state of affairs which they percieve as unjust, and for genuinely disturbed people who have a conflict with society because of their undesirable psyche which they want to change – but do not have enough inner power to do it, and need a help of more knowledable and experienced person.
Report comment
Thanks for the comment. Although I acknowledge there is no fine line, I am talking about people who are not engaging in discourse which I can follow. I am always wanting to give examples but then constrained by confidentiality. Even in the court system, where they see many people are not not following the rules, they call us in because these individuals stand out as different in a sometimes profound way.
But fundamentally, I think this is what I am getting at with the “both/and”. We should never stop trying to engage in as collaborative and respectful way as possible.
Report comment
Sandra,
I continue to be puzzled by why you post on this site. I’m sure you are aware that almost all the users are against enforced psychiatry, yet you are always in favor of it. You mention “a safe place to work through a crisis” as if you are unaware that psychiatric hospitals are not safe at all. They immediately harm a person’s sense of self (leading to “tainted identity” that almost never can be erased), they put any person in danger of a thousand forms of physical harm, iatrogenesis, etc. and they never have enough facilities or personnel for actual psychotherapies that have been shown to help people in crisis.
As for your not being able to clearly explain what you mean by individuals not making sense to you, when you resort to the “confidentiality” excuse, it reminds me of the Catholic church refusing to explain things based on the doctrine of “mystery.” Maybe I’ve misunderstood you?
I’d love to hear what you have to say in response.
Report comment
I’m not entirely certain what you mean by users (readers? commenters?) but it almost sounds as though you’re suggesting that their agreement is a requirement for blogging here… that’s definitely not the case. I think I can speak for everyone on the staff of MIA when I say that we value Sandra’s perspective — a perspective that is much more thoughtful and nuanced, in my opinion, than “always in favor of enforced psychiatry” — and are grateful that she chooses to share it here. To really change things, we need to be aware of the dilemmas and unintended consequences that may result when people attempt to put principles into practice on the ground, in complex and less than ideal circumstances. And we need to understand how a person’s thinking can evolve over time as they grapple with these issues. I’m glad that Sandra is willing to be so open about her process here, because I think it can serve as a model to others in the field who will hopefully come to change how they practice psychiatry too.
Report comment
Thanks, Emmeline. It is a privilege to have this opportunity.
Report comment
Thanks, Emmeline, for replying for Sandra. I can see that Sandra would only be available to respond to compliments, not questions.
Report comment
Comment removed.
Report comment
Ann,
I was going to reply that I blog here because I was invited to do so. Emmeline seemed to address that before I saw your comment.
As for your other comments, I read them as comments that did not necessarily call for response. However, since you seem to want one I will try.
I do understand that people are harmed by being forced into hospitals and I try to do what I can to avoid that outcome. And while I do not agree with your characterization of me as being in favor of it, I admit that I can not always find other alternatives. I recognize that this is not an adequate explanation for some. I stand by my decision to not describe particular situations out of concern for privacy and I understand that you may find this a poor decision that gives the appearance of avoiding open and honest discourse.
Report comment
Sandra,
I do think it more appropriate for you to reply to me rather than having “followers” do so. I think that any paid professional who posts articles on this site should feel it incumbent upon them to engage in dialogue with commenters. Otherwise it is the same old power differential that keeps bad ideas in practice everywhere.
Did it ever occur to you that the very power differential inherent in you talking with a ‘patient’–i.e. that you have the power to incarcerate said patient–might have something to do with communication difficulty and breakdown?
If I were in your position, I would quit the whole system and set up something closer to what my conscience tells me is right. I say that having forfeited a large pension when I had many years in my profession and could write my own ticket. I simply couldn’t stand to be part of a conveyer belt that took to many people straight to hell. But I’m broke, Sandra, so you can see it is not the choice for everyone. Good luck with your own choices and I hope you feel more peaceful as you make them. At least you’re struggling, which puts you ahead of most.
Report comment
Sandra,
“And while I do not agree with your characterization of me as being in favor of it, I admit that I can not always find other alternatives.”
Perhaps, the alternative is not to stigmatize people with fictitious “disorders” and drug people with toxic drugs that cause the “mental illness” symptoms in the first place?
Perhaps, helping people is about actually listening to their real life concerns, and psychiatrists going to the police with crimes that have been committed against people, rather than just stigmatizing people with fictitious “mental illnesses” and tranquilizing them with toxic drugs?
Report comment
The one thing that I appreciate about Dr. Steingard is that she doesn’t pretend that there are any simple answers to the problems that people labeled as “mentally ill” face and deal with on a regular basis. I appreciate the fact that she admits that she doesn’t have all the answers, unlike so many of the psychiatrists that I deal with on a daily basis in the state hospital where I work.
I believe that it takes a certain amount of courage and guts to stand up and point out that there are no simple answers. All too often, I find myself reaching for the simple answers and solutions to problems that are not cut and dried, black and white, and they are certainly not simple at all. I also believe that at times, many in our movement only want the simple answers.
I appreciate Sandra’s willingness to show that she struggles with all of this, as any clear thinking individual would struggle with the issues.
Report comment
Ann, “I’m budding in” as I was just so enjoying the more positive exchange happening here that so often we don’t see when “professionals” blog. As a consequence most doctors won’t blog here as the negative comments feel like bashing rather than dialogue. I don’t think things will change if we can’t have an open and respectful forum to dialogue and for others who may be curious and or wanting to learn and join the discussion can’t do so without attach. I’m not saying your comments in this chain or attacking but they are a little bit. That said I want to say I wish there were more doctors like Sandra working in the mainstream as that in and of itself would start to change “business as usual” we need the “good guys” working in the belly of the beast!
Report comment
Psychiatric hospitals are worse than any hellhole save maybe Guantanamo prison and other places of torture. It’s beyond ridiculous someone can call them “safe”.
I’m a psychiatric surviviour and was tortured in such an institution and I know for a fact that is standard practice. I despise any attempt to defend torture, no matter if it’s called “enhanced interrogation” or “psychiatric treatment”. There is in fact a direct link between the two, obvious for anyone with a bit of knowledge about the history and sadly present.
Report comment
Isn’t it odd that “enhanced interrogation” of prisoners and supposedly benign and benevolent “psychiatric treatment” are the same thing? How can that be?
Report comment
Comment removed.
Report comment
“I mean that people accused of deeds which are considered “criminal” should be given a choice between trial and treatment.”
Accused? How about they get a trial and at sentencing they get the choice? Maybe we should stop with the Minority report already. You’re only a criminal in the eyes of law when you’ve been adjudicated as such.
Report comment
Thanks! If this was easy to figure out, it would have been done a long time ago. Sharing perspectives from different sides of the debate is important and valid. My feeling is that community-based programs have never been funded sufficiently to be as effective as they could be, and that models like Soteria are given up on far too soon. They’re never treated as more than pilot programs — and expected to produce instant results by people with vested interests, like psychiatrist, who can’t show instant results either — if they can show any results at all — and who feel threatened that someone else would set up a model of support that isn’t under their own control. If someone had a physical illness, like cancer, everyone would expect that it might take years to ever solve it and for that person to recover. But with mental difficulties, there’s no realistic picture in people’s heads. Some people work through their troubles quickly, while others need time, and maybe a lot of time — but we’re so fixated as a society on a quick fix that we expect instant results. It can be scary to deal with people who seem out of control, and if drugging them and locking them up relieves the public’s anxiety, the public will go for that option, and community-based programs will never get a chance to show their long-term outcomes. And I’m quite confident that the psychiatric establishment, given a chance, will pay no more than lip service to community solutions while actually undermining them at every step, whether by strangling their funding (every dime lost to community support is a dime not collected for appointments or medication) or by coopting them and turning them into yet another channel for coercion — turning them into the deceptively named “assisted” outpatient treatment programs. An object lesson is the history of state asylums. The original success of asylums was a result of the respectful and humane environment of the moral treatment model brought from Europe, where everyone was respected and no one’s freedom curtailed, and people had time to recover. It was so successful that state hospitals were built all over the country. But what happened next was that they were gradually corrupted by outside forces. Doctors — the self-appointed experts — took over and began to impose their treatments: cold baths, spinning, wrapping, insulin shock, electroshock, lobotomies, disabling drugs — and they brought with them the whole hierarchical structure of coercion and control, of the “expert” who supposedly knows more about the “patient” that she does herself, thus justifying their control. At the same time, the hospitals became a dumping ground for society’s undesirables. While those who recovered were able to return to the community, only those who didn’t were left behind, and they accumulated in number. Other undesirables — hopeless drunks, and teen rebels, and the socially disobedient, and blacks who spoke out for their civil rights, and communists, and unmarried pregnant women — were confined there, and kept there, because they were committed by other people who had been granted that coercive power. (The way the Soviet Union used mental hospitals and diagnosis and drugs should be a lesson to us all.) The whole purpose and structure of the asylums was subverted. If asylums were to return in something that resembled their original form, where it was about respect and freedom and being part of real community, I’d be all in favor. That would be a haven, not a prison. But if asylums return in the form they had in the past few decades, I have little hope that they will help anyone recover. Are the old asylums any better than the de facto system of “mental health care” that now dominates the country in the form of the prisons and jails? I don’t think so. Thanks for speaking up about the complex issues involved and your concerns.
Report comment
Hi Eric,
You make some very good points including the notion that it is easy to romanticize the notion of asylum. My one quibble is that I do not think it is the psychiatric establishment per se who strangles funding for community services. Some of us are part of that system. I think the psychiatric establishment sometimes undermines the credibility of alternatives and that is important to acknowledge.
Report comment
Here is some reason alternatives are under mined. One is, mentally ill people are not seen as people in need of help or support, but society wants to do them in and get rid of them for not living up to standards. Therefore they don’t get medical treatment, they can controlled, drugged, and imprisoned which is also very profitable to the unions who lobby for this type of stuff and the police state and private companies involved. Next up is, pills happen to be patentable, and profit can be had by each person drugged, tax dollars and insurance money can be siphoned off from society into the hands of rich wealthy investors, and everything in America is for profit. Anyway imagine being able to control what people think is treatment, get them to even exclusively prescribe pills, because its far more profitable and easy than letting the money go towards actually creating a solution or paying for psychotherapy, housing etc..
Report comment
Maybe we don’t need psychiatry at all? It seems like as far as “evidence” goes your drugs make people worse, your coercive interventions make people worse (personally they made my try to commit suicide which has it succeed would have for sure been blamed on my severe mental illness and not on the torture that people who subscribe to coercive psychiatry inflicted on me) – what’s the point?
You can’t tell who’s mentally ill, you can’t define mental illness based on any objective criteria, you serve as an institution of social control of undesirables and you punish the victims of abuse with physical assault, labelling and brain-washing.
Psychiatry is a useless entity – in contrast to other, somewhat legitimate areas of medicine, it can show no improvement whatsoever as the current “epidemic” shows. So why bother?
The answer is not in medicine, is in politics and social change. Psychiatry is a part of oppressive system that should be abolished.
Report comment
I agree with Eric’s concerns, as well as B’s comment that, “You can’t tell who’s mentally ill, you can’t define mental illness based on any objective criteria, you serve as an institution of social control of undesirables and you punish the victims of abuse with physical assault, labelling and brain-washing.”
I was defamed with a “mental illness,” unbeknownst to me at the time, based upon the lies of a genetically Russian ELCA pastor (a religion that originated in Germany), so that this pastor could cover up the sexual abuse of my child, and his denial of my daughter a baptism at the exact moment the second plane hit the second World Trade Center on 9.11.2001.
And perhaps also because I come from an ethical American banking family, and I am now disgusted to learn that our country’s banking industry has been taken over by the “banksters” that our founding fathers warned about, and our country is now being ruled by those who financed the Nazis.
I hope the psychiatric industry, that is currently willy nilly defaming everyone they can get their mother f-cking hands on to, with scientifically invalid “mental illnesses,” rethinks the wisdom of whom they are actually working for.
Report comment
Btw, I don’t mean this as a personal attack on you (although as a victim of coercive psychiatry I see you as a torturer every time you subject someone to this atrocity – there is just no “polite” way to put it even if you or some other people who may not have the experience see it as offensive). I appreciate that you are trying to make the camp a little more bearable for the inmates and prevent more inmates from being shipped in – there’s a value in that. But it also legitimises the existence of the camp and that I can’t agree with.
Report comment
Thank you Eric for your thoughtful comments.
D. Steingard, my point is similar – how long has Soteria house Vermont been operating? Think how many years it took for the people in Harrow;s studies to recover.
People in extreme distress need safe and humane places to go through their distress, possibly for years. They need it now, desperately. Families desperately need some safe place to take their loved ones when they need a break etc.
What is criminal is that people can be forced to take medications which could hinder their long term recovery. AOT results do not cite research that relate to `recovery’ (e.g. improved cognition, independence etc.) but to things like decreased incarceration, homelessness etc, that would be the result if a person was well, but also if they were sedated!
So please, let all of us who are worried about the long term effects of antipsychotics work together to focus on providing a system that includes forced safety for the severely ill -when necessary – that is independent of forcing drugs that could harm or hinder recovery. Once people are safe, then the discussion of whether or not medication is used can be a choice of therapy If a humane asylum as described by Eric is created and closely monitored , it could be an important part of that picture that stops forced medication.
Forced medication, given the state of the research, is the real urgent problem now.
Imagine if people were being forced to take street drugs which everyone acknowledges can seriously harm people – imagine how that would play out in the news.
Thanks, as allways for the time and concern you spend on these issues.
Report comment
I just wanted to add that having safe places to take people in extreme distress to, takes away any ‘justification’ of AOT (e.g. with proper supervision and care, noone could say these people were a danger to themselves or others)
I just wanted to add that a proper ‘asylum’ could create the environment needed for recovery. Now, people who believe medications hinder the recovery of their loved one try to provide a ‘healing home’ in admist a very prejudiced and misinformed society.
A protective setting could be set up so a person could work gradually to their independence – go by themselves to exercise or swimming or possibly to little shops etc, , go to work or school settings with people other than their family; knowing that there were trained and humane people who could step in when their stress became overwhelming. Maybe a percentage of people would make this their permanent home (research indicates around 10 to 15 %???), and the other 85% could eventually increase their independence to return to the community. Maybe some clients would be ‘day visitors’ living at home with their families, or parttime residents or working there as peer counsellors or in other jobs as they help the newly or more seriously afflicted.
Report comment
While I think you idea is a fine one, I nevertheless know people who decline these options.
Report comment
Is that kind of an option available in Vermont?
There are no places where I live where people could go to when they are in extreme distress, without having to take anti-psychotic medication. And there are no services that go into the home that do not involve forced medication. So having this option could provide enormous support to families who fear what the science is saying about antipsychotic medication.
And at least for those who decline this option, if there had to be `force’ it would be a better option than AOT, prison or hospitalization with forced medication.
Report comment
If someone is not free to decline an option, it can no longer be accurately described as an option.
Report comment
Good point, Sharon.
Report comment
“I nevertheless know people who decline these options.”
So? Should that not be their right? If they are indeed criminal and prefer to face charges for their behaviour it should be up to them. If they’re not criminal you should leave them alone.
There is nothing worse for one’s mental health than loss of freedom, dignity and right to one’s mind and body. Which is all coercive psychiatry does. It is torture.
Report comment
B,
Your argument- to prosecute people if they are breaking the law- is what is happening, according to those who believe in the concept of transinstitutionalization. This blog was a response to an article decrying the fact that rather than put people in hospitals we are puttin them in jails. We have many fewer psychiatric beds in the US now than we did a few decades ago. I think that is an unassailable fact. But on all sides, no one is happy about our mental health system. The authors of the commentary suggest building more hospitals. While I do not think you are suggesting we build more jails, I am not sure what it is you do favor.
Report comment
@ Sandra:
“While I do not think you are suggesting we build more jails”
I don’t because it’s a false choice: there are many things which are legally criminal which should not be and people should not be getting locked up for them in any institution. Many people in US are locked up on bs offences, often involving drugs (which use very often already put people in the “mental” category). Let these people out and we have half of the problem solved.
Secondly, the narrative itself is false: many of the people who get “diagnosed” in jail are getting diagnosed because they are in jail. Or they would never be in jail if they didn’t have a diagnosis because people who are labelled are treated worse by the justice system (“the dangerous mentally ill” – the stereotype which people advocating for coercive psychiatry propagate).
Thirdly, I don’t think that prisons are worse than psychiatric hospitals – in fact they may be better. Of course US prisons are not particularly known for their “humanness” but I know a situation in Austria where I’d take prison over psych ward 100% of the time – nobody would be drugging me to my gills against my will and I’d know what is the latest date I’m out – people who get locked in psychiatric hospitals even for small offenses end up doing more time than if they went through the normal justice systemand when they get out is usually based on “the psychiatrists said so” (there was recently a study which was reported in the press which addressed that).
Therapy in psychiatric hospitals is a sick joke, especially if you are not interested in being there in the first place. It always equals drugs.
Report comment
Sa: You wrote: :Now, people who believe medications hinder the recovery of their loved one try to provide a ‘healing home’ in admist a very prejudiced and misinformed society. ”
So we build asylums to compensate for a very prejudiced and misinformed society? After we pour billions of dollars into building asylyms, prey tell, when do we direct resources into the problem of reeducating people and changing our culture so that is is inclusive and tolerant?
You are also wrote: “Maybe some clients would be ‘day visitors’ living at home with their families” Hah! From experience, having a loved one forcibly committed to state hospital 200-500 miles from where a loved one was born or raised makes your idealist vision ridiculous.
Report comment
Yeah. The description of a “perfect asylum” fits the flowery description of some psychiatric hospitals. Sounds good on paper until you go there and see for yourself. Institutions, especially those where some people have power over others, ALWAYS -re-create the Stanford prison experiment. That’s human nature and good intentions pave the road to hell.
Report comment
OK, so– Yes, psychiatry did it. The mainstream won’t act against its immediate judgment of its own best interests. Very specifically I mean that however collegiate the various groups have to be, who get their credentials to have this perceived and real authority, in order to leave no question of substance about where there loyalties lie, that is the prime objective and it shows.
But all these terribly intricate problems are not part of my material purposes for earning my living. Positive strategies at this point seem like the joke they are guaranteed to be faced with the enormity of the problem. But if everyone got due process and could only be held against their will according to it, and that means in jails not psychiatric facilities, we’d have half the problem to deal with. The propaganda and stupidity of the hailing of revolutions in psychiatry as a way to get the public on board, that and the sum total of inconsitent messages we are told “help fight stigma” but really don’t–that also would be halved if the coercion was both made explicit as the guiding purpose of evaluations in the first place, and then limited by separating the proven offenders from the difficult companions on purpose. These are ethicists you say?
Report comment
travailler-vous :
I’m not following your logic. Could you try to explain this a second time? My intuition is following you and is saying a big “YES” but my logic is not concurring.
Report comment
Madmom – That’s the right way to put that, that my logic is something else to follow. Sorry, as mainly it is not reflective of good communication, but is shorthand for how I would think it over in the ideal thinking state: but I can explain, except I want to read the thread and go back to to reread Jill Littrel’s last post which is in many ways related. There, too, I was typing out what I myself thought helped me to keep the ideas together, alluding to the difficulty and posting a link to British female philospher who I rely on for constructive critique of psychiatry. The asylum vs. jail debate is farther from my own material purposes in life than the hospital, which I consider most unfortunately unusable for my own good, but which is where my lived experience comes from for whatever I can do to understand the views under discussion. Both Dr. Steingard and Dr. Littrell constantly make extensive revisions of their version of needed reforms and are each sharp in their own way and I don’t want to add an explanation of the logic of this flurry of doubts and concerns of mine without making sure I get my ideas clear. Especially since your interest is expressed on behalf of your daughter and since the moderator has to interpret the verbiage with the same problem in doing so as I left you.
Thanks for asking, and I’ll get to it. For starters, I presume that we are talking about reforms for the “failed paradigm” of behavioral healthcare, though, if that helps in the immediate moment. Also, I wanted to recommend a fine book to you that I just started and that I believe you would not want to wait on yourself, called “Imagining Robert” by Jay Neugeboren. He’s not at all square and lives as a writer; the story regards his fraternal relationship to his brother as he has gone through treatment for schizophrenic overwhelm. Neugeboren brings all the right questions to the table even when he’s too kind and encouraged by NAMI and MHA and those organizations or when he’s not putting quotation marks around Mental Illness and so on.
Report comment
Madmom – So let’s see about this trip back in time to re-explain. I’ve gotten enough distance from the initial motives to see what I h-o-p-e-d to have said. Whenever something gives me greater chance to hang onto stability, which does tend to be what follows intense flashback episodes, I end up surpised at how little my mind has changed about how bad the services on offer are. But my sense of humor comes back in better condition and my head’s more clear. So…
My point derives from the libertarian critique of mainstream efforts in both academic and clinical behavioral science, of everything from publication to court testimony. The system is just one grand crying out for permanent entitlement first and foremost, and patients are second in line at best. Really, it is not hard to see that the push of the allied mental health industries is wholly toward the formulation of a medico-therapeutic bureacracy that blurs all distinction between private enterprise and government “aid programs”. Wow, that shows prominently in the work I’ve seen underway in mental health wards and community mental health centers and doctor offices, come to think of it.
The other idea is that the same people who gave us this failed paradigm are very nearly the ones who will give us the next version. The ethicists today are representatives of their employers and tomorrow they still will be. (And I think that “failed paradigm” has got to suggest “flawed from the outset” and “rotten to the core”, etc.)
I find myself able to interpret my first post line by line, but it’s not of enough interest in comparison to just expressing myself anew, since now it is easier. Meanwhile, thanks for asking in the first place. It says something nice about your attitude that you’d care to make out the meanings in connection to the intentions for my trying to communicate them!
Report comment
Travailler-vous: Thank you for revisiting this post. I like how you express your ideas and I appreciate the recommendation of the book (which I was reminded of when I re-read your original post to put your second post in context) Are you bi-lingual by any chance? It would be nice to keep in touch. You can email me at [email protected]
Report comment
madmom- I got you on that, so if you want to have Emmeline pull down your email address you can probably get her to. I am–maybe unmistakably– American, and although I could have been brought up with biracial consciousness, it escaped emphasis likely as not because the language had been let go down through the generations. Typically, I know only the language that I have to know.
Report comment
“These are ethicists you say?”
I love the people who are making up great humanistic theories from the midst of their ivory towers. Completely ignoring the totality of human history with the special emphasis on the XXth century. Yeah, I’m sure the new day asylums will be nothing like the old day ones. I mean the nature of humanity has evolved so much during the last… well that would be 10seconds because even the current scandals in psychiatry and beyond show we are not past the Milgram and Stanford prison experiments and worse.
Report comment
Thanks for the piece Sandra. I agree that there should be a” safe place for people to stay while they work through their crisis.” The complexity arises when we talk about the varieties of crisis.
Here in Portland, the various hospitals have found themselves increasingly squeezed and are losing large amounts of money in their acute settings. This is largely due to the fact that acute hospitalization tends to involve people who have limited or state insurance. This leads to poor reimbursement while funding the payroll for all the doctors and nurses is exorbitant.
For this reason, the largest hospitals are pooling their moneys to centralize and create one large inpatient facility in Portland with its own psychiatric ER. This is mainly a cost savings measure but points to the inherent problem with crisis mental health care. Generally, the medical system is far too expensive to “manage” crisis. Its just not a model that has made fiscal sense.
We are in desperate need of alternatives that are not only cheaper, but far more humane. One of the main problems I see is that most anyone in crisis is funneled into one monolithic system. Those who are high, drunk and acting bizarre and agitated, someone with dementia who is violent, someone who has stopped taking strong neuroleptics, people experiencing “first-break” episodes- all get funneled into this one system and tend to receive very similar care- psychiatric drugs and often a short stay of a few days before being sent out for services (generally lacking) in the community.
We need systems where we funnel a number of these folks to systems of care that do not prioritize med management. This is especially important for “first break” folks. In my perfect world there would be “asylums” designed to allow crisis to run its course without medical intervention. But my second best choice (and likely more realistic) is to promote a non-interventionist model for first-break in a hospital setting where people are not immediately started on strong doses of neuroleptics, or at least offered a choice for selective use.
In this way we may not create a group of folks who require long term med management. Once this happens, folks often cycle in and out of hospitals due to intermittent and understandable “non-compliance.” Then it becomes much harder to create non-medical alternatives for crisis. I believe we have to really start at the beginning when people first start taking strong meds and try to avoid that as much as possible. Once an individual has been taking psych drugs for a while, it is deeply challenging to offer alternatives that don’t in some way involve psychiatric intervention, even if it means to help taper someone safely as you have been talking about. And when someone is agitated and has been cycling on and off meds, soteria and respite models are not effective. We have to go the root and start from the beginning and address how this epidemic has happened. Trying to fix it midstream is deeply challenging.
Report comment
I just want to add although starting at the beginning would be ideal, people on their second break or third break or whatever, should also be given the opportunity to be in a safe place where the crisis can run its course without medical intervention.
The people in many stories of recovery started off on drugs, or had many relapses, or like Katherine Penney, went for years prior to recovery. Somehow -whether it is in an ‘asylum’, soteria house, healing home or hospital people must be allowed the chance to work through a crisis without medical intervention if it seems that this is their best chance for recovery.
Report comment
…..when I say medical intervention, i actually mean forced medication
Report comment
Right on! Great point, Sa!
Report comment
“[W]hen someone is agitated and has been cycling on and off meds, soteria and respite models are not effective. We have to go the root and start from the beginning and address how this epidemic has happened.” And realistically, it stated with defaming and drugging people with scientifically invalid “disorders” and mind altering and toxic drugs in the first place.
Report comment
Forgive the typo, “it started…”
We’re dealing with an iatrogenic problem, and an iatrogenic epidemic actually, propagated and supported by the unethical few currently in charge, and whom actually profit off these crimes. The psychiatric industry needs to wake up, your drugs cause the DSM disorder “symptoms.”
Report comment
Jonathan: You laid it out brilliantly. Creating choices and alternatives while keeping costs down. If people who are undergoing a crisis, aren’t ‘medicalized’ to begin with, perhaps we could avoid the enormous costs of funneling people through the medical system. The medical system is ballooning out of control in in general, not just in the mental health side. A culture shift needs to happen before we can stop viewing all people who are confused, disoriented, scared, angry, etc. as in need of ‘medical’ expertise/treatment. The only reason why parents like me take a child who is experiencing their first ‘break’ to the ER where they are introduced to neuroleptics, restraints, and where they are inflicted with unfathomable psychological harm, is because we are lacking in imagination due to the homogenous way we have been raised. Plus, we are products of a generation that was raised to believe that doctors were trusted and wise authority figures, like Marcus Welby. We had no idea the level of mediocrity that psychiatry had become due to commercial forces, lack of imagination, and scientific curiosity.
Report comment
“parents like me take a child who is experiencing their first ‘break’ to the ER where they are introduced to neuroleptics, restraints, and where they are inflicted with unfathomable psychological harm”
And then psychiatrists complain that there are people who don’t want any options. Is it so difficult to understand that some victims actually have the strength and dignity of resisting oppression. And once victimised they have no interest in becoming pets of “good-meaning” psychiatrists.
I just don’t understand how can you not understand that and see it as unreasonable or even “lack of insight”. the only person lacking insight is the psychiatrist, who apparently lacks empathic skills to understand this.
Report comment
Apparently imagination which includes empathy and a sense of humor are severe psychoses. Psychiatrists are certainly devoid of them. Once they get through messing with your brain you will be too!
Report comment
Thanks for your comments. I have been thinking lately that the way to stop current psychiatric practices — the drugs that debilitate and eventually kill people, which consumes simply enormous public resources, and the extremely expensive recurrent hospital stays and endless psychiatric bills — might be the way to attack the system and put something else in its place. For instance, just to use my own case as an example: A hospital stay, even a brief one, costs many thousands of dollars. When I became psychotic, I cost the system more than $10,000 in just a few days. After I became psychotic, I was given disability — at a cost of more than $1,000 a month. Since I was prevented by the drugs from ever truly recovering, and in fact further disabled by medication even after the real psychosis passed, that meant it became a permanent expense to the public. (In the interests of total disclosure, I’ve only just completely eliminated meds and haven’t yet rebuilt my life enough to get off it, even though I’m getting there.) Psych meds also come at a premium: more than $700 a month for the single drug I was on, and I was one of the lucky ones who resisted being sucked into the system of polypharmacy, where you might be juggling numerous expensive meds. Because that antipsychotic stopped my metabolism, it caused immense weight gain and high cholesterol and high blood pressure and high cholesterol — and now we’re talking more bills to medicare, not only for drugs (insulin alone is $350 for a supply that might last as little as a month, but that really does vary, so it’s only a ballpark number . . . but then there’s the other stuff, which added up to at least a $100 a month.) Now add doctor’s bills — for follow ups and dealing with new problems as they emerge. Even now, I am dealing with the fallout of what happened to my body, and though I have eliminated the big-ticket items like antipsychotics and insulin, the expenses haven’t ended. And there’s another cost: while disabled, social security paid my child support to the tune of $500 a month. So: instead of my returning to being productive as soon as I might be able, for many years I have been an enormous drain on the system — to the tune of roughly $30,000 a year. And since I haven’t had to be rehospitalized or had multiple psych drugs, I suspect that I’m one of the cheap ones.
Perhaps what we need to do is reframe the entire public debate away from the personal costs of current psychiatry, because there seems to be a kind of blind spot about mental difficulties in our country. The public debate is framed mostly by fear of what those with mental difficulties are going to do, and it is from this fear, unthinkingly played on by the media, that psychiatry derives its power. Desperate people will turn to the people who present themselves as having the answers, and in our society, that’s psychiatry. The human picture of what actually happens to most people who come under the influence of that system is completely obscured. Psychiatry’s harms are swept under the rug, maybe because there is this constant triumphal march about their supposed progress, how they’re supposedly helping, while their actual record is almost never examined. That ten years on antipsychotic shortens your life expectancy by five years, for example. And maybe the way to attack the system is to reframe the discussion outside their rhetoric of illusory scientific progress and cast it in terms of actual economic costs. If we can contrast the public cost of community-based models like Soteria, or even the costs of a program like Open Dialogue in Finland, we might discover that all of a sudden people will stop being distracted by psychiatry’s rhetoric and become more openminded to examining actual outcomes. Talking money might wake people up to shift the model away from the current system and get us the funding we need to set up something that works — based on humane conditions, mutual respect, no forced medication, and community support — long enough for us to prove on a large scale that it works.
Report comment
Eric,
This is such a great post. I hope through this whole discussion a movement to provide funding for alternative services on a larger scale will be born.
Dr. Steingard,
Thank you so much for opening this discussion. I think the fact that you continue to work as a critical and caring psychiatrist within the system, without always having the adequate supports available to preserve safety, is truly brave and honorable.
I think as a family member living somewhere where there is inadequate support for my loved one, I can truly understand the dilema where one might have to choose the hospital Hopefully recovery for our family will continue in the positive direction it is going so we will never again have to face that decision.
Report comment
Eric:
I completely agree with everything you said. My daughter’s ‘treatment’ has cost the taxpayers and our private insurance company close to 1 million dollars, in five years, not including her monthly disability checks of $1,200. For a fraction of this cost, she could have been directed to a program delaying her exposure to harmful neuroleptics during her first break, and received peer support, food stamps, a bus pass, supported housing, and college tuition. I am certain she would not have come off the hinges this way or have a criminal record but would now be a productive member of society. Instead, her confidence is crushed and the psychological harm of being recommitted and forcibly medicated again and again and again is beyond description
Report comment
“In the interests of total disclosure, I’ve only just completely eliminated meds”
Congratulations. Such good news. I hope everything goes well and you’ll be able to recover permanently :).
Report comment
Great comments from all here and I just want to continue on with what madmom says. Imagine a campaign where the expenses for “helping” someone is tallied up. Put a monetary figure on each person in terms of hospitalizations, psych drugs, health complication medicine and surgeries, disability checks, etc…
Call these folks the million dollar man or million dollar woman. Then describe how that money could be spent…as you just did Madmom. Then simply ask…is this how you want your taxpayer money spent?
Report comment
I agree, Eric, our society’s current “mainstream” unethical manner of “social control,” which results in covering up the crimes of the unethical currently in charge, is absurdly expensive and unjust.
As a society, we need to learn of the lack of scientific invalidity of today’s psychiatric “illnesses,” and that today’s fictitious “diseases” are no more credible than were the fictitious “diseases” of the Nazi’s. And this includes the 1% and those connected to them like the religions. Treating all others as one would personally like to be treated, is of paramount importance, instead.
Report comment
Eric,
I agree that approaching this from an economic perspective will have some traction. As I noted above many disparate groups come together when there is a potential for cost savings. We need good data to support that. But we also need to show that short term intensive costs (let’s say in the form of intensive support for those experiencing psychosis) might yield longer term savings(as you note above in reducing the chance of a person being on disability).
Good luck with your ongoing recovery!
Report comment
Warning: Reading the following article will probably make your blood boil.
Drug companies and Schizophrenia: Unbridled Capitalism meets Madness
Loren R. Mosher, Richard Gosden and Sharon Beder
http://herinst.org/sbeder/corppower/drugcompanies.html#.VMV3bId0yfA
Report comment
Thanks Donna,
Fabulous perspective of what was going on in the psycho / pharmaceutical industries at the turn of the most recent century, I appreciate the link.
I was surprised by the Whitaker quotes:
“Zyprexa” … “It’s a potential breakthrough of tremendous magnitude.”(Whitaker, 2001, p.260-61)”
“Or as the Los Angeles Times (1/30/98) put it: ‘It used to be that schizophrenics were given no hope of improving. But now, thanks to new drugs and commitment, they’re moving back into society like never before.’”(Whitaker, 2001, p. 259).”
But I suppose they prove why Whitaker’s current, thankfully, like Sandra’s, “are a perspective that is much more thoughtful and nuanced … than ‘always in favor of enforced psychiatry.’” And their current perspectives are of concern to the mainstream psychiatric industry. Since they are much more well researched, critical, and open minded, than that of the perspectives of most mainstream psychiatric practitioners.
As a person who was flipantly defamed as a “paranoid schizophrenic,” “depressed by self,” and “bipolar” (all within three weeks, and unbeknownst to me at the time based upon gossip from others and with no personal or family history of any mental health issues) by a PCP and psychologist, who, I later learned from their and others’ medical records, wanted to cover up the PCP’s husband’s role in a “bad fix” on a broken bone of mine, and the medical evidence of the alleged sexual abuse (with medical evidence) of my child for the psychologist’s pastor and/or his friends.
I will definitely say we need the critical voices of the psychiatric industries’ unchecked power within our society. And we need to rethink our respect of all those professions that, when I was a child, were formerly respectable. My personal experience implies we’ve ended up with the psychopaths in the formerly respectable professions. And a decent pastor did confess to me that I’d dealt with “the dirty little secret of the two original educated professions.” Which I guess implies that the religions and medical community were never actually respectable?
I personally think we need to rethink the wisdom of our forefathers, and the importance of returning to a society of “checks and balances.” I know the “antipsychotics” can cause “psychosis,” in a healthy person who is inappropriately put on them. Perhaps force medicating anyone with them should not be the legal right of any doctor for any (especially unethical) reason, particularly since every person reacts differently to these drugs, and they’ve now been proven to be toxic in the long run for all people?
Report comment
Soneone Else,
Thanks for your encouraging comment about my link to the great Dr. Loren Mosher and colleagues with an excerpt from a highly acclaimed book on “schizophrenia.”
This rather short excerpt does a superb job explaining the out and out evil corruption by Big Pharma of all those in power from government, medicine/psychiatry, academia, the supposed watchdogs like the FDA, NAMI and other drug company front groups, the media for the most part, advertising and promotion, schools, the courts, familes and society at large.
I hadn’t realized that Big Pharma was actually literally behind the forced treatment agenda to further expand their lethal neuroleptic drug markets while preying on children, the elderly, pregnant women and babies in utero and any other breathing (if only barely) human being who could be forced on these poisons for their insatiable greed, power hunger and sadism. Of course, this makes sense when one considers that Dr. Robert Hare, world authority on psychopaths and consultant to the FBI, agreed with the author of the book and DVD, The Corporation, describing its evil agendas and “behaviors,” that many modern day “corporations” as well as those leading them could well be described as psychopathic (or just plain evil, intraspecies predators).
Of course, Jim Gottstein, J.D. gives some involved the benefit of the doubt when he uses the terms duped or complicit describing this debacle, meaning that not all involved were aware of the predatory Big Pharma/biopsychiatry KOL/APA agenda behind the new “magic bullet” supposed wonder drugs or second generation neuroleptics with the best corporate spin money could buy. Even Bob Whitaker said he believed this great miracle story until David Oaks, former Director of Mindfreedom, encouraged Bob to investigate the history behind psychiatry’s great DSM and neuroleptic wonder drug “success” and the rest was history as Bob explains on a blog about Oaks being a great influence on him. And this excerpt doesn’t even touch on the next monstrous invention and expansion of the bipolar fad fraud described in Dr. David Healy’s MANIA: A Short History of Bipolar Disorder, that demonstrates that the DSM III and IV addition and expansion of this latest garbage can “sacred symbol” of psychiatry could be used to prey on one and all including perpetrators and victims, Axis II and anyone but the “kitchen sink” to push the lethal neuroleptics and the bogus “mood stabilizers” or reinvented epileptic drugs for a bogus theory that bipolar and epileptic seizures have similar paths. This also coincided with the nefarious Texas Medical Algorithm scandals to push the toxic second generation neuroleptic drugs on Medicaid programs nationally that has led to a vast number of children in the state welfare and orphaned children programs being on these poisons. Fortunately, in recent years there has been a public and media outcry about this toxic over drugging of such vulnerable children thanks to Senator Grassley exposing the child bipolar overreach to justify toxic neuroleptics for children by Joseph Biederman actually working on behalf of Johnson & Johnson. Biederman was supposedly doing an NIMH government study while promising J&J positive study results of their neuroleptic drug before the study was even done, which is illegal especially with an NIMH grant, getting him the usual slap on the wrist despite being responsible for the death of toddler Rebecca Riley and similar victims thanks to his bipolar toxic drug cocktail protocols that single handedly caused the child bipolar epidemic. MIA recently posted an article about how this child bipolar epidemic came about mainly in the U.S.
I guess I was pretty naïve not to realize Big Pharma’s role in the forced treatment agenda, which makes the likes of Torrey, Jaffe, Murphy all the more dangerous.
You cited the quotes by Robert Whitaker as puzzling, but these are actually quotes by the perpetrators quoted by Whitaker in his great book, Mad in America, when Bob first came to realize these sordid truths about the great claims of progress with the treatment with neuroleptics or “magic bullets” of the so called mentally ill. Thus, those quotes are used by Bob to make his points about the bad treatment of those stigmatized as mentally ill and certainly not to condone it. It appears Bob had a pretty close relationship with Dr. Loren Mosher with videos of their talking together about the “mental health system” on the web including a great site called Yoism.
I’m glad and impressed that Dr. Sandy Steingard read Bob Whitaker’s book with an open mind and has gradually been changing her own views based on his work and her own related research and trials while being more upfront with her patients with informed consent while trying to wean people off toxic neuroleptics as much as possible. (I hope you hear me Sandy).
Report comment
Sandy,
My last paragraph expressing my gratitude and admiration for you(despite our differences past and present we’ve agreed could exist while having some meeting of minds) was buried in my post, so I’m recopying it in the hopes you will see it and hang in there. I’m glad to see you still posting at MIA and I appreciate your long term efforts to learn about and fight against the worst of the Big Pharma/biopsychiatry APA/KOL/government industrial complex as you continue to share this process with us.
I now have a famous Dr. Steingard quote I use when I don’t think things easily fall into black and white categories: “I’m feeling “muddled” about this…though that wasn’t your exact quote I’m sure, but the idea sure works when one is honestly “muddled” when trying to make sense of the best choices in very complex, difficult situations that you obviously face daily with limited funds, resources and support.
Here’s my last paragraph in my above post that is a tribute to you though you might not think so reading the rest of my post:
“I’m glad and impressed that Dr. Sandy Steingard read Bob Whitaker’s book with an open mind and has gradually been changing her own views based on his work and her own related research and trials while being more upfront with her patients with informed consent while trying to wean people off toxic neuroleptics as much as possible. (I hope you hear me Sandy).”
I also miss your posts on 1boringoldman and hope you won’t allow the bullies to drive you away as others there expressed as well.
Report comment
Donna,
I’m always blown away by your research, thank you so much for it, and all your references. It’s always so commensurate with my personal experience and research, as one wrongly defamed with today’s “bipolar fraud,” for unethical reasons.
“You cited the quotes by Robert Whitaker as puzzling, but these are actually quotes by the perpetrators quoted by Whitaker in his great book, Mad in America, when Bob first came to realize these sordid truths about the great claims of progress with the treatment with neuroleptics or “magic bullets” of the so called mentally ill. Thus, those quotes are used by Bob to make his points about the bad treatment of those stigmatized as mentally ill and certainly not to condone it. It appears Bob had a pretty close relationship with Dr. Loren Mosher with videos of their talking together about the “mental health system” on the web including a great site called Yoism.”
I ran into information on the web claiming these were Bob’s personal quotes, which struck me as odd, since I’d read both Mad In America and Anatomy of an Epidemic, and had not recalled these as quotes by him personally. Thanks for the clarification.
I too am grateful for the critical psychiatrists like Sandy. But I’m still amazed by the staggering brainwashing of the psychiatric industry, who don’t seem to understand that treating all others, as one would personally would like to be treated, is how all humans should treat all other humans.
And Sandy, I’ve met you in real life, I know your psychiatric training / brainwashing is still difficult for you to overcome. We have a long way to go in regards to retraining the psychiatric industry that the way to help others heal is to actually listen to their concerns and properly deal with their real life problems, rather than just defaming people with scientifically invalid disorders, and tranquilizing people.
Report comment
Donna;
I’m glad you brought up the point of how Robert Whitaker was influenced by David Oaks. One of David Oak’s gifts to this movement is his ability to talk to people and make friends on both sides of this important debate. Many of us who have a loved one who has been/is beinbg harmed by psychiatry experience great difficulty communicating calmly and rationally with people who advocate for coercive practices such as AOT. If psychiatric survivors like David Oaks, were not willing to share their experiences, calmly and with great dignity, to mainstream individuals who ‘had no idea’ what it feels like to be medically raped, things would be even worse than they are currently.
Report comment
Donna and madmom and others-
Thank you all for the interesting discussion. I realize I do not comment to everyone but at least people can know I am reading and when I think I have something of value to say, I say it. It was suggested above that I ignore the negative comments and while an analysis of my comment frequency may suggest this is true, from my perspective, I am respecting the right to voice dissent while avoiding what seem like irreconcilable differences (for instance, that at this point I do not know how to avoid forcing some people into hospitals).
It is interesting to me that David Oaks and I graduated in the same year from the same university. We did not know each other and we only met once at a rally at an APA meeting in 2012. From what I know of him and have learned since, I agree with what madmom has written. Of the many people from our graduating class who have gone on to have prominent careers in medicine – and many are psychiatrists – I think David Oak’s contribution’s are the most significant. I have enormous respect for him and I regret that our paths did not cross sooner.
Report comment
“for instance, that at this point I do not know how to avoid forcing some people into hospitals”
That is quite simple: don’t do it. You may not be able to prevent these people being tortured but others but you’re responsible for your own actions.
Report comment
Sandra, I want to thank you for sharing your insights and perspective on this troubling article in JAMA, the issue of promoting bringing back the “Asylums” for the supposed rising numbers of people in jails and prisons that have mental health labels. This is such a complex issue and so easy to jump to conclusions..As the blogger, “1 boring old man” brings to light that this so called conclusion may in fact not be based on accurate data. I also want to honor you for your openness in sharing your challenges and vulnerability in your personal struggle as you work to find and practice as best you can in a complex world with varying opinions. We need thoughtful doctors like you working in mainstream, ones who are open to new information, that can acknowledge maybe we’re doing things wrong and causing harm. Doctors who listen to what their patients say and are committed to really listening and working with rather than being “the expert”. Acknowledging that psychiatry is in fact not a science but could be an art form, might be the first step. I hope we all can be open to change and remain open to new information and evolve as we learn. What really strikes me is the almost knee jerk response by these members of U.Penn Medical Ethics to jump to this conclusion without an in-depth study of the prison data. (read 1 boring old man’s data that he sights!) And to think the solution is to return to the old State Hospital model (Asylums in this JAMA article) as if that was when things were better! Wow!
This lacks so much of what has been learned over the years post deinstitutionalization. Sadly community models were never funded, which was the supposed grand plan to be the next step when the State hospitals were closed. We certainly know that what helps is human connection, safe places where one can be allowed to go through difficult times without judgment, forced meds, but to have a place to sleep, food and people to talk with or not. A true Asylum in the words of R.D.Laing, not what these “ethicists” are calling Asylum. We know that being with others who have had similar experiences, models such as Peer Respite houses are reportedly benefiting those who have the option to access these homes, again, there are only a handful in the country due to lack of funding. While our federal government, representatives like Tom Insel director of the National Institute for Mental Health, has spoken out against the DSM and has acknowledged the medications don’t “cure” people, and in fact have been causing more harm, what has he directed new federal dollars to do? More Brain Disease research! Zero dollars are being allocated to community support services, true community support. The models are out there, Soteria, Open Dialogue, peer support, Hearing voices support groups, Emotional CPR, Housing First, .. So while we have many alternative models, they are all sorely lacking the necessary funding to be fully staffed and implemented nation wide. Small pockets of alternative models stand out with either private funding (so only the wealthy can access) or short lived pilot projects funded with grants that aren’t able to be sustained because there’s no federal or state money. I think we need to demand that our federal and state dollars be spent on what people who have survived the broken system are telling us… what they say worked for them and replicate more of that. I’m appreciative of having doctors like Sandra Steingard be willing to join with the alternative movement and take risks and speak up. I can imagine how difficult this is as one becomes marginalized by their peers and then often marginalized by the group they are agreeing with and joining. How can we be more welcoming?
.
As more and more doctors and providers of the mainstream system come out and speak up as Sandra is doing, we need to welcome and work together as allies rather than attack and critique. Where is the common ground? How can we build upon this and create a huge ground swell of both outrage at the “business as usual” and demand that funding is targeted to building natural communtiy support on all levels. This includes law enforcement, families as well as professionals, and peer supporters.
Report comment
Beautifully said! Dr. Steingard has already done so much to help give credibility to alternative approaches and we need to all work together for changes to community support. I wonder how this can best be organized?
Report comment
We have a national and international Foundation that was inspired by Whitaker s book, Anatomy of an Epidemic. A group of people with lived experience, researchers, doctors, providers, philanthropists all got together and started this Foundation almost 4 years ago. We have launched some important research (without big pharma $$) that has been published in JAMA, and have both educational funds like the new one with Mad in America (MIACE) on line CEU’s for all providers and family members…as well as Funds to support alternative models of treatment, Open Dialogue and residential models, the Hearing Voices Network, Intentional Peer Support….see our website and please please spread the word for more donors to work with us. Anything is possible. Given that the Federal Government is putting all their tax dollars into brain research, we can’t wait another 50 years for them to find or not find answers, we are trying to be a place where people can both design new funds for starting programs and/or donate to existing alternatives that we know work. Everyone should know about the Foundation and spread the word. http://www.mentalhealthexcellence.com. or contact me if you’d like to learn more. I’m the Senior Program Officer for the Foundation. [email protected]
Report comment
Thanks for making me aware of this. I will be sure to spread the word.
Report comment
The mentally ill are in prison in high numbers also because the USA is the worlds largest police state.
In October 2013, the incarceration rate of the United States of America was the highest in the world, at 716 per 100,000 of the national population. While the United States represents about 5 percent of the world’s population, it houses around 25 percent of the world’s prisoners.
The U.S. incarcerates 716 people for every 100,000 residents, more than any other country. In fact, our rate of incarceration is more than five times higher than most of the countries in the world. Although our level of crime is comparable to those of other stable, internally secure, industrialized nations, the United States has an incarceration rate far higher than any other country.
more http://www.prisonpolicy.org/global/
“The private contracting of prisoners for work fosters incentives to lock people up. Prisons depend on this income. Corporate stockholders who make money off prisoners’ work lobby for longer sentences, in order to expand their workforce.
The prison industry complex is one of the fastest-growing industries in the United States and its investors are on Wall Street.
http://www.globalresearch.ca/the-prison-industry-in-the-united-states-big-business-or-a-new-form-of-slavery/8289
Research on mental illness in prisons and jails needs to look at the fact that never before in human history has any nation locked up so many of its citizens the way the USA does.
Report comment
They are fighting over who gets to own the prisoners. You have to commit a crime first (with proof and a trial) before you lose your freedom.
ER Nurse bloger writes it is all a set up, they( medical psychiatry) take away a persons freedom then wait for them to get angry (during the long wait) so they can call them sick and drug them.http://emergency-room-nurse.blogspot.ca/2015/01/mental-health-patients-are-treated-like.html
Report comment
It does seem that since 9/11/2001, this country has actually been facing an internal war against the citizens of the US, by Wall Street and the corporations.
Report comment
Problem is, these hospitals are never used as intended and are mostly to lock these people up, deny them care, force drug and get away with assaults and battery. This is one of the reasons these places are shut down. There is not a safe institution.
Also if you even give them an inch by thinking it won’t be this way, they will go towards a model that always includes some type of destructive properties, trauma inflicted with drugs, shock therapy, seclusions, restrains, beatings of patients, deprivations, and isolation with no outside checks or legal protections. It will never be like a resort, never be drug free, free of forced drugging, free of voluntary druggings, leading all patients to serious illnesses and injuries. Also the staff who run these places tend to be unskilled lay persons without degrees or education, as the floor staff need nothing more than a training course to become simple nursing aids and this attracts lots of riff raft unions, state employee, correctional and for profit types who just want to make a secure working environment while using the place to make a buck. The patients/clients are always second best in a place like this, and when push come to shove on abuse, they’re framing each patient to look like the most intense schizophrenic to get away with the violence and abusive practices that ensue which also helps them legally justify such violence and abusive practices, meaning with a nod and a wink it’s state and police protected abuse and violence. When a client/patient cannot leave, this requires them to take extordinary measures after years of fuck ups and incidents that cannot get better in such a situation, including even killing of patients out of retaliation and super high doses of drugs to incapacitate and maim. I know, this is how the Oregon State Hospital is ran today and how it’s been ran for decades, and I trace it back to its earliest days including reports I uncovered from the entire 1900s days ..
http://www.obamasweapon.com
Report comment
Todd:
Having a family member residing for several con-consecutive years in the institution you refer to, I agree with most everything you say and I believe that staff members do retaliate against patients who are rebellious, most notoriously by ‘upping the meds’ and adding stigmatizing new labels such as ‘personality disorders’ to a patient’s long list of diagnoses. I believe that sometimes patients are set up for failure in both in-patient and out-patient settings providing an unconscious type of “I told you so” retaliation when doctors are not rewarded with gratitude and adulation from the their most rebellious and antagonistic patients. Doctors who run the gamut when they exhaust their single page prescribing algorithm without success often blame the patient and this too, can be expressed in a type of retaliation such as by cutting them from the caseload.
If you believe, as I do, that meds are used primarily as chemical restraints for the benefit of the caregivers and to foster the smooth operations of an overly large institution, then yes, definitely there is much to be bitter about.
If our mental health system was imbued with values of empowerment and self determination and if psychiatrists were willing to accept that empowering their patients is by far, a more effective prescription, than dopamine binding agents which flatten the emotions and kill desire, then patients who exhibit a healthy desire to run away should be rewarded and reinforced! Every time my daughter ran away from an institution the system’s answer was to rehospitalize her and inject her with higher and higher doses of neuroleptics. Although any normal parent teaches her child that it is completely appropriate to run away from abuse, when one encounters it in the hospital or a foster home, when one is civilly committed, running away is not only not an option, it is viewed as ‘proof’ of illness! I have never witnessed anything as insane, crushing to the human spirit, and as antithetical to healing.
As you know, the experience of torture and abuse does nothing to adequately prepare patients to live fully and independently in the community. I hold that patients who are restrained, isolated, and forcibly medicated are being tortured. Even the United Nations has gone on record saying this constitutes abuse. Once discharged from a facility that routinely engages in psychiatric abuse or is coercive, an individual will always be looking over his\her back and it will take years, if not decades to overcome the trauma of being locked up and restricted, while living in fear of abuse.
As you know from experience, conformity is critical to the smooth running of a secure psychiatric facility, particularly large state hospitals like OSH, which cannot or will not cater to individual needs, even if those needs are rooted in an individuals cultural, ethnic, or religious background. Patient centered care in a large institution is a joke. Once you are in the system, you are prodded through a pipeline like cattle moving down a chute. You have very few, if any choices.
The argument goes something like, if you bend the rules once, such as security rules or visiting policies to meet an individuals needs, soon there will be chaos. After all, if one individual seeks and receives special attention or accommodations, even if it fosters his/her mental and emotional growth, everyone would want the same accommodations. There is a cheaper by the dozen mentality in asylums, after all. And then there is this confounded fear of patients going AWOL and maybe what, do axe murders, while they are on the lam?
On occasion, a staff member will use discretion (often off the radar) and bend the rules to assuage the mental agony that most patients experience by being locked up and having no comforts of home or community; but most employees are not secure enough as individuals to exercise such discretion or they lack the training that would give them confidence they need to trust their own intuition on when it is appropriate and safe for a patient’s well being to bend the rules.
Many of the nonsensical rules in mental institutions should only apply to axe murderers, not patients who are recovering from emotional and mental distress, especially if they are recovering from emotional abuse from controlling family members, which makes these controlling rules even more nonsensical.
Aside from the higher authorities, the harmful actions of staff are usually not so much characterized by cruelty as by toadiness and fear, starting with the fear of losing their livelihood. The fastidiousness by which some staff members conform to nonsensical rules and policies should possibly qualify for a new mental health disorder in the DSM VI: “Obsessive fear of losing a lousy job” Still, I am in no position to judge, as I too, as a worker, have been in numerous situations where I acted on a strong compulsion to seek personal gain or favor in over fulfilling the mission of my organization.
While I tell myself that many could lose their jobs for breaking the rules on behalf of a patient even when the rule is ludicrous and I try to put myself in the shoes of the person whose control and authority is the most limited. I try not to forget that the pay grade for an entry level employee at a state mental hospital is actually not far above the aggregate value of a montly SSDI, food stamps, subsidized housing, etc. Sometimes there is a sliver of difference. Shouldn’t this give us some basis for widening our coalition based on economic justice? After all, I’m sure that more than a few state employees sloshing and mopping the floors of Oregon State Hospital came to resent patients who threw garbage on the floor, then used their diagnosis as an absolution from all personal responsibility.
That having been said, I hope ex patients are willing to expose some of the common practices of these large state hospitals that still operate today such as Oregon State Hospital, so folks advocating for a return to the ‘good old days’ of the asylums will get a much needed reality check; if nothing else, people writing about their experiences may help many of us resolve the anger that we feel about our loved one’s extended commitments there and expose the hypocrisy of our caring mental health system to the ignorant public.
I also want to point out that some individuals who work at OSH stand out for their kindness and humanity. One staff member while rounding up patients to go on a field trip exclaimed loudly in my hearing “I can’t imagine how it awful it must be to be civilly committed and forced to come here!” Another time, Will Hall was invited to speak to my daughter at OSH. This is hopeful! For every unkind or careless word I overhead a staff member make, I probably heard two that were kind and empathetic. Yes, they may have been whispers in private, but they give such great comfort like little candles in the dark!
But even kind words can be a double edged sword when you are a patient or a family member. Thanks to NAMI and its infamous ‘anti-stigma’ campaign, families are inundated with kindness but starved of meaningful support and opportunities for self empowerment. Kindness can be suffocating and patronizing, even diminishing, whereas actions and words that lead to true independent are far and few between.
Finally, although I agree with much of what you say and how you say it, I take issue with the wording of this statement: “When a client/patient cannot leave, this requires them to take extordinary measures after years of fuck ups and incidents that cannot get better in such a situation, including even killing of patients out of retaliation and super high doses of drugs to incapacitate and maim”
First, I will state why I sympathize with your statement. Then I will describe what I don’t like about it. When I took my daughter to the ER for ‘help’ during her first break, I personally witnessed how being forcibly drugged caused her to react violently by punching a nurse, even though she had no history of violence EVER. The greatest irony was that she was immediately charged with assault by the attending physician. Considering she was a victim of psychiatric assault and the first ‘blow’ was issued by hospital staff when they wrestled her to the ground when she tried to escape from the ‘isolation’ room, a stark room that is no more than a jail cell, and when they used goons to put her in five point restraints in order to inject her with a big needle, an experience from which she has yet to recover, without even ascertaining, first if he had a history of sexual assault, it is extremely ironic that she ends up with the criminal record, not the hospital staff. This was the first harsh lesson of anyone caught in the psychiatric system. NEVER EVER ask for any help from the system when you are having a crisis unless you are OK with having all of your rights taken away. Do NOT retaliate with violence even if someone in the system treats you with violence. Once you have the label schizophrenia, your story is not going to be believed so NEVER EXPECT JUSTICE if you experience abuse or harm in the system.
You and I probably can agree on that. But beware of inferring doctors of “killing” people out of retaliation. They will think you are crazy. It’s true that people have been killed by being put on psych meds that made them do dangerous or violent things; its true that elderly patients who are put on anti psychotics experience twice as many cardiac arrests; it’s true that many doctors put their patient on anti neuroleptic cocktails, then fail to recognize the contraindications until the patient is dead; its’ true that some doctors do not even acknowledge that psych meds cause metabolic disorders that lead to early death. But describing these actions as intentional is a slippery slope. Best not use any language that cannot hold up in a court of law. It does not promote our agenda in any way.
We should not use words like ‘killing’ because it infers murderous and criminal intent, which is highly unlikely and difficult to prove. I have witnessed psychiatrists act like petty lords in a fiefdom, rather than collaborative and curious human beings, but all of us can act this way at times. The question then becomes, when a person who is in a place of power and authority acts out of pettiness or dislikes a patient, does it cloud his/her judgement while making decisions that affect the person who is subject to that person’s control? The answer is unequivocally YES but when this happens, righting the injustice may be impossible. To date, most people who were harmed psychologically, mentally, emotionally, physically, legally or financially by a doctor have never received any compensation or apology. Most will never see justice. I think our movement needs to accept this and move on.
The casino is rigged and the best we can do sometime is to restore our dignity, refuse to play, and go on with our lives. I like the plantation metaphor. If a slave escapes to the North, one may live out the rest of one’s life as a free person in the North. But if one has a noble calling, one may risk one’s personal freedom, as some do, to help others travel through the Underground Railroad. This metaphor works for me because it captures the very real dangers of helping others migrate out of the psychiatric system when they are in a very fragile and even dangerously unstable place. People like Will Hall and Dr. Cornwall do this in their work and probably hundreds, if not thousands of others. Some family members like Cindy Fisher do this work for a loved one. But this metaphor has its limitations because individuals in the mental health system are enslaved by forces that are much more complex and numerous than an army of evil doctors or abusive family members.
Some people are under the control of abusive family members or a cult. Some people are haunted by their past. Some, like me, lack imagination for what our lives could be or if we are blessed with a imagination, we allow our dreams to be crushed too easily by others. We often are enslaved by a negative self image and a victim mentality. Though its true that low estimation of ourselves is reinforced by the cruel and inhumane treatment we or a loved one received in the mental health system, in the end, if we allow trauma and abuse to write our life story for us, rather than find a way to rewrite the narrative of our lives, then we ourselves are the ultimate slave masters.
If our imagination is capable of creating great things for ourselves and our loved ones, it is also capable of imagining very dismal futures for ourselves based on our negative experiences in the mental health system. Doctors are capable of creating very negative conditions for us and our loved ones, occasionally out of a low need to outlet their anger and resentment and I think its sometimes it is fair to call this ‘retaliation’ but from my experience, doctors who harm, usually do so more out ignorance, not out of intent to harm which means the harm is usually not a fatal form of harm and is one we can recover from. It’s as if many doctors are in a spell that they cannot make up from and until they do, they can usually offer us very little meaningful assistance other than a pill to numb us or our loved ones. If we can put our lives back together, we are twice blessed if we have the courage to go back to the doctors whose treatment was a miserable sham and off them our recovery as proof of our resiliency and their ridiculousness.
Until they stop viewing we and our loved ones as people with ‘diseases’ until they are out of this collective spell. I think that the most fatal harm that happens to us is the harm we do to ourselves.
Report comment
Madmom
I just want to say, once again, that you are a powerful voice in our movement.
Your story and the way you articulate it so clearly and passionately is very valuable to all of us who seek an end to psychiatric oppression and all other violations of human rights on this planet.
I am amazed that you have been able to maintain your moral and political compass and overall sanity given the terrible treatment of your precious child by the mental health system; she is so lucky to have you as an advocate.
Keep writing and keep fighting; I would be proud to stand next to you at the barricades.
Richard
Report comment
May the days when we stop traffic over these issues be not far off. To lay the groundwork for that day, I think David Oaks has the right approach. Emphasize Creative Maladjustment. Build coalitions with the environmental justice movement. Global warming doesn’t resonate with me although I know its important. Eradicating pesticides/GMO’s resonates with me. Toxic poisoning of our children is happening in more ways than one. Getting our people united under a wider banner is essential.
Report comment
I could not agree with you more madmom. However, this is the perspective that even some of the “well-meaning” psychiatrists miss. They equate “getting better” with cooperating and accepting the abuse. anything else is lack of insight and/or personality disorder of the narcissist/antisocial/borderline variety.
Report comment
Asylum always was a misnomer. Mental institutions never were places of asylum. Loony bin characterizes them more correctly. They were essentially trash receptacles for unwanted people, and so they remain. If prisons were no more, these guys would be singing “bring back the prison”, talk about your misguided nostalgia, and then they would be saying that doing so was ethical. Keep going. We don’t “torture” people. Why should we “torture” people when we’ve got “enhanced interrogation techniques”?
Report comment
Might be nice places to send people suffering from affluenza. It can be tough down in the cell blocks. And the taxpayer can bear the cost.
Report comment
Hi Sandy, obviously, I’ve gone back on my resolve not to post here due to the frustration I was feeling from the general level of resistance I’d been encountering. And that’s because soon after I had expressed this to you in our last exchange, I did notice a shift on MIA. I felt things starting to move forward a bit, in terms of new information and direction, so I’ve been encouraged. I guess God gave me a mind so I could change it 🙂
One reason for this shift, I feel, is that you do make it a point to be transparent about your own inner conflicts around this most controversial and vital issue, and, as others state, I really respect and appreciate that. Transparency is necessary for truth and clarity to emerge from complex situations like this.
With that said, I’m drawn to what you say, here:
“But from where I sit, there continue to be people who can not live safely in our communities. Some do not seem to have the wherewithal to care for themselves adequately and others appear to pose a risk to their neighbors. In some cases, they refuse what we have to offer and for others, we do not have adequate resources. The issue of resources is not trivial.”
I think we want to question how safe our communities are, and I’m not just talking physical safety from violence, etc.–I’m talking about emotional safety. Even the most safe-seeming environments can, in reality, be oppressive, controlling, and emotionally tortuous.
My question is: why is there always a scapegoat for this, and the community around this scapegoat never questioned and, usually, so well-protected? I think, often, there is only an illusion of integrity and respectability, when there is often something sinister and toxic going on around the ‘patient’ in question.
The power imbalance is overwhelming, when one person can decide the fate of another like this, under any circumstance. Even parents can ‘control’ their kids only so much. We’re all independent and have free will, at the core. Violating that birthright is bad news for mind, body, and spirit, I would think that’s obvious; and no doubt we have plenty of evidence of that all around us. Oppression is toxic.
And here, we’re so largely talking about adults. That’s where this really troubles me, about ‘what to do with’ adult human beings who have, perhaps, ‘lost their way.’ That’s how I’d put it, anyway, in the most general sense.
As I’ve said before, these ‘extreme states’ are the result of chronic neglect of issues, it usually doesn’t happen overnight. Communities/families tend to bury their heads in the sand until a catastrophe occurs, or someone’s defenses completely break down, which would lead to an extreme state. Usually, they’ve been beaten down over a long period of time, subtly and insidiously.
I think you’re likely to scratch your head for a long time wondering what is best for people who either cannot care for themselves in that moment—and have no one in their personal lives who can support them adequately—or for those whose lack regard for personal boundaries poses a threat to others. (Perhaps it’s a paranoid community? That’s another perspective).
But in the end, I think it’s more fruitful to wonder what to do about a society that lets things get so bad before even admitting there is a problem. By then, everyone is looking for someone to blame and wondering how to find the light at the end of the tunnel, usually scrambling, fighting, and back-biting, as a desperate and fear-based community. Nothing changes in environments like this, just more of the same, and more people losing their way, aka in extreme states. Downward spiral.
Resources are, indeed, vital, but why do we keep insisting that one side has to offer the other side anything? Perhaps ‘resourcefulness’ trumps ‘resources.’ (I.e., teach a person to fish, rather than giving him fish…). This would go a long way in creating change, mentoring others.
Sometimes, it’s just a matter of letting the light find you. Have you considered a silent meditation retreat? I guarantee that this would bring clarity to you around, at least, some of this. Just a thought.
I continue to appreciate following your evolution around all of this. Thanks, as always, for sharing so openly.
Report comment
Hi Alex,
It is nice to hear from you. Yes, I have considered a silent retreat.
While I do not disputed that our society could benefit from improvement on many fronts, that is a rather daunting task and it does not address some immediate challenges.
Report comment
Alex:
Great points! Thanks for posting. Your wrote:
“I think we want to question how safe our communities are, and I’m not just talking physical safety from violence, etc.–I’m talking about emotional safety. Even the most safe-seeming environments can, in reality, be oppressive, controlling, and emotionally tortuous.”
When psychiatrists make these judgements about a person’s ability to safely live on the outside, they often only listen to family members when the family members are extremely vocal and want their loved one committed. Sometimes, if a family member who seeks help for a loved one but is critical of the mental health system (and wants alternatives including ones that don’t yet exist) professionals will force the family members out of the equation and dialogue, making it easier to cover up iatrogenic harm. I’ve witnessed very loving family members who were active in the consumer survivor movement for change actually being accused of abuse just to quiet them up!
Either way, you end up with extreme triangulation, an issue that is effectively addressed by alternative model like Open Family Dialogue.
We live in a ‘sanist’ society and family members and professionals who purport to be compassionate are often not being honest about their own complicity in a society that is lacking in safety across the board on many levels. I believe what you are saying that the ‘insane’ are scapegoats in our society. They are!
Most doctors because of their caseload do not or cannot take the time to learn the dialect of their ‘insane’ patients. Abuse that took place on the ‘outside’ if often coded in the dialect of the ‘insane’ especially if they are caught in a double bind. They may be divided internally on how to convey information about their safety or lack of it on the ‘outside.’
The information is there but it can usually only be accessed by rare professionals who have a unique mixture of humanity, curiosity, empathy, and patience.
I once had a dialogue with a very agitated and confused individual on the street (most would say he was ‘psychotic state’ but I prefer ‘extreme state’ ) Very quickly by opening a dialogue I learned that his best friend had been killed in prison and he himself had been raped in a men’s. We hugged and parted ways that day and he stops by my place of business frequently ever since. I think he is making ground but he sleeps on the street which in some ways is a hostile, dangerous place but for individuals who have been forcibly committed, it’s actually safer from an emotional perspective to live on the streets. I’m convinced. The biggest danger on the streets is being picked up by the cops for nuisance crimes and being brought to the ER where they will refer to you with terms like ‘frequent flyer’ or ‘persistently seriously mentally ill’ or some label and drug you.
Report comment
Very well stated, as usual, Madmom.
The thing is, when it comes to the scapegoat issue, from what I’ve seen and also experienced in my own life, there are some people who walk the planet in a highly empathic way, just naturally. I know of a lot of people who say they can easily pick up the vibes of another person or in a room full of people–and not just when populated, an empty room has a ‘feel’ to it.
Some people pick this up way more easily than others, which creates a two-fold effect for a person–
First, it makes them quite vulnerable in the world, as they pick up energy so easily–whether joy or stress–so they’d fair better in a light, joyous environment. A stressful environment would undo someone with a heightened sense of environmental empathy, until they learn to have self-compassionate boundaries and healthy defenses. But that takes practice, as we are not born with these, but must learn them, from healthy adults, by example.
Also, people with this particular quality–which, once integrated, is a gift, and a tool for navigating life–tend to be more artistic because that vulnerability is what connects us to our creativity, directly. When we are in our truth, we are inherently vulnerable.
So yes, if everyone worked together to create a better environment rather than this dark, dense, oppressive, toxic entity that is called ‘the mental health system,’ then I imagine pretty strongly that healing and clarity would be achieved.
But then again, that kind of describes the world right now, too, doesn’t it? So where do we begin? Something needs to lighten up somewhere.
I think right now, we’re all scapegoats one way or another, considering the political and socio-economic climate, on a global scale.
Clients try to communicate a lot to families and professionals that is simply not understood by the mainstream mentality. That’s where we seem to hit a snag, and it’s somewhat tragically ironic, because if they are the ones carrying the social ills predominantly, then they are also the ones with the solutions.
So I think it’s a good idea to make it a priority to bridge the communication gap here. That’s where I’m never quite sure if progress is being made, although MIA is a good gauge for this, in general. It’s gotta start somewhere!
Report comment
I wanted to amend where I say self-compassion and healthy defenses are not natural but learned. I got that backwards–we are born with self-compassion, but that can be unlearned in an out-of-balance environment. Trauma certainly undermines our sense of personal boundaries.
Healing is a matter or remembering our self-compassion.
Report comment
I mean, a matter OF remembering our self-compassion.
Report comment
Asylums are a more humane alternatives to prisons…wow.
When one looks at the chart it’s apparent that in the period fro 6s to 80s institutionalization went down across the board so it’s not like if you empty asylums you have to lock people up in prisons – they managed to avoid that for like 20yrs apparently. It may be worthwhile to think what happened, outside of psychiatry itself, in the 60s and what happened politically n the 80s and you have your answer. 60s was an explosion of creativity, struggle for self-determination of various groups of people, sexual revolution and so on. 80s were a comeback of authoritarian era under the banner of neoliberalism. Oppresive systems lock people up – they use both prisons and asylums for that purpose. the answer is not to ship people from one to the other, the answer is to change the system.
Report comment
Alex:
I think you hit the nail on the head when you wrote: “it’s somewhat tragically ironic, because if they are the ones carrying the social ills predominantly, then they are also the ones with the solutions”
David Oaks expressed this same sentiment on several occasions, that people who express extreme emotional or mental distress, even to the point of being being disabled, are seeking recovery in great numbers through community and personal solutions as well as through personal empowerment and hard work. These recovered individuals are the ones who hold the key to the recovery of our entire society from man-made caused problems like global warming.
If you know someone who has recovered from a deep depression, an ‘anxiety disorder’ or even ‘psychosis’ ask them for advice the next time you feel frightened or disturbed! These individuals are the greatest mentors, teachers, and friends alive! Embrace them and support them in our community so they don’t have to waste their precious time and resources obtaining certificates and credentials to do their important work (not to undermine the accomplishments and importance of people who did obtain such credentials).
If a person is willing to share his/her recovery story in person, let alone to a large audience of peers, professionals, community of faith, etc. pass out flyers and posters and get out the word! Psychiatric survivors are made of a steel. They are OK with being creatively maladjusted and as such, they often harbor important information about saving our entire species from almost certain destruction. If we do not learn from psychiatric survivors, the best hope for our society to become more inter dependent and cooperative will go down the drain.
As Mr. Oaks said, ‘Normal behavior’ is killing the planet. Science confirms this. Pesticide use, heavy metals in our water and soil, air pollution, radiation leaking from outdated chemical weapons plants, wars and prisons, diminishing ocean fisheries and salmon runs, over-logging, desertification, overpopulation, economic pressures due to globalization and the break down of indigenous cultures, the role of extreme poverty and increased prison rates leading to the breakdown of traditional family units in Western society, just to name a few ‘REAL’ not imagined dangers. All of these man-made dangers are very disturbing. When people who are emotionally disturbed are completely misunderstood by mainstream psychiatrists and harmed by restraints, isolation, and use of toxic medications, its not just personal loss, to individual, it is a tragic loss that affects us all!
Those who recover from horrific psychiatric harm and abuse—their stories are being virtually ignored by mainstream mental health professionals and the media (I wonder why when those who often have the best personal outcomes generally have not so flattering things to say about those who practice the healing arts)
Increasingly, I believe that psychiatric survivors, consumers, and family members need to continue to fight to revolutionize the mental health system but we shouldn’t continue to do it within a bubble or a vacuum. We should widen our movement’s goals to include environmental and economic sanity and justice for all by showing up at the protest marches of people who are fighting the good fight under different banners. We should reframe the crime victim’s movement to include crimes agains survivors of psychiatric assault.
We should reframe the ‘anti-stigma’ campaign, taking away one of NAMI’s greatest talking points, reframing it to include the important stigma of those who were slandered, dehumanized, or diagnosed with a manufactured illness and forced to take toxic medications or ‘treatment’ that made them much much worse. We should address the stigma of being scapegoated as a danger to society when in reality, the most dangerous people of all live in the state department, the Pentagon, at the policy level, etc.
Report comment
“We should reframe the ‘anti-stigma’ campaign, taking away one of NAMI’s greatest talking points, reframing it to include the important stigma of those who were slandered, dehumanized, or diagnosed with a manufactured illness and forced to take toxic medications or ‘treatment’ that made them much much worse. We should address the stigma of being scapegoated as a danger to society when in reality, the most dangerous people of all live in the state department, the Pentagon, at the policy level, etc.”
My goodness, this is exactly what the content of my film explores, to a tee. That was exactly the intention, to reframe and take back the issue of stigma, and make it relevant to clarity, understanding, and HEALING.
I made the film while on disability, using my best resourcefulness, faith, and trust in the process. It’s not a perfect product, but I know it gets many of these points across. And it’s just us, from the system, and a couple of our spouses, no outside ‘experts,’ just our truth. I thought it was one of a kind, in this regard.
I was invited to submit it to MIA film fest, from the trailer, but it was then rejected. It’s been highly regarded and acclaimed in many circles, and it also led to effective activism in San Francisco, but aside from a couple of thumbs up here, it has not been favorite among this crowd, for some reason. I’ve yet to really be able to put my finger on it. But yes, I totally agree with you and again, this is what I have been exploring, specifically, which is what led to my making Voices That Heal.
Thankfully, it has served me well as self-advocacy and it did precipitate a big transition in my life that has been favorable, so for me it was extremely healing, as well as for my family. I’m not promoting it (again) here, as I write this, I’m just saying it’s ironic. Indeed, to my mind, the stigma is the issue which muddles everything up, personal prejudice can be hard to ascend, but that’s a wonderful healing, when we own our prejudices.
NAMI and other advocacy agencies are simply exploiting this issue for funding and to create more business for themselves, but they are, in reality, only perpetuating stigma and discrimination. Healing is impossible in these environments.
Report comment
Alex: the Film sounds awesome! Can’t wait to view it. I couldn’t agree with you more that NAMI is exploiting the stigma issue to make money with the end result that they actually perpetuate stigma and discrimination, especially the stigma against those who are non compliant; but I know good people who are active in NAMI trying to change it from within. I salute them! I often think we don’t give insiders like individual NAMI members and doctors like Dr. Steingard enough credit for their valuable efforts. I think in the future that it will be easier for mainstream professionals to come out of the closet agains the practices and policies of their own profession or guild. We are standing on the shoulders of giants, the first generation of survivors to organize. People generally want to be on the right side of history and I think this will apply to a lot of people who don’t yet feel safe enough to engage in this dialogue openly out of fear of losing the respect of their peers. But in the future it will become safer to speak out, as the rising tide of evidence becomes generally accepted about the true nature of many psychiatric medications; that they are brain damaging, especially neuroleptics. Sadly, it will probably help out that big Pharma, will put their vast profits into other avenues of research other than mental illness.
I think we should be very respectful of those who have been deeply harmed. Their voices are important.
but so are the voices of professionals who are trying to change things from within, including those in NAMI. One’s livelihood is a terrible thing to risk; Doctors too have families to feed, clothe, etc. and they too, have been duped by the Universities where they received their credentials. I know this statement alone is liable to anger some. Perhaps we could have town meetings to allow reconciliation to occur as Nelson Mandela did after apartheid ended.
I think it would be wise to create more safe communities for dissident psychiatrists to come out of the closet and avoid using a rare forum like this one, as a reconciliation platform. Sadly, there may never be any opportunities for individuals and family members to enjoy full compensation and spiritual reconciliation. Many are already in grave sites, many of them unmarked. Somehow, we must all move forward together in this f**cked up nightmare of a mental health system and move this mountain of ignorance and indifference together but we need a diversity of voices including those who are justifiably very angry about the torture and abuse they endured as well as mainstream voices. Unity is not going to be easy but it could make or break how effective we are
Report comment
“People generally want to be on the right side of history and I think this will apply to a lot of people who don’t yet feel safe enough to engage in this dialogue openly out of fear of losing the respect of their peers. But in the future it will become safer to speak out…”
Fear of losing respect for speaking out, embodying and standing in one’s truth? That seems like a double-bind to me.
I say the future is now, we have to MAKE it safe by breaking that ground. Many of us have, evidenced here every day. I’ve been in the face of the system, spoke my truth in legal mediation, and in my film. The agency with which I was associated at that time was not aligned with the truth of my film, I called out the system, which was, in essence, their meal ticket. But it was truth, that was most important here, given what we’ve all been facing with such a myriad of messy ‘mental health community issues.’
What all of this cost me professionally on one level, I gained more than I could possibly say, in the long run–freedom, mostly. Also a sense of myself, which is what I was after. That’s where I found my inner peace, finally. I felt good about myself, in a way I never had–resolved.
If we fear speaking our truth, then we are letting the oppressors and power abusers win. We all have our styles, I try to be respectful. Sometimes I get passionate. I always strive to be clear and direct in how I communicate and I always appreciate the same, I think it leads to needed clarity. But that’s just me.
However one does it, I always highly recommend facing that particular fear, taking a leap of faith, and speaking one’s truth. The truth really does set you free, not just a hackneyed philosophy. It’s truth.
Report comment
I was a psychotherapist and now all my former classmates and colleagues won’t get near me, after I spoke out. They never had my journey on the wrong side of the system, so they haven’t a clue about this. Instead of listening and dialoguing with me about it, they get offended and abandon. That says a lot to me.
I lost the support of peer group after peer group as I awakened to all that was occurring around me in my journey through the system, from group to group, staff to staff, etc. It got pretty nasty a few times, but I learned a lot about the culture from exchanges like that.
In the end, it was my guidance, because it led me to all that is now, and I have no complaints, not a one. My affirmation became: then these are not my true peers. Eventually, I found my community of healers (and artists!), with whom I’m in perfect synch. That’s how it works!
Report comment
Hi Alex,
I think we need a support group for “professionals” who speak out and become ostrsized by their professional groups, The Survivor group is skeptical
and won’t really let us be part of that club, so maybe a club for the oppressors who left the system and want to be apart of the voices speaking out! OR as I said when I left the system, there were lots of people with lived experience at my farewell party, they joined me during my “speech: and I said to the audience remaining (the “professionals”…These are my peers , but they won’t let me in the club because I haven’t been locked up and forced meds so I don’t qualify…but these are the people I like to hang out with and I identify with! How can we join forces and be one?
Report comment
Hi Yana, well, as far as which ‘club’ I would belong to, my identification has changed quite a bit over the years—therapist, client, ‘peer,’ psychiatric survivor, advocate, activist. I’ve been in agreement and affinity on one hand, and also at odds, on the other, with each one of these communities within the mental health industry. As a healer and teacher, I identify with a community outside the mental health world.
I was a therapist-turned- ‘consumer’-turned-disabled-turned-awakened, if that makes sense. That’s the basic outline of my healing trajectory and spiritual evolution.
At present, I identify with those who are looking to create a new world of healing. That’s been my work in the world, as a result of my journey. The deeper I got into it, on all levels, the more I could see that this mental health industry was doomed, in terms of what we have going on now. This was before I discovered MIA. This community validated my experience, and that relieved me a great deal. Until I found this website, I was the only one I knew that was speaking out this way. My fellow ‘peers’ were petrified of speaking out, and were angry with me for doing so, as I was ‘rocking the boat,’ and challenging the mental health cultural programming.
As far as creating new healing avenues, I feel I’ve gotten off to a good start. I did a lot of training as I healed from disability, in various schools of thought. It was an extremely interesting and enlightening training as a healer. I’ve been working consistently in this capacity for the last ten years, expanding and evolving as I go. I’m happy with how it’s all been growing, suits me perfectly.
Here’s my website, if you want to check it out, this is my particular brand of healing and activism. I add ‘manifesting’ to the list, because I discovered that this is where healing can be fun and real, rather than tortuous and illusory.
http://www.embodycalm.com
There’s an interesting documentary that I made on the last page, if you feel compelled to check it out, where 6 of us from the ‘peer’ culture talk about our experiences going through the system. We’re not all of like mind, but there is overlap in our truths, for the most part.
Report comment
Alex:
I appreciate your sharing how your identity changed during your journey and the experience of being ‘shunned’. I think every individual in this community, at one time or another has experienced a ‘shunning’. If you are a dissident mental health provider, you may be shunned by consumer groups, psychiatric survivors, and other professionals, sometimes all three. Often, when we are shunned for no more than using language that triggers another individual. For instance, if you are a provider or a family member, using the nomenclature of ‘mental illness’ may trigger rage from a survivor who does not identify with a label that he/she was given erroneously or during a time when they were robbed of their rights.
If you are a consumer or family member and you use the term ’empowerment’ and ‘human rights’ you may trigger the rage of a psychiatrist who is awash with bureaucratic paperwork and may wrongfully blame civil rights activists for making their job more difficult.
It seems at every turn one is searching for a safe community where one can speak one’s truth but there is a huge divide on what constitutes fixing the ‘broken’ mental health system. Within this divide are individuals who have been so diabled by the system itself, that no-one can presume to speak for them in this community (even though people on both sides of the spectrum do so constantly)
Everyone in this community has a dog in this fight to peacefully revolutionize mental health care in the US. In the wider picture, our struggle is a part of a larger struggle to save our planet from destruction and to create justice and equality. But our movement is not united and we don’t have a broader coalition yet to be effective and shift the poles of the debate. Realizing this, we are trying to attend to these challenges.
One thing that keeps us from being united is the disparity of privilege and the range of physical and mental abilities of consumers. Some consumers have been so denied of their rights they cannot even access the internet to join this community. Some have been so cognitively harmed from long term neuroleptic use that they cannot use a computer keyboard. Some are blind or have had their limbs surgically removed due to diabetes and must get around in a wheelchair. Some consumers have family members who limit their exposure to outside information unless it has been filtered by NAMI. I imagine, some even have Stockholm syndrome.
The other great divider is privilege. Our community is characterized by poverty, unemployment, and homelessness. We can’t expect to enjoy unity when some of us live comfortably in houses with heat and internet access. Some have had to make terrible choices to comply with a coersive mental health system to receive subsidized housing.
I propose that a person in subsidized housing who risks ‘biting the hand that feeds’ by being openly critical of community mental health care system in his/her community and who does more than vote on pizza and attend Alternatives is taking the same risk as the psychiatrist who speaks out in his/her community about the lack of choices and human rights in the mental health system and risks the ire of his/her peers.
Some members of this community literally profit from the current system and enjoy the American Dream. The current system has harmed many. Those who have been harmed the most live in poverty. This is a divide. How can one whose poverty is arguably caused by iatrogenic harm speak calmly with one who profits from the system?
Though some have courageously risked their professional careers to speak out with the hopes of changing the system are being shunned so they are risk of burning out or losing their insider status. In which case, the movement loses another potential ally.
Some psychiatric survivors enjoy more economic privilege and social capital (friends, networks, etc.) than those who are still struggling with issues such as poverty and homelessness that they arguably wouldn’t be experiencing had they received more humane and effective treatment to begin with.
There is also an element of luck and unfairness in the current system which is a crazy patchwork system of uneven care and opportunities. Some people have access to peer counseling and housing and enjoy favorable public health policies because their community has one or more dynamic peer leaders. Some even get lucky enough to have a Sotoria experience. Yet others get killed by their medication or they get locked up in prison permanently.
Some psychiatric survivors get a shot at the ‘American Dream’ while others, permanently disabled by tardive dyskenesia, from years of being drugged, live in foster homes where every decision is taken away from them, except how to spend $30/week. They may walk with a funny gait and people may avoid them on the street. Many experience the ultimate shunning.
Family members advocating for a loved one, want to shout out “I don’t want my loved one to end up rocking back and forth!” to the treating psychiatrist but they dare not out of fear that their words will be misconstrued as delusional (the medical notes will read: parent lacks insight and remains in denial about daughter’s condition) Plus, the words will be portrayed as lacking in compassion for those who do rock back and forth. “Look how that activist or family member talks disparagingly about these poor people with diseases who are fortunate to have our care and support” If one accuses the psychiatrist who is treating one’s loved one of harming the other patients on the ward, they have terrible ways of retaliating against one’s loved one and the most terrible thing of all, most doctor ;retaliate’ are completely unconscious of their terrible abuse of power and authority. It is as if they are in a dream, a stupor or a spell.
I am speaking as a family member but I am also emboldened to channel my 24 year old daughter if she were to visit this site. When one visits this community after spending days, months, even years in the back ward, one may obtain a bitter consolation. So many individuals in this community who successfully made it out of the system. Yes, this can provide hope. But one may be left to wonder, do the contributors in this community have more than words to assuage my isolation and suffering? I just want a sanctuary where I won’t have my experiences discounted and pathologized. I want housing but I want freedom of choice, not doors that lock. I want dignity and respect and treatment that doesn’t harm me or make me cry in my pillow at night. I want an end to this nightmare of institutionalization and civil commitment. I just want an end to anger and hate against this f**cked up system.
I agree that we need support groups for professionals. But it would be wise for professionals who are concerned about being shunned by their peers to remember the level of shunning that they endure is a fraction of what our loved ones endure on the streets.
Individuals like my daughter who occupy the lowest rungs in our society because they are labeled ‘psychotic’ or because they hear voices, are shunned in a way a doctor or psychologist will ever experience.
And to add insult to injury, there is an even lower rung reserved for people like my daughter who are ‘non compliant’ or who ‘lack insight’. They are civilly committed over and over and over again until they have adopted the code of conduct imposed on them by the mental health system to live half asleep, with no motivation, no desire, no ability to feel emotion, no dreams. As long as they take the medication that makes them sleep 12-16 hours daily, they will be accepted.
Report comment
Madmom, I think you’re describing society at large. At this point, I think virtually everyone on the planet is feeling like a prisoner, one way or another. We’re going through a time of great change all over the world, and it’s not easy for any of us. The goal of this change is for each of us to know our personal freedom. That’s a pole shift.
Indeed, our society has been one based on the ‘rich and powerful’ exploiting the ‘poor and vulnerable’ in order to achieve ‘the American Dream.’ That dream, obviously, is a grand illusion, if it was created by robbing others of their soul and happiness, which is what had occurred, through blatant deceit and disregard.
The world and humanity are shifting, in every respect, and as you imply, those who have been privileged by this inequality, mass deceit, and corruption are not making it easy for that change to occur. In reality, underneath all that wealth and position, is a lot of fear, even paranoia, I would imagine. Those of us speaking up and out, however, exemplify courage and truth.
I’m optimistic at this point. I think the old systems are breaking down and we will see more and more evidence of this daily. I think there are enough of us bringing in the new healing wisdom and how it applies to creating a more harmonious and peaceful world, that we’ve shifted the axis here.
People are waking up in droves, daily now, in all areas of the global population. So many of us are really tired of this constant tug-of-war, and want, more than anything, to see an integrated world. I believe we’ve made a big difference, and the evidence of that will show up soon, unmistakably. That’s my gut feeling.
Report comment
I also wanted to say–I wouldn’t say that I changed my identity as much as with whom I identified evolved over time. I played different roles in the community, not turned into different people. My spirit identity has remained constant.
How I prefer to see it is that I explored different aspects of my spirit and personality. That would be the advantage of playing different roles. Personally, I enjoy going through life this way because it exercises all of me, not just this narrow little aspect of myself. That’s terribly constricting to me.
Probably why I took to acting so well! That’s REALLY an opportunity to explore deeply different aspects of ourselves. It’s really a fun endeavor, and incredibly enlightening, when we allow different aspects of ourselves to come forward in life. Fear of speaking and showing up, in our totality, is something we need to get over, if we are ever going to achieve personal freedom and inner peace.
Report comment
Yana, I also wanted to make clear that when I say, ‘a new world of healing,’ I’m talking about ascending any need for money when it comes to doing healing work in the world. Once money is involved as a necessary component, healing can easily become corrupt. Healing is a spiritual issue, not a material one.
I am one of many energy healers on the planet, who work with the light. That’s the shift in healing. In truth, healing has nothing to do with how we, in our western culture, have been perceiving it all our lives. It’s an entirely different paradigm of thought, where healing and spiritual evolution become a way of life. That is how one achieves health and well-being, unmistakably. At least, that is my truth.
Report comment
They say, Bring back the asylums, and untold numbers nod in agreement. Asylum is such a sanitary word. It promises safety and care. I wonder if they decided to clarify, how many people would still be nodding mindlessly in agreement. How about, Let’s bring back numerous, unexplained, neglectful, and violent deaths… rampant instances of sexual and physical abuse, deplorable conditions that mirror those of auschwitz at the height of Mengele’s reign.. Let bring back over medicating to the point that patients are unable to finish single sentences… Because that is what the asylum brought with it.
Report comment
Since some of my comments were moderated I’ll try to put my point across in what is I hope perceived as more “civil” way. I’d like to bring up the topic of coercion because it seems to permeate any discussion about asylums in this article.
Dear Sandra,
you are one of the MIA’s bloggers who represents the so-called “critical psychiatry”. While I do appreciate your efforts and criticism regarding the current state of affairs you also come across as a person who constantly defends the ability of psychiatrists to force treatment upon their “patients” and admit that you, however reluctantly, are involved in such practices. You also seem to allow for such things to happen not only when people are supposedly a “danger to others” but as you write: “Although I acknowledge there is no fine line, I am talking about people who are not engaging in discourse which I can follow.” and “In some cases, they refuse what we have to offer and for others, we do not have adequate resources.”
You seem to avoid engaging with many psychiatric surviviour commenting at MIA, including myself, who accuse you of being a human rights abuser due to your stance on and practice of forced psychiatry. You’re explaining that by seeing this as an insurmountable difference of opinions and you defend your position by saying you have no better choice of action.
First of all I would like to say that you do have a choice on the matter. You can simply refuse to participate in any form of forced treatment and work only with people who want to engage with you voluntarily. I don’t know if that would in anyway affect you negatively in terms of your career or social stance or what not but it certainly is an ethical choice. Nobody is threatening you with violence and coercing you to such practices so it’s hard to see it as anything else but a choice.
Secondly, if you agree with my assessment that this is indeed the “lesser evil” type of choice you’re making than I’d like to challenge you on that. Forced psychiatry and coercive “treatment” is torture. You don’t have to take my word on this – UN has called it inhuman and degrading treatment and it should be enough to listen to the testimony of countless psychiatric surviviours and their loved ones who use the very words: TORTURE, RAPE, ABUSE. Denying the fact that forced psychiatry is exactly that is denying reality in much the same way as the people who defend enhanced interrogation techniques defend waterbording. I understand it that you have yourself never experienced being “at the sharp end of the needle”, having your liberty, dignity and physical and psychological autonomy taken from you in a violent way much as many of the torture defenders never experienced waterboarding. It’s sad to see that you find it hard to or are unwilling to empathise with us nonetheless. There were some people who volunteered to be waterboarded in order to prove it’s a OK and came back strong opponents of this form of torture. I don’t advocate you try the same with the forced psychiatry because I do not wish this kind of hell on any human being but I simply can’t understand why you don’t seem to have enough empathy on that to understand how profoundly inhuman it is.
You often mention the situations when you think it’s justified to use forced psychiatry. One of them is imminent threat of physical violence. In this case I think nobody can refuse you the right to defend yourself or those around you. However, you also have to understand that it may be you who is creating the violent situation in the first place. I gather these are the situations which most often occur when someone is being brought to ER or psych ward against his/her will. That means, unless the reason for bringing them in the first place is violence, that it is psychiatry which generates the distress in likely already vulnerable person. Taking away someone’s freedom and forcing them into a psych ward is a treatment that provokes violence, provokes aggression. You can’t treat people this way and then expect them to be reasonable and docile and what not. This is ignoring human nature or it is social control pure and simple. You also mention that when you can’t follow somebody’s train of thought (presumably because they are psychotic) or when they refuse to cooperate with you you have “no choice” but to force treatment upon them. You should understand that the first instance is an extremely arrogant way of viewing the person as we all know that even the most delusional people have some internal logic and that is the representation of their inner understanding. You should try to understand this logic instead of violating this person’s dignity. As to people who “refuse what we have to offer” I suggest you make a mental exercise. Imagine somebody takes you, against your will and often in a violent manner, from your home of the street, takes you to the place you don’t want to be (sometimes because you’ve already been to a place like that and suffered horrific torture and abuse) and you’re faced with a choice: either you chose one of our nice “treatments” for you or we will force them upon you, violating you physically in the process. I know some people will maybe go with it for a moment being while resisting in tehir heads but there is a certain part of the population, usually the people with most anti-authoritarian tendencies, who will feel that giving in to your demands is more degrading that anything you can possibly do to them with the drugs and restraints and all the forms of psychiatric violence. And it does not really matter if you offer them some nice psychotherapy, or yoga, or whatever alternative programme you may have – the sheer fact that this is coercion will prevent them from ever trusting you or wanting to collaborate with you and it’s not hard to see why. Again if you’re expecting anything else you are ignoring human nature and the better part of it – the one that resists oppression.
That brings me to my final point. Even if you disagree with me on everything I’ve written so far and for you the perceived end of coercion justifies the means maybe this one last point will make you change your mind. Torture does not work. Coercive treatment does not work. It is worse than that – it’s counterproductive. Just as CIA torture chambers have created more terrorists and more threat to the US and hatred and fear – in the same way psychiatric torture creates anti-psychiatry. It makes people hate you, despise you and never ever under any circumstances want to work with you. Even if there are ways taht you could possibly help these people – you’re essentially guaranteeing they won’t listen to you, won’t cooperate and in the end you’re hindering they recovery.
Just to add a personal touch to this probably already too long comment: I tried to commit suicide because of psychiatric torture. That was the one and only time in my life that I was really 100% determined to end my own life and took steps to do that. And I did not because I was “crazy” or hallucinating – I did that to end the torture which was unbearable. So if you think that mine of others comments here are offensive to you when you defend your ability to use coercive psychiatry you should bear in mind that you may be responsible for acts of violence against self and others committed by the victims of this system simply because that is the only choice they are left with. If you’re OK leaving with that responsibility then I guess there is nothing more I or anyone here can say to change your mind.
Report comment
B,
I appreciate your comment, “B on January 30, 2015 at 8:21 pm said…” and Sandy I appreciate your attempts at trying to change a broken system.
And I think the real issue is that we are dealing with a completely corrupt system, one with some good people working within it but with too many who abuse the power they are given within that system. B, I ran into a similar situation as you, and felt the same way. And I think my situation points out how corrupted the system has become.
I was hospitalized against my will twice. Once because I suffered from a sleep walking talking issue and my husband called the paramedics. I awoke when the paramedics arrived at my home. I explained my dream and agreed to just go back to bed. Five paramedics dragged me out of my own bed, while the sixth paramedic told the other five that what they were doing was illegal since I was neither a danger to myself nor anyone else. I ended up being put on a hypnotic drug and shipped by doctors at my local hospital, which was no longer covered by my new insurance group, due to prior malpractice, to V R Kuchipudi. Here’s his arrest warrant seven years later for doing the same thing to many other patients:
http://www.justice.gov/usao/iln/pr/chicago/2013/pr0416_01a.pdf
The second time I was hospitalized against my will was for lying in a park, minding my own business, staring at the clouds. I was also trying to mentally come to grips with the reality that I had been railroaded into the psychiatric system by a pastor who wanted to cover up child abuse and a PCP who wanted to cover up her husband’s “bad fix” on a broken bone of mine. I was shocked by the betrayal of my ex-religion and doctors, but had just finished chronologically typing up my medical records with the proof of this. I was forcibly given a $5000 physical, resulting in a “medically clear” diagnosis.
Then, without signed HIPPA forms, this hospital inexplicably sent this completely healthy person a long distance back to Kuchipudi’s psychiatric partner in crime, Humaira Saiyed. She, of course, injected me with Geodon, which I had told her I was allergic to and I also told her it was against my religion to have neuroleptics forced upon me. The “professionals” at that hospital commented in their medical records that they’d never seen such an adverse reaction to a neuroleptic. So I ended up being forcibly treated for a non-existent UTI.
The “system” is completely corrupt, and is harming innocent patients for profit, and more insidious greed inspired medical reasons.
Report comment
B,
I will do my best to respond.
I am sorry for the way that you have suffered. However, I can only take responsibility for those situations in which I have been directly involved. I have no idea what I personally would have done if I had encountered you at some point in the past.
I am not sure where you got the impression that I think it is justified to commit someone to the hospital whose only problem is that he is talking in a way that I can not understand. The laws in Vermont only allow a person to be committed to the hospital if there is a risk of danger to himself or others and I follow that law. I understand that there is often a considerable amount of judgment in making that determination and that is another reason why I can only take responsibility for the decisions I have made.
Your thought experiment about the person being brought to the hospital is a good one but I am often aware of people who have not been brought anywhere. They are living in their homes and are threatening the people who share the space with them. No one has ever intervened. The people in the home are frightened and call out for help. Interventions to try and understand the problem, meet the person in a respectful and humane way over weeks or months fail, and one day the person acts on the threats that have been made for months. These are individuals for whom I would love to offer some sort of respite but they reject everything we have to offer. What about this situation? Why are the rights of one individual more important than the rights of the others in that space? Multiple people are traumatized in these situations. Now if you tell me that you would prefer to have the person taken to jail,. that is fine. You have a right to your opinion but that brings us back to the article that was the subject of this post.
When you say the violence is due to some action on my part, I will just say that this is not what I observe. Those of you who do not believe intervention is ever warranted are likely to find some proximal cause, some proximal trigger that if addressed adequately could have led to another outcome. There is no way to refute that. I will just say, please come join us. We are trying hard to help everyone live with dignity and autonomy in the community. I am being overly scrupulous when I say I am directly involved in committing people to the hospital. Most of the time, when people I work with end up committed, I was not directly involved. Often something happens in the community and they come to the attention of others who intervene. Prior to that point, I and others have often been working hard to find some way to help and to prevent that outcome. When I say I do not know what to do, I am admitting that the help we offer has not been adequate.
You and others have asked for more specifics. I would prefer to be accused of being evasive than to take the risk of violating someone’s privacy. I live and work in a small town. I already take some chances by blogging here. There are certain lines I will not cross even if it means incurring the criticism form you and others.
I agree that forced treatment addresses a short term crisis but does not usually lead to a long term resolution. I do know of some people who after the fact were appreciative of being brought into a hospital. Some of them spent large amounts of money or ruined relationships and look back in regret over decisions that they believe in retrospect were faulty. I realize that you will likely not believe me or insist that their beliefs are due to their being co-opted by the system. So be it. We all live in our own realities and that is just some of what I have experienced in my life.
I understand I have a choice and I try my best to try all other means first. I understand that you would prefer me to retire and all I can say is that you probably will not need to wait too much longer. But your charge that I do not engage, is just hard for me to understand. I have written about this topic and tried to respond to the best of my ability. It seems that the only “engagement” that would satisfy you would be to fully accept your position. I am sorry that I am not able to do that.
Report comment
Dr. Steingard,
Thank you for responding to B. in such a thoughtful way. You raise really good points and I don’t envy the position of professionals who are trying to balance the rights of multiple individuals in complex situations. You bring a valuable voice to the debate on whether psychiatry, as it exists today is medical science, a healing art, or a form social control (or a mixture of all three) let alone what psychiatry should or could be.
Your response goes a long way towards healing the anger I feel against psychiatry for harming my daughter. I may never 100% trust all doctors again, as I once did, but it feels really good to hear a psychiatrist who is willing to talk this way, including to people like me who identify with having a loved one who being harmed by psychiatry. She is locked up and has zero options to titrate off or change her medications.
I am very grateful for your donating your time to the Foundation for Excellence and for explaining your views in this community.
I only wish there were more psychiatrists like you in the system!
Report comment
1. In the first comment on the article Vortex asked you: “So, my question is: does such description fit devoted rebels, dissidents, non-conformists etc.? These are people who are usually described (and treated) as “asocial” and/or “antisocial” not only by authorities, but also by the “silent majority” compliant to authoritarian dominance. Should their protest and resistance be labeled as “delusional” (which, by the way, happens quite often)?”
Your answer: “Although I acknowledge there is no fine line, I am talking about people who are not engaging in discourse which I can follow.”
I may be misunderstanding your stance but it seems to me like you’re equating the fact that someone does not want to cooperate and talk to you in a manner you understand may be a good enough reason to use coercion against that person should they behave “anti-socially”. You acknowledge this is a fine line and indeed it is. It may be difficult for me to comprehend the logic of Mr Brevik (an ultimate “anti-social” guy example) and I’d surely not be able to talk to him in any productive way but I’d be far from deeming him mentally ill (which was attempted) and claiming he needs some medical treatment. The only “treatment” he needs is prison and resocialization if that is ever possible. In the same time there are certain forms of “anti-social” behaviour that are political which I totally agree with but other people would deem delusional and disruptive. Using this kind of logic is making the criteria for committing someone etc. subjective and ripe for abuse. You may be judicial with doing it or you may think you are but there are plenty of people who don’t care. Not mentioning the clear cases of locking up political dissidents and whistleblowers and no, I’m not only talking about China.
2. On the criteria of “danger to self and/or others”: I know this is the law but I don’t see why that should be an excuse. If the law is wrong and inhumane one should engage in civil disobedience against it. In this case it’s easy because this is the law you are volunteering to enforce – it’s not like you’re going to be put in prison yourself should you stop working in an environment that requires you to do that.
There are several reasons why these criteria are wrong. First of all the ability of psychiatry to predict if someone is “danger to self and/or others” is practically zero. So this is a law from Minority report – I have a magic mirror into the future which tells me this guy will try to kill himself or that woman is going to strangle her baby. That is simply impossible to predict with any sensible validity and by having this standard thousands of people get tortured because you or someone else making a danger assessment based on your gut feeling. By the same standard you should be locking up any guy who makes a sexist comment and is drunk because they are in danger of raping someone. That’s not a legal standard that would be allowed in any other circumstances. If someone has already committed a crime (and running around threatening people or setting something on fire etc. are crimes) then we have a different situation. Merely being delusional or agitated or refusing “help” is not and should not be illegal.
In terms of “danger to others” specifically I’d also like to mention that people are often brought in against their will for bs annoyances or other none offenses or nothing at all and often are treated with violence from the get go in the process (I have experienced that myself). If that person then gets reasonably agitated and angry – here comes “danger to others”, “verbal aggression” and so on. In other words – coercive psychiatry creates the situation which it claims to be preventing. I’d say that every time someone is brought to you against his/her will and calls you every name in the book or refuses to talk to you or becomes “agitated” – that’s a perfectly normal response whether they were delusional or not to begin with. I know it may not look like that to you because you lack this perspective but that is the fact. You can’t treat people like violent criminals and expect them to be OK with it or subject them to loss of liberty, dignity and often physical and social humiliation and then blame them for getting aggressive.
“Danger to self ” should not be a crime and not be a reason to claim someone is legally insane and/or should be committed. I have the right to kill myself or to harm myself and claiming otherwise is not only ridiculous but also violation of my human rights – the ability to decide about myself. Psychiatry arrogantly claims it can force people to live but then if someone commits suicide on their watch or shortly after getting out of the psych ward they refuse to take any responsibility. This is the most insane and hypocritical part of the whole system to me and I really can’t comprehend the mindset behind it.
3. “They are living in their homes and are threatening the people who share the space with them. (…) Now if you tell me that you would prefer to have the person taken to jail,. that is fine.”
That is exactly what I suggest. In this case the only reason of bringing them anywhere is isolation to prevent harm to others which is achieved by the prison. If person refuses any “treatment” that means the only “treatment” you can effectively use is drugs. Which don’t solve anything. You can’t force talk therapy or gardening or yoga or whatever on someone who does not want to participate – you can only torture them with needle rape. That’s hardly more humane than simply locking him/her up in jail. In which you also have rehabilitation programmed (or should have) which can provide this person support should they choose to “get help”. Unless they choose though the function of either institution is locking them up but the “hospital” only adds additional corporeal punishment that should be illegal.
4. “We are trying hard to help everyone live with dignity and autonomy in the community.” I think you miss the point. I mean – the very existence of coercive psychiatry will make your job on that harder if not impossible. You may be as nice and as helpful and as well-meaning as you like – the fact is if the person on the other side knows you have a legal right to torture them you’re the enemy. From the get go. Before they even see you, talk to you, before you do anything. It is counterproductive. So sometimes it may seem to you you did everything right and that person will still refuse to talk to you and barricade him/herself in their home or throw rocks at you should you approach. Especially if they already have experience with someone who may not have your ethics. And you will see it as unreasonable and “crazy” but you simply have no idea. I’m not saying it’s always you who are at fault because you did something – you’re at fault because you’re a part of and therefore legitimising these system of abuse. Systemic abuse can’t be fixed by well meaning individuals trying to limit the abuse – it can be fixed by bringing it down.
5. “I do know of some people who after the fact were appreciative of being brought into a hospital.” Sure, so do people who commit a crime, do their time and get rehabilitated. It doesn’t mean that you should be doing it or calling it medical. Simply put – the potential benefit to a few does not justify a legal system that allows for profiling people, pre-crime and torture.
6. “But your charge that I do not engage, is just hard for me to understand.” Well, you have not engaged so far – this is the first set of comments where you’ve actually kind of addressed people who have a beef with your opinion on the subject. Which I do appreciate.
7. “It seems that the only “engagement” that would satisfy you would be to fully accept your position. I am sorry that I am not able to do that.”
Just to clarify: do you disagree with me that coercive treatment is torture?
Report comment
Btw, you mention you don’t want to give specific examples because you’re afraid of possible identification of certain real people. So what if you’re presented with a imaginary narrative? Say a guy calls the police/ambulance on his gf because she has cut herself and told him she will kill herself and refused to get out of her room. She is unarmed though, only crying and “agitated”. She refuses to negotiate with anyone and leave her room but she does not threaten violence against anyone. Would you think this is justifiable to force her out of her room, bring her to the hospital against her will, inject her with sedatives and/or restrain her? She is not cooperating on any of it and is fighting back when physically tackled. What would you do? What do you think, if anything should be done?
Report comment
B,
Re: #1: I see that my answer was not as clear as it could have been. I think this is because I sometimes have trouble finding good language. Let’s say there is someone who is walking for miles in our sub-zero weather in order to meet up with aliens and in the process he has sustained frost bite. This person is found by a concerned person who sees him walking in the road and calls the police who persuade him to come to the ER for evaluation. If this person refuses all offers for safe shelter insisting he is impervious to the cold (despite the evidence otherwise) and tell us the aliens will meet him and will care for him and I was called, I would likely hold him in the hospital against his will. If on the other hand, a different person comes to the ER with frostbite. He has been camping in the area for awhile. He seems to generally know how to mange but on this night things got out of hand, If he says he wants to leave and seems to have some reasonable ability to fend for himself, I might view this as an unusual choice but I would not be likely to intervene.
Re #2: I encourage you to go ahead and fight to change the laws to match your beliefs and values. Re: danger to self, we are much closer together on this. I do agree people have a right to make a choice about whether to live or die. I think it gets complicated when someone presents themselves to mental health professionals because of some act of self -harm but then refuses any offers of help. I just completed Intentional Peer Support and this was discussed nicely there. The idea is to try to understand what it is the person is asking for when the person comes to you with either the self report of having urges to self harm or after having acted in that way. This is an approach developed by someone with lived experience and it is offered as an alternative to coercion. I highly recommend this training. I think it matches nicely with what I have tried to do for years but it also enhanced my perspective and was extremely helpful. http://www.intentionalpeersupport.org/
Re #3: Again , that is your preference and you can try to change the system. I just do not agree. I think we are at an impasse. But where I live, the jails are not going to keep people who are judged to be experiencing psychotic symptoms.
Re #4 and 5: I do not mean to be disrespectful but I think we are at an impasse.
Re #6: One of my earliest blogs http://www.madinamerica.com/2012/05/coercion/
I thought it was important to be honest and transparent about this. There were over 200 comments and I was actively engaged. This has come up on many of my blogs since. Again, you may see it differently, but I consider that engagement.
Re #7: Yes, I disagree.
Re your final post- I think there are many ways to engage with someone in this kind of state. I mentioned Intentional Peer Support. If I were on a crisis team and we were called, I would not refuse to respond but there are many kinds of responses short of breaking down the door and I would try that. Can I absolutely say that under no circumstances would I condone breaking down the door? No. But as I said earlier, I would look for the ambivalence. If she were 100% ambivalent, I would wonder why she told her boyfriend of her intentions. I have known many people who have chosen suicide and the impact on those who are left behind is severe. So I would have some concern for the boyfriend who as also caught in a difficult situation. But perhaps most important, I would keep in mind for the beginning that I do not have the answers. People are complex. I do have a certain notion that many of us are looking to connect and I would try to make a connection.
Report comment
The frostbite example reminded me of Viktor Frankl, Mans Search for Meaning, and the position he found himself in. A Jewish psychiatrist picking the frostbitten toes off inmates in the Concentration Camps. Quite a crossroad to be standing at, the showers or forced labour.
I don’t envy your position at times Sandra, but appreciate your honesty about it.
Report comment
boans,
That is quite an image. One of the things I learned in IPS is that we try to make a connection and we try to understand the other person’s worldview. I guess I am just trying to articulate what it looks like from my position and to share some of the values I have that inform the choices I make.
Report comment
Sandy, this is very poignant, what you say here. Thank you. I think one is thing is our values, and another thing is being empathic to another person’s position. Obviously, there are a lot of people here who are furious about having been coerced, and it has led to trauma, so empathy with your position might be a stretch.
At the same time, you are sincerely and exhaustively exploring how to best empathize with a person whom you do not understand.
The issue of great divide is that you–and others–have a particular authority to make people do something against there will, while those people do not have that same power over you. Most of us balk at whomever gave you that authority (the govt, I guess, since legally you have this option), but still, it is a professional tool that you have at your disposal, and it seems to me that you are saying that there are times when you feel the need to use this tool, and you don’t know any way around it.
From your examples, it seems that your intention is to use this tool of forced hospitalization for ‘the good of the client,’ that is, from a space of compassion. There, I can easily see your values, and I feel them, as well.
So perhaps, it’s an issue of who knows what’s best for others? Perhaps it’s just a philosophical inquiry at this point, because until the law prohibits you from locking people up, you will still have that tool at your disposal, and, as B says, it’s trouble from the get-go. No way this is an equal partner relationship, that’s impossible within those parameters.
I so respect your values, and I can feel your authentic compassion for humanity, but psychologically, how can this be sound?
Report comment
One thing to add…
I do believe you have a good heart and you want to see people recovering and doing well. But personally, I would be on the side fighting to take that one particular privilege away from any mental health care professional, to force anyone to do anything against there will, regardless of circumstances. If that is a job to be done, for the good of society, it should not, in the slightest, belong to mental health care professionals. That is just too much of an oxymoron, and compromises trust significantly. In mental health culture terms–it is UNSAFE.
Report comment
This topic is so central to what I’m working on now, I can’t help but to keep coming back to this, it’s such a vital core issue, this power of forcing someone to take treatment of any kind.
Sandy, I’m ok with whether or not you choose to respond, seriously. I think that’s a free will choice we all have, based on our comfort level. Still, so much occurs to me here, that I feel compelled to express it.
I was wondering, Sandy, if you would continue in your position were that privilege of forcing treatment on someone–for whatever reason–were taken away? I imagine that this would bring up a lot of fear and feelings of vulnerability to mental health clinicians, and I question how many would continue to practice. It takes a lot of faith to sit with high level anxiety without panicking, and reaching for the stun gun.
I realize this might be edgy, but so is this topic. I always appreciate the privilege of exploring our respective truths here, together, to get clarity on these issues which ignite passion for us all. With clarity, change comes with minimal effort.
Report comment
Re: Re: #1: That is a situation where you should be allowed to lie. Tell him/her that you’re taking him to meet the aliens or whatever you have to do but don’t abuse this person by using physical force. There are perfectly good ways in dealing with delusional people which do not need to escalate to aggression. These techniques are also used for people with severe dementia (of course when the caregivers actually care and not just drug these people up to their gills). Besides, what if that person told you that they are going out in the cold because they don’t care if they get frozen because they don’t care about their life anymore? Would that be good enough for coercion? How delusional does one have to be and what standard do you use other than your opinion?
The problem I have is that maybe if you’re really as selective as you say it really does not mean that other people who have the same power are. So maybe you only do it when someone is about to jump of the cliff because he/she sees angels on the other side but I can assure you the bar is much lower than that in general. And what you’re doing to this person is not simply something you can do to 10 people when one of them “needs it” and it will be all OK – you’ll traumatize all the 10 of them.
Re: Re #2: “I think it gets complicated when someone presents themselves to mental health professionals because of some act of self -harm but then refuses any offers of help.”
And what if I asked you for help and then decide that everything you have to offer is not only useless but even more harmful and told you to stop “helping” me and let me do what I want to do? Would you accept that?
“The idea is to try to understand what it is the person is asking for when the person comes to you with either the self report of having urges to self harm or after having acted in that way.”
Asking would be a start. I mean it’s totally OK to offer someone a choice of: if you think you may become a danger to self and you’d like to be prevented by harming yourself by force – tell us under what circumstances and how it can be done (who can do it, what force can be used, can you be given drugs). Using force based on pre-consent is OK. Arbitrary violence is not. The bottomline is: you don’t know what is inside my head and each and every time you’re trying to guess you’re bound to guess wrong in a substantial number of cases. Coercion is traumatising and can push people to really commit suicide (speaking from experience here) and you’ll never be able to tell if that was your fault or the plan from the beginning no matter what the person said before (most people who are “suicidal” don’t really want to kill themselves but it seems like psychiatric treatment may actually tip the scale for some).
” I think it matches nicely with what I have tried to do for years but it also enhanced my perspective and was extremely helpful. http://www.intentionalpeersupport.org/”
It’s all nice and good and I agree with the principles but I will never be able to have a constructive relationship with someone who has a legal authority to torture me and insists of keeping this right. Psychiatric treatment is torture (again: not only me and countless other surviviours but also UN said that) even if you disagree with that. That’s why I keep saying that it’s just like any other torture used for other reasons: it’s counterproductive. Unless one’s aim is to install terror in people – for that it’s extremely useful. If you want to have people cooperate with you you have to have their trust. I can’t trust you if you are allowed to do these things to me, period.
To the hypothetical scenario:
“Can I absolutely say that under no circumstances would I condone breaking down the door? No. But as I said earlier, I would look for the ambivalence. If she were 100% ambivalent, I would wonder why she told her boyfriend of her intentions. I have known many people who have chosen suicide and the impact on those who are left behind is severe. So I would have some concern for the boyfriend who as also caught in a difficult situation. But perhaps most important, I would keep in mind for the beginning that I do not have the answers.”
You admit you don’t have all the answers but yet you would allow yourself to act on this lack of information and potentially cause profound trauma to that girl? You mention that you’re concern for the boyfriend – he’s not your “patient”. You don’t treat people for their family – that is not medicine, that is what many here accuse psychiatry of being – social control. Plus I find this example you gave particularly ironic because this hypothetical scenario is in a way similar to my own experience (that’s why I gave it) and your response would be exactly wrong. You’re in a crisis situation, you don’t know a girl and she won’t talk to you. Yet you care about the guy’s feelings. You may not know but what if he is an abuser? What if he has worked long and hard to get this girl to that point and you’re essentially doing his biding? What if he’s concern and worry are 100% fake? You admit people are complex and you don’t know everything, especially in a situation like that yet you would allow yourself to make a judgement call that may haunt this person for the rest of her life. That is my problem with the whole approach: you don’t know and yet you think you have a right and responsibility to act while you have no idea what you’re really doing. I don’t want you to take that personally – I simply don’t think that anyone, safe maybe for people who are very close to the whole situation, can tell what’s really going on. That is not the problem. The problem is that you think you can solve this crisis by coming in and doing some arbitrary thing.
This is again not to an attack on you but an attempt to show you that you may be committing two main sins of psychiatry: ignorance and arrogance. That is what happens in situations like that: you act on poor information and your subjective opinions and that leads to actions based on you “knowing better”. I’m honestly trying not to be offensive but it’s just how it looks for that girl.
As to this and following points: I think again that you simply lack understanding on these issues. You look at it from your point of view and you don’t seem to be able to step into the other side’s shoes. Which would be all good and fine (I also can’t understand you on this subject, I think that is pretty clear) but you’re the one who is allowed to use force on people whom you clearly don’t understand and that is not OK. I’ve tried to explain how it feels and how you may be making mistakes that you’re not able to see from your perspective and how the other side may perceive the situation and you don’t seem to understand and I don’t really know why. You may guess that it’s kind of frustrating. If the issue is whether drugs are helpful or not or if someone is “mentally ill” or having an existential crisis – these are the things that are important for many but people may at least theoretically reject one or the otehr viewpoint. This is different – this is an issue of state violence and the fact you are not able to understand how much harm it does has real life implications for people like me. I’m not sitting here writing these comments because I have nothing better to do in life – I was so traumatized by coercive psychiatry that this is the one of a few outlets I have, not being able to seek justice for myself or prevent others from being harmed the same way. Your responsibility as a doctor is first to do no harm and I am a living example of that harm. I just wish you tried to imagine yourself on the other side. Can you imagine yourself being beaten? Raped? Locked up somewhere in a scary place, tied up? Helpless? Terrified? I believe you are able to empathize with victims of such crimes – why are you not able to empathize with me? These things are no less horrible when you or any psychiatrist does them then they are when some criminal does it. In a way they may be worse because they are legal and you’re not seen as a victim, you’re seen as someone who deserves it and/or should be grateful for it. It’s insult to injury.
I really don’t want to “attack you” I just genuinely wish you could have some more empathy to people you claim to be wanting to help and I am at loss of how can I make myself more clear. Maybe I can’t but I also can’t stop trying…
Report comment
“People are complex. I do have a certain notion that many of us are looking to connect and I would try to make a connection.”
I am also trying to connect but so far unsuccessfully…
One more thing to ask about your perspective: why do you choose to get involved in coercive psychiatry? Do you think you’d be responsible if you didn’t stop someone from killing him/herself? Not in a a legal but moral way? I simply don’t understand why you want to take this kind of responsibility on yourself…
Report comment
Alex,
Thank you for your thoughtful comments. I do think there are some tricky philosophical questions. But to the question of whether I would practice if I did not have this authority – I would welcome it! This was not something I thought much about when I entered psychiatry. It is not what drew me in. But once in, I certainly realized I needed to reckon with this in a serious way and that is an ongoing project. But if I did not have that authority, I do not think the problem would go away. So what would you propose for the first gentleman I describe above with frostbite?
Report comment
“But to the question of whether I would practice if I did not have this authority – I would welcome it! (…) But if I did not have that authority, I do not think the problem would go away.”
You can practice and not use this authority. You can simply refuse to coerce people ever – there are plenty of psychiatrists who don’t do it for many reasons. It’s not a requirement, it’s an authority you elect to have, not are forced to have it. I agree if you didn’t do it, someone else may but this should never be an excuse for any harmful act – substitute “coerce people to treatment” with “abuse” and I think you see how ridiculous such an argument is. I simply don’t get it – when you don’t want to do it and don’t have to, why do it?
“So what would you propose for the first gentleman I describe above with frostbite?”
Convince him to go with you. Use “white lies” if you need. But don’t use physical force on him.
Report comment
A bit more on a frostbite: you may say “I’ve tried everything in my power to convince him to go to safety and he won’t listen and if he does not he will end up dead or at the very least with severe frostbites”. That is all true but using this logic you should also be able to force diet and exercise on a person who is suffering from type II diabetes and obesity or force people who smoke to quit or force someone who has cancer to undergo treatment. Doctors are not allowed to make these choices for their patients even if these choices are as “unreasonable” and “delusional” as any pursue of aliens. It is completely arbitrary that you see the example person as so delusional that you need to “help him” even against his will and have a legal authority to do so but you don’t have the same authority to stop a guy who’s about to die from diabetes to stop eating cakes and take his meds (I know a person who dies this way and it pained me to see it yet I would never assume I had an authority or responsibility to do more than trying to convince him to change his behaviour). This is all a social construct – what is sane and what not, what is rational choice and freedom and what is craziness and delusion.
Report comment
Thanks for asking, Sandy. The simple straightforward answer is, I’d off to help and try to get that person to see that their actions are hurting them, but if they refuse to listen or take any assistance, in the end, I’d mind my own business. It’s not for me or anyone to say what another person chooses to perceive, as long as they are not harming others—that’s a different matter. But in this instance, it is himself he is harming, and if there is nothing we can do about stopping this voluntarily, then we are powerless to that person’s well, which is humility, a virtue.
I’d like to say a bit more about what is behind my response, here. I’m re-posting that example in two parts, for clarity.
“Let’s say there is someone who is walking for miles in our sub-zero weather in order to meet up with aliens and in the process he has sustained frost bite. This person is found by a concerned person who sees him walking in the road and calls the police who persuade him to come to the ER for evaluation. If this person refuses all offers for safe shelter insisting he is impervious to the cold (despite the evidence otherwise) and tell us the aliens will meet him and will care for him and I was called, I would likely hold him in the hospital against his will.”
First of all, you are assuming there are no aliens. Perhaps there are, you never know. Just because you don’t believe in them or you haven’t experienced alien energy, doesn’t mean that it is not a reality. Many, many, many—thousands—of people have reported affirming alien experiences. Psychiatrists need to stop “assuming” this is a delusion. Research this on the internet please. Lots of info, of all sorts, from a variety of people in various positions in various cultures. This is a cross-cultural phenomenon.
Although really, the fact that he’s going to meet the aliens is not the problem, that’s his business, his reality. The problem is that he is allowing his body to be harmed in the process. If a person calls the police, they are not ‘concerned,’ they are afraid. I think that’s a very important distinction to make, because fear makes us want to control others. If the person were truly ‘concerned,’ they would take them to a hospital themselves.
If he refuses shelter, that’s his prerogative and his business. Anything else is meddling. The fact that he is hurting himself and cannot perceive this can be addressed, you can try to point out to this person that they are putting themselves in harm’s way from their own actions, but in the end that is his business and fate.
In the healing work that I do, it is part of our creed that we are never responsible for other individuals, we are only there to offer loving support if they want it. If not, then their fate is between them and their God, whatever that would mean to anyone.
We are not saviors, just helpers. To me, it seems you are wanting to ‘save’ people. I don’t think that is sound, and in fact, throws society off kilter. We can only save ourselves, and be responsible for ourselves. Even our children are not our children, as Kahlil Gibran says in The Prophet.
“If on the other hand, a different person comes to the ER with frostbite. He has been camping in the area for a while. He seems to generally know how to manage but on this night things got out of hand, If he says he wants to leave and seems to have some reasonable ability to fend for himself, I might view this as an unusual choice but I would not be likely to intervene.”
Sandy, with all due respect, why should you even have an opinion about what another person decides to do? Mental health clinicians have the mental program of ‘evaluation,’ and we really don’t need to go around evaluating other people, how is that helping anyone? This is an inherent problem in the field, that’s institutional arrogance, pure and simple, as far as I’m concerned.
In this scenario, the difference in your description is striking. If I boil it down to what it feels like to me, it seems you are saying, “We have this crazy guy who believes in aliens and then there is this reasonable guy who I can kind of relate to because he’s generally aware of when he gets frostbite. The crazy guy I’d lock up and the other guy I’d let him go.” I’m putting quotation marks even though I’m not quoting you, but this is how your example read to me, very dualistic and stigmatizing. Now that’s just my reality, but it’s how I read the energy of it, and felt it.
“But to the question of whether I would practice if I did not have this authority – I would welcome it! This was not something I thought much about when I entered psychiatry. It is not what drew me in. But once in, I certainly realized I needed to reckon with this in a serious way and that is an ongoing project.”
But you can choose to never take this option, or is that not true? I know you justify it with your examples, but at the same time, many of us are trying to communicate that this is neither sound nor just, and we are asking you to feel this with your empathy. And I’m saying there’s no way healing can occur, here.
So I’m not sure, from what you say, if involuntary patient incarceration is something you can choose, or is it something which you, yourself, are mandated to do by law? If the latter, then you’re being coerced, too. Unless of course, you are of the same opinion as the government. I’m not sure if we’re talking about your values, or what you perceive to be ‘your duty.’ I think that would be important to clarify.
“But if I did not have that authority, I do not think the problem would go away.”
Hmmm, I beg to differ here. I think that your having this authority is directly and specifically a social ill, and I very strongly believe that if it were to be taken away from you and others, things would most definitely improve.
One thing I hated hearing people say—and these were my professional peers–was “I’m a mandated reporter.” There was such a ring of ‘self-importance’ to it. I urge people to never get near nor talk to anyone who calls themselves this. You never know when you’re going to get reported for pissing someone off. Happens all the time, and it puts people through hell.
The mental health system is drunk with power, and this is why. Imo, not sound, not healthy, needs to change, and yes, it would improve things a great deal if there were no such thing as ‘mandated reporter’ or forced anything. I’m certain of it.
Report comment
meant to write “powerless to that person’s WILL,” not ‘well.’
Report comment
I agree with you 100%. I hope maybe you’re making my points clearer than I do myself…
Report comment
It’s a community effort, B, we’re all speaking from our perspectives and yes, I do hope it adds up to the whole elephant this time.
I think many of us would welcome that authority being taken away from clinicians, so at least we’re all in agreement about that. Although some do want psychiatrists to have this power, because they fear their family members.
Shall we take a vote on who would like this power taken away from clinicians vs. those who want this to remain status quo?
Report comment
I’m not sure things like that should be up for a vote. Human rights should not be voted on for a simple reason – the people who are oppressed are usually either lacking a political voice or in a minority, hence lacking a political voice.
Report comment
I didn’t mean to vote as the public to see if this should be so, I was basically wanting a metaphorical show of hands so that we could see where people really stand on this–or at least, so people can get clarity for themselves. I’ve noticed a lot of fence-walkers on this issue, and I think there should be clarity and definition, here. Just for information, not decision-making.
No, no, I would never ask for a public vote to decide on this issue. If one hasn’t been through it, one doesn’t get it. We’ve lost sight of human rights, altogether with this one.
Report comment
“If one hasn’t been through it, one doesn’t get it.”
Sadly.
Reminds me of a curious fact that John McCain is one of the few people in power who has the integrity to condemn torture, even when perpetrated by his own countrymen. He was also a victim of torture himself and I think this is the main reason why he has this stance – he gets it. It’s sad that there are people who can’t understand it until it happens to them. I wish people had more empathy and imagination.
Report comment
B, Alex, and whoever else may still be following this thread,
I am writing to let you know that I have read your comments. I appreciate the time and thought you have put into this most important discussion. I do not want to be dismissive but this will be my last reply.
A concept we are hitting on – who has capacity to make decisions – is complex and I do not think I can do it justice. While I understand the point – at least I think I do – that harm is done to people when they are forced into hospitals or forced to take drugs they do not want – I also think that your experiences do not speak to every experience.
There are several other writers who come to mind. The first is Elyn Saks, an attorney who has also been forced into hospitals. Her best seller, “The Center Can Not Hold” details her experiences. She has also written another book, “Refusing Care” which is a scholarly approach to this topic.
Rachel Aviv wrote an article for the New Yorker, “God Knows Where I Am” 9http://www.newyorker.com/magazine/2011/05/30/god-knows-where-i-am) about a woman who starved to death after she had been released from a psychiatric hospital. When this came out, what I found so fascinating is how people with varied positions all found their world views supported in the story. For me, it described the complexity and uncertainty of these situations, how there is no “right” answer, and how many people suffer. But others saw clear justification for more aggressive interventionist approaches and some saw further justification for never intervening against a person’s will.
I had an important experience in my first few months of psychiatry residency. An older man came into the hospital in extreme distress. His bowel was twisted and the surgeons said he would die by the morning without surgery. They said he would have a full recovery with surgery. The man declined but his children insisted he get the surgery. I was called. I was 27 and a few months into my training. It was the evening and no other senior physicians were available. I met him and he told me he just wanted to take his chances. He thought he would pull through. If I determined he had decision making capacity based on that interview, he would not have had the surgery. Since I was told he would be dead by the morning, I anticipated having to defend this decision to his children and my attendings who would not have the chance to also meet him. Since the surgeons insisted there was no chance of hope and the man told me he thought he would pull through, I said that he did not have capacity because he did not appreciate the risks of the decision he was making. My main objective was to trigger a hearing because I did not want to make that decision on my own. So at 10 pm, a judge was called in and we had a hearing. The judge was an older guy, he talked to the man, and he said the hospital could not do the surgery against the man’s will. I was not unhappy with that outcome. I requested the hearing not because I was intent on a specific outcome but because I did not think I should be making that decision by myself. The man survived. I have carried this story with me. I am glad that I work in a state that has a fairly rigorous standard and process for evaluating forced treatment. I think this is a decision that requires rigorous scrutiny.
All I can say is that I understand that there are subjective fallible decisions involved that have serious consequences – and sadly traumatic consequences – for people. When one has so little trust in psychiatry, I understand why it is scary to think that psychiatrists are given this power in our society.
At the same time, I believe there is a space where some of us – although we may not have common ground in some areas – can work together to make many improvements. I found this in the IPS training I just completed. I find it in the approach of Open Dialogue. I find it in the Hearing Voices movement.
Report comment
Thanks, Sandy, I’ve appreciated this dialogue and your openness a great deal. You are definitely high on my list of courageous people.
Btw, I read The Center Cannot Hold a few years ago, and contacted Elyn Saks. We had a pretty long phone conversation one afternoon, very interesting lady. She’s not only an attorney, she’s a psychiatrist.
One of the things about speaking our truth in order to make change is that, more often than not, I’m aware how this can challenge people’s ego and feelings. That’s a necessary bi-product of waking up. Certainly mine went through the wringer, but that was necessary to heal and creative positive change in my own life. Sure did lead to being able to own my sense of self and spirit truth, and that’s what changed everything for the better.
I have a guilt button that wants to go off, nature of my family culture. I was taught, by example, to enable abuse and oppression in my family (in other words, to shut up and go along with it), and that became a template in my mind, so that if others weren’t abusing me for speaking my truth, I’d do it myself.
That’s not longer the case for me, a core aspect of my healing was to validate my own reality, despite the wishes of punishers, intimidators, and fear-mongers–the enablers. I’ve worked very hard with that, so I don’t self-judge, and trust my truth. As far as I know, I speak it with clarity, authenticity, and integrity. That’s always my intention. I can only hope it leads to the necessary changes we seek.
I think by each of us speaking our truths and following our hearts, we are, indeed, already creating change together. That’s in the bag, as far as I’m concerned.
Report comment
Dr. Steingard,
Thank you for all your time with this discussion.
For me this conclusion does not address the particular concerns that I have.
I understand the complexity of forcing someone’s safety and believe there are times to intervene and that those must be very difficult decisions indeed. I think Elyn Saks (and forgive me as I have not read the books yet – just the Ted talk and some comments) justifies forced medication for first episodes because she believes that her ‘former’ self would agree and want to be given the medication. For her, medication returned her to her former self,’ medication in combination with psychotherapy has worked wonderfully and for so many years without (from the outsider view) the difficulties with metabolic syndrome or cognitive or emotional difficulties.
I don’t think there would be a Mad in America site or discussions like this if medication had that result even for the majority of people. I do wonder (and I guess I better read Elyn’s book) what she says about the people who seem to get worse symptoms after medication has started, or who remain permanently ill on medication.
It is because of the state of the present day science, which has no valid way yet to diagnose people, nor to know who are the people that will benefit from which medication, and which people will recover in the long run, that discussions about forced medication have an ADDITIONAL layer to go through BEFORE deciding whether interventionist approaches are justified.
I know you said that this was your last post on this thread but I do wonder if psychiatric patients and their families are given the same hearing that the man u described who was undergoing surgery was given. I wonder if judges are called when psychiatric families or patients refuse medication and if the family’s opinions of past failure with medications is taken into consideration, or if it is only the psychiatrist’s, who may have just met the person, opinion that is counted. I wonder if people are put on psychiatric medication first as these issues are worked out. Remember the vast number of people will not have you as their psychiatrist but likely someone who would not be aware of any of the literature on this site. I am reminded about the recent blog of Elahe Essemar on this site who, when I asked her what strategies she had in place to prevent future hospitalizations, wrote back that this was her greatest fear. And this fear that her daughter could be forced remains despite the fact that her daughter came OUT OF a catatonic state 2 years after stopping medications. I really do think that the possiblity of creating ‘supersensitivity to psychosis’, and not knowing to whom this will apply , has to make the decision to force these medications different than for other situations.
So for me this discussion has loudly and clearly answered the question of your article which was do we Bring back the Asylum. Although I would no longer personally use the word ‘Asylum’ because of the painful stories this triggered on this site, it seems to me that having some sort of humane “santuary’ where people can be taken to avoid being forcibly started on psychiatric medication which once started, cannot necessarily be easily stopped, is the only way to solve this issue for people who I would argue are the most vulnerable in society . Surely a humane santuary run by the proper people would be better than either the jail or hospital for the people I worry about. If there was a santuary, then more time could be taken to make sure good decisions were made in those severe cases where is seems intervention is required. ( I can’t imagine how good decisions can be made except by chance in overcrowded emergency psych ward in the few hours or days it takes to start these medications) And for people and families like Elyn Saks who have found that they or their loved ones are restored to their former selves with medication , they could write contracts outlining the type of intervention they want. (and in the absence of a contract, again having time to review their past, talked to loved ones etc to see what they would likely want to happen)
It seerms that these kinds of services are being started up with the Mental Health Excellence site and the Beyond Soteria project.
When I read over my posts to so many people on this site, I realize I must sound so repetitive. But it does feel to me that society is not seeing how urgent this issue is, , and how horrific the results can be for some of the severely ill .
Report comment
Sa,
Although the laws vary from state to state, it does require a hearing to give someone drugs against his/her will. the exception is in an emergency situation (and I understand that is a big exception). In VT, it requires tow separate hearings and they tend to be rigorous – much more so than in the other states where I practiced. they typically last a minimum of two hours.
Report comment
I just wanted to add one thing to your points:
The fact that coercive treatment is used in many cases, not only when someone is deemed psychotic. It seems like almost every time you discuss the issue with some who is pro-forced treatment they come up with the “crazy schizophrenic with a knife story” or at least an alien seeing guy about to jump of the cliff. In my experience these people are anyway a tiny minority of all people committed and drugged against their will, not to mention other types of torture. What can make you deemed incapable of recognizing reality and lacking insight whatever that means is so arbitrary that it is basically equal to “because I say so”. This would not be an acceptable legal standard anywhere (forget for a second the fact that pre-crime is also not an acceptable legal standard and very few people get committed for actually being judged to commit a crime).
I had a unique experience of reading my hospital documents and the things I read were nothing short of incredible. They contained obvious lies (basically stated that I refused to take drugs when I in fact asked for them or that I threw myself on the floor or some other nonsense that didn’t happen but was necessary to justify “danger to self and others”) but the most stunning was actually the description of “symptoms”. The psychiatrists took everything I said and twisted it in a way that made it look crazy. It was Rosenhan experiment all over again. If I laughed – it was “inappropriate laughter”. When I got frustrated I was “agitated for no reason”. I was described to be narcissistic because I told them I was in a PhD programme (which was true) and it was interpreted as “you think you’re smarter than everyone else” (I’m not kidding – that’s a direct quote). The things that happen in these places are so insane that the alien lover in the freezing cold appears like the most sane person in the room. I’d not let anyone of these people in charge of throwing away my garbage because I’d be afraid they kill my elderly neighbour in the process of something. I know an actual judge who avoid bringing in “experts” because she is afraid they are going to make the whole situation worse with their bs diagnosis and she will have to commit someone who can get away with a minor conviction and some social worker oversight. This thing is out of control and should be dismantled.
Report comment
“I am glad that I work in a state that has a fairly rigorous standard and process for evaluating forced treatment.”
I think you have much to much trust in the system. Many of us here don’t have that privilege. I personally was shocked to discover, partly on my own skin, partly by observation and accounts of others, just how f***ed up humanity is in general. The overall rule seems to be – whenever you give a group of people power over another group of people they are going to abuse it and they will find new and creative ways on how to do as much harm as cruelly as possible. Maybe not everyone of them but in the end the best way to prevent abuse is to give people as little power over others as possible. It’s not a rule that applies only to psychiatry but, because of it’s, let’s call them “loose”, definitions and criteria it’s where it is so clearly visible.
Thanks Sandra for engaging in this conversation nonetheless. It takes some integrity to be willing to participate in it from your position even if I think you’re dead wrong on the issue. I wish you all the best with the other approaches you’re taking and hope that maybe some day “the truth will set you free”.
Report comment
As I note above, the civil commitment process in VT is rigorous. It was not that way in other states in which I practiced. I do not know what I would be doing at this time if I was still in that setting. I also am well aware that money has an enormous influence and many people who find themselves in a commitment process do not have adequate resources. It is unfair. Perhaps I am wrong to think I try to help by approaching this with as much honesty and integrity as I can. I am vigilant about not overstating what I know (for instance with regard to the prediction of dangerousness or the dangers of delaying the use of drugs). But I am aware that the law is as much about who has resources as it is about what is written in a statute.
Report comment
That’s funny because if you drug someone in the ER and then give them a “hearing” they are either “under the influence” or in withdrawal. I don’t even remember I had a hearing or talked to a lawyer since I was given such amount of benzos I have basically an almost complete anterograde amnesia from a 5 day period. Given the mental effects these drugs have (with such nicieties as angry outbursts, sucidal ideation, emotional lability, cognitive impairment, catatonia, and so on) and a complete ignorance even most psychiatrists not to mention judges have about these effects it’s pretty laughable to pretend that these hearings are in any way useful.
Report comment
“many people who find themselves in a commitment process do not have adequate resources”
I’d start with the problem that it’s quite difficult to think straight while on a massive dose of whatever sedative they throw on you plus some occasional ECT if you’re really unlucky. Not to mention that suing the hospital your in and staff that has power over you may lead to some nasty consequences.
I don’t think you understand what it means to be in such a situation Sandra. I do not advocate that you go and get yourself locked up because I would not wish that on anyone but you seriously have no idea.
Report comment
Just one more addition I just looked up Elyn Sak’s book “Refusing Care” and it seems it was published in 2002, long before Anatomy of an Epidemic was published.
I wonder how she would weigh in on the discussion now forced treatment when treatment results for the long term are so inconclusive. Inded I wonder if she could be encouraged to post a blog about her opinions on this matter!!
Report comment
……I mean forced medication ,,,,,,,,,
Report comment
Although her book was written awhile ago, she remains active as a scholar and an activist. I would not presume to speak for her.
Report comment
I didn’t mean to imply that I wanted you to speak for her – I find it so difficult sometimes to express what I mean in print!
I really do wonder what Elyn Saks would say about these matters , and I also am now thinking that a team of ‘critical lawyers’ could really help out the movement by drafting some kind of a guideline that looks at the concerns you and other people have been discussing here, Then people and families would at least have something to refer to, particularly as laws vary so much from state to state.
Anyway – thanks for listening and responding even after you had decided you needed to end the discussion!!
Report comment
B makes many relevant and unanswerable points–and hence Sandra doesn’t even attempt to answer most of them. It is a logical fallacy to talk about a worst-case scenario (frostbitten homeless) rather than address the reality of involuntary treatment, which is done to perfectly normal people all the time. Of course professionals who make their living off the established system are not interested in changing it. As was said about Watergate: “Follow the money.” Rationalization and pale attempts at ameliorization of an horrific system just serve to support and protect that system.
Report comment