So, thanks to everyone who has read and commented on my stories of reentry into the mental health system. I have now had many nights of very good sleep and my mental health symptoms are back to the baseline. Baseline for me means I only get separated from consensus reality when a significant trauma occurs at the same time I’m having a pretty good sleep deficit. Usually I can manage it myself simply by being aggressive about handling — and increasing — the sleep. This time I was unable to break that cycle and got some more drugs to help.
The other thing I got drugs for is to help with my vestibular disorder. There are some very good research articles that say that 65% of people who have vestibular disorders also have significant mental health-type issues, or as I have been calling them; “meltdowns.”
What happens for me is my energy level is great except when I have to do things that involve motion, or reading, or loud noises, or a lot of heavy thinking. I am alright cooking, farming, walking, and interacting via phone or in person. But reading, or looking at a computer, or driving, or exertion, or too much bicycling just sorta tears me up.
And when I do too much of that I get very fatigued and have to lay down. If I don’t get myself laid down in time, I get too fatigued. Then, when I’m lying there, if I am scared and angry and discouraged and hopeless and frustrated, I feel like I am dying. A “meltdown” is when all this emotional stuff piles on at once; the sadness and desperation and total lack of perspective, and I just lay in a ball in bed and start crying. What I have found is this happens a lot less when I take an antipsychotic.
I did a bit of research. (I mean I asked my friend to do a bit of research, because reading is so hard.) My friend found me a good article on the drug treatment of vestibular disorder, and they mention nausea medications. Well, it turns out a bunch of the nausea medications are weak antipsychotics. So my thought was “hey, why not a strong antipsychotic?”
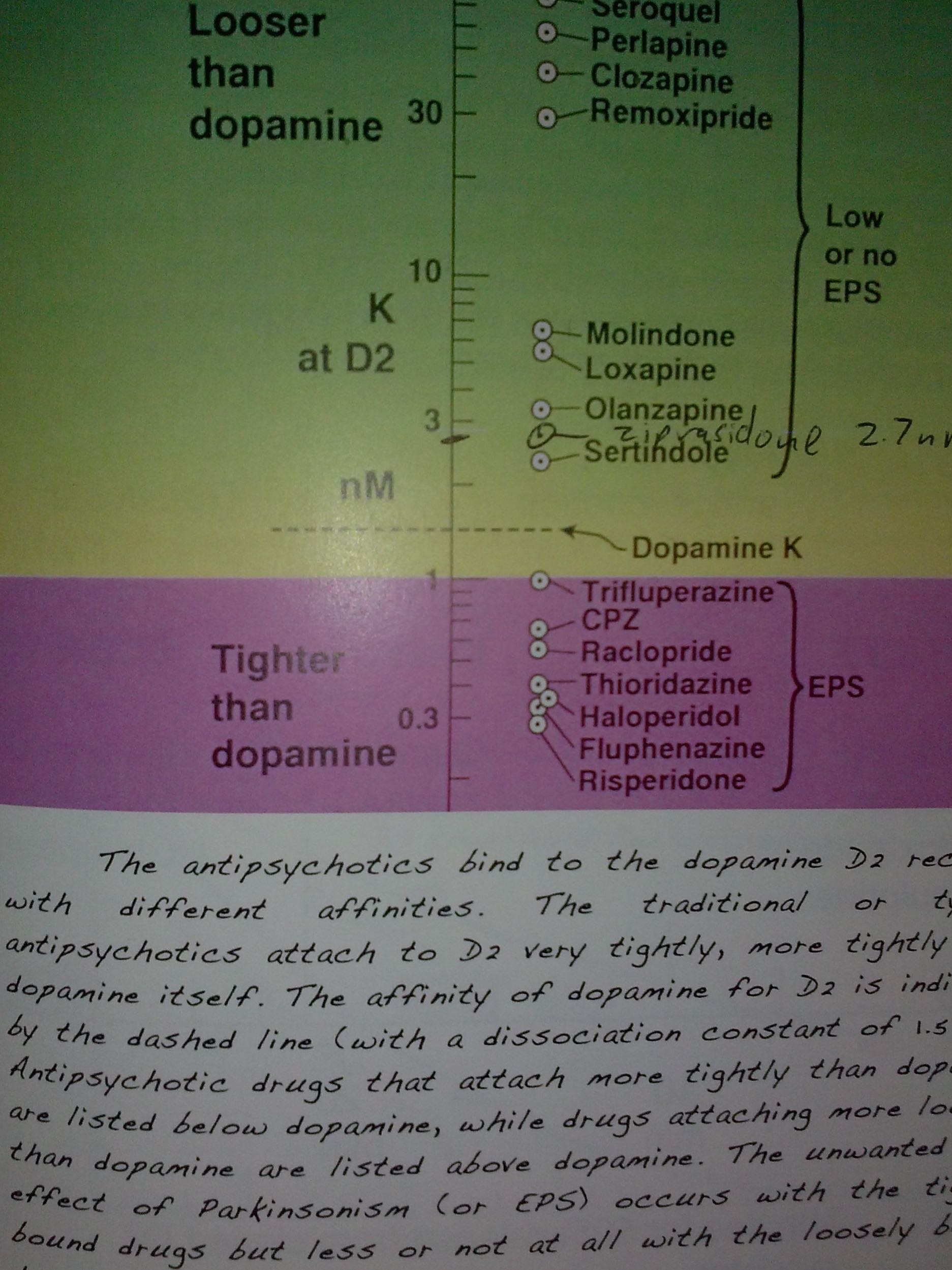 It turns out that antipsychotics can be rated by how tightly they bind to the dopamine receptor. A lot of doctors try to sell more expensive and newer antipsychotics as “atypical.” This means they — theoretically — have lower side-effects. But it turns out the side-effect profile is linked to how tightly they bind to the dopamine receptor, not how new the patent of the drug is. A picture from Dr. Philip Seeman’s book Psychosis: Discovery of the Antipsychotic Receptor1 lists these drugs in order and shows how some of the typical nausea medications are at the top along with some of the older antipsychotics. In the middle is the Geodon that I am using and at the lower end is, in fact, risperidone — one of the so-called atypical antipsychotics. So risperdone is actually worse than Haldol about causing Parkinson’s disease.
It turns out that antipsychotics can be rated by how tightly they bind to the dopamine receptor. A lot of doctors try to sell more expensive and newer antipsychotics as “atypical.” This means they — theoretically — have lower side-effects. But it turns out the side-effect profile is linked to how tightly they bind to the dopamine receptor, not how new the patent of the drug is. A picture from Dr. Philip Seeman’s book Psychosis: Discovery of the Antipsychotic Receptor1 lists these drugs in order and shows how some of the typical nausea medications are at the top along with some of the older antipsychotics. In the middle is the Geodon that I am using and at the lower end is, in fact, risperidone — one of the so-called atypical antipsychotics. So risperdone is actually worse than Haldol about causing Parkinson’s disease.
Or tardive dyskinesia. I don’t know why we’re going to call Parkinson’s disease a different thing if someone has a mental health label and gets Parkinson’s disease – but it’s iatrogenetic. That’s the first concept I wanted to share: that typical vs. atypical is a matter of dissociation from the dopamine receptor, not a matter of patent life. And some of the new drugs really suck. And some of the older drugs are not that bad.
It’s hard to find psychiatrists who actually know this info. I have given a data dump to my current psychiatrist. My appointment is Thursday, we will see what happens.
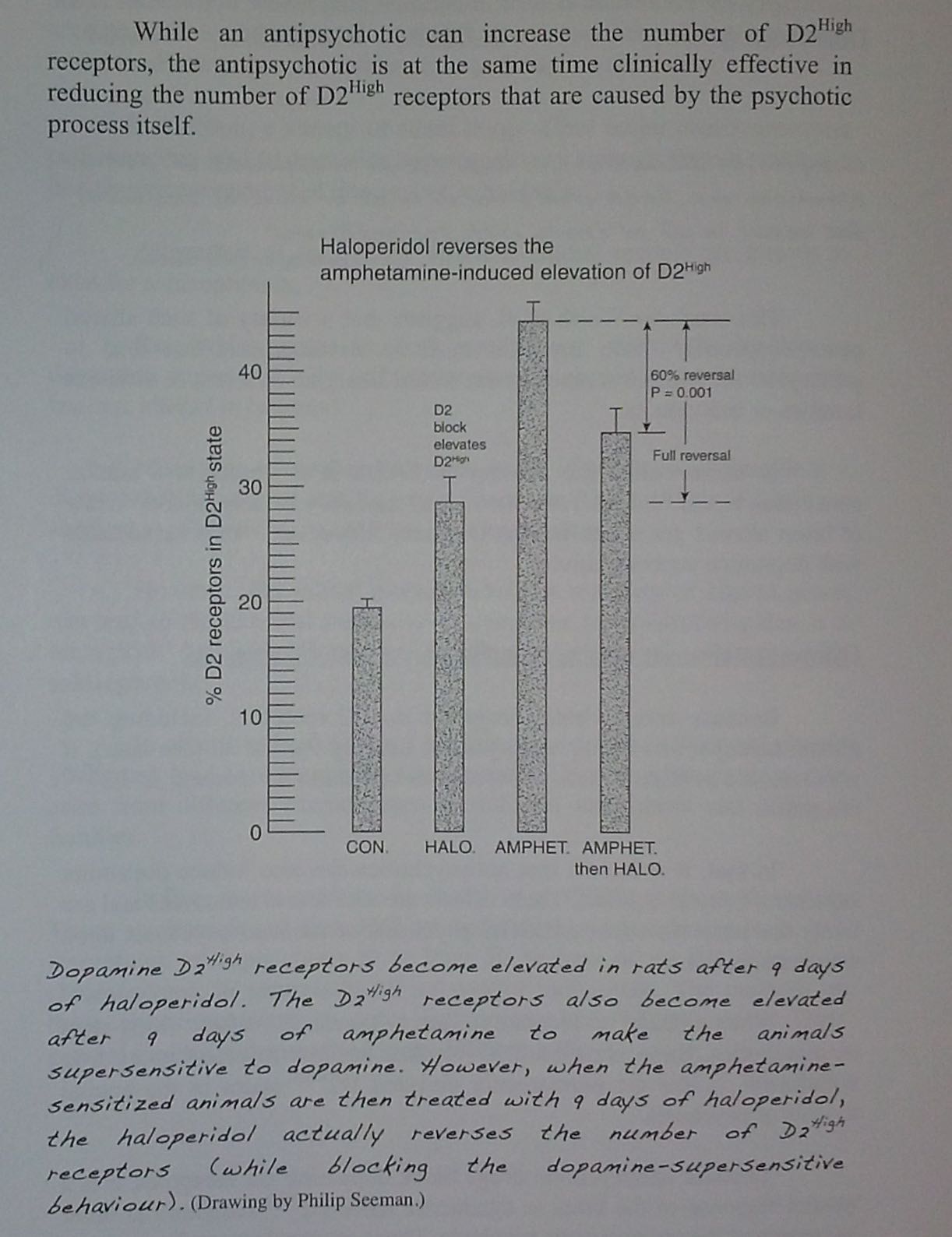 The next thing I wanted to share is how antipsychotics actually cause psychosis. This is best illustrated in a bar graph by Dr. Seeman, with a caption to explain it from his book. The antipsychotics increase the amount of receptors that are in the high-affinity state for dopamine. People who are experiencing disconnection from reality have more receptors in the high affinity state for dopamine. This is a proven research concept with something like 600 academic citations, which means it is just about as much fact as we get in the scientific industry. All of the animal models for psychosis — and there are about 30 of them — have more of these receptors in the high-affinity state.
The next thing I wanted to share is how antipsychotics actually cause psychosis. This is best illustrated in a bar graph by Dr. Seeman, with a caption to explain it from his book. The antipsychotics increase the amount of receptors that are in the high-affinity state for dopamine. People who are experiencing disconnection from reality have more receptors in the high affinity state for dopamine. This is a proven research concept with something like 600 academic citations, which means it is just about as much fact as we get in the scientific industry. All of the animal models for psychosis — and there are about 30 of them — have more of these receptors in the high-affinity state.
Just because there is a biological mechanism doesn’t mean that psychosis is a brain disease. Something causes that mechanism to kick in. In the animal models it can be social isolation,2 or it can be drug use, or it can be certain genes that are screwed up on purpose for lab reasons, or it can be oppression.3,4 Another study showed that rats who have a personality type that stands out from other rats in the degree to which they like to explore and be creative, also have more dopamine receptors in a high-affinity state.5 This, and other studies show that those rats get beat on more than the other rats. This may explain why the dreamers and thinkers and artists and advocates and socially conscious people in our society end up with mental health labels.
But the bar graph, which is the most clear explanation I have ever found of dopamine supersensitivity, shows that while a so-called normal rat has one level of dopamine receptor in the high-affinity state, a so-called psychotic rat has another level of dopamine receptors in the high-affinity state, and that giving an anti-psychotic to the so-called psychotic rat will reduce the amount of receptors that are in the high-affinity state. But it will not reduce that level of receptors back to the so-called normal state.6 The difference shown on the bar graph is the amount of supersensitivity that was increased by the anti psychotic by itself. So; anti-psychotics both cause and relieve psychosis. This is why they need to be used temporarily, because if you want someone to get back to a baseline of zero symptoms, getting off of anti-psychotics will be essential. Since antipsychotics cause psychosis, there is a time factor: you have to sift through and gradually taper and accept the increased level of symptoms that were caused by the drug itself.7
When I re-entered the mental health system, I knew all this and knew that taking an anti-psychotic would increase my risk for psychosis. However, I feel very comfortable managing psychosis. I have psychosis two to three times a year. Ever since I left the mental health system, about two to three times a year my trauma issues and sleep problems build up bad enough that I start having hallucinations. I always know that this is just a signal that I need to get better sleep and do better trauma processing work; through journaling, poetry, nature, talking with friends, and doing some online writing.
But I also knew that antipsychotics for nausea medications are good for vestibular disorder, so I gambled as I re-entered the mental health system. I knew that taking anti-psychotics would give me increased psychosis, but it might relieve my vestibular disorder. Since I know how to manage the psychosis that would occur upon withdrawal, this is a problem I felt OK to handle.
Unfortunately, many people are not educated at all about the fact that anti-psychotics cause psychosis. Instead of people being educated about a gradual taper to help them deal with the rebound psychosis, when they quit taking anti-psychotics and get very, very separated from reality that just “proves” to them that they are ill.
I found, four years ago when I tapered off of 10 continuous years of antipsychotic use, that a very, very hard part was learning how to manage emotions. I felt so much strong emotion at that time that it was hard to build skills to manage. That’s why my taper lasted a whole year. I had been emotionally numb for 10 years, and it had delayed my adult development. I had some catch-up work to do.
But this time I knew that these emotions were fake. From the vestibular meltdown. Because they only came with fatigue, and there were so many emotions all at once, they couldn’t possibly be all the truth.
This is the problem with anti-psychotic taper, and why it’s really important to educate people about these drugs. I actually chose the anti-psychotics because I know this process. The benzos and the SSRIs have a worse withdrawal process because they cause brain injury.
But that is another story. I chose, basically very consciously, to deal with rebound psychosis instead of a drug-induced brain injury to compound the brain injury I already have. This is one of the really nasty aspects of psych meds that people really need to be educated about. These withdrawal processes and all of the struggles that come with them.
* * * * *
References:
- Seeman, Neil & Seeman, Philip; Psychosis: Discovery of the Antipsychotic Receptor. SZ Publications. Toronto, Ontario. March 12, 2009
- King, Madeleine; Seeman, Philip; Marsden, Charles; Fone, Kevin; Increased Dopamine D2High Receptors in Rats Reared in Social Isolation. Synapse. 63:476-483 (2009)
- Seeman, Philip; Weinshenker, David; Quirion, Remi; et al; Dopamine Supersensitivity Correlates with D2High States, Implying Many Paths to Psychosis. Proceedings of the National Academy of Sciences. March 1, 2005. 102(9)3513-3518
- Seeman, Philip; All Roads to Schizophrenia Lead to Dopamine Supersensitivity and Elevated Dopamine D2High Receptors. CNS Neuroscience and Therapeutics. 17(2011) 118-132
- Alttoa, Aet; Seeman, Philip; Koiv, Kadri; Eller, Marika; Jarro, Jaanus; Rats With Persistenly High Exploratory Activity have Both Higher Extracellular Dopamine Levels and Higher Proportion of D2High Receptors in the Striatum. Synapse. 63:443-446 (2009)
- Seeman, Philip; Schizophrenia Model of Elevated D2High Receptors: Haloperidol Reverses the Amphetamine-Induced Elevation in Dopamine D2High (Letter to the editor). Schizophrenia Research. 109(2009)191-192
- Kanpur, Shitij and Seeman, Philip; Does Fast Dissociation From the Dopamine D2 Receptor Explain the Action of Atypical Antipsychotics?: A New Hypothesis. American Journal of Psychiatry. 2001; 158:360-369















Thanks, as always, Corinna, for your observations about first and second generation antipsychotics. I’m zeroing in on the taper you did four years ago. There appears to be no ‘consensus reality’ when it comes to tapering and I find this lack of good information troublesome for anyone wishing to get off these drugs. You assumed that your taper was prudent and therefore slow, and that’s why it took you a year to come off the antipsychotic(s) you had been taking for ten years. My son’s psychiatrist’s rule of thumb (admittedly, this was a few years ago when she told us this) was that for every three years someone has been on an antipsychotic, it takes a year to taper off. So, by her rule of thumb, your taper should have taken over three years, not one. Would a slower taper have helped diminish the withdrawal symptoms? There’s just no consensus reality around tapering, and that’s a problem. It would help people psychologically as to their expectations, I believe, if more agreed upon information was available. Not just about the length of the taper, but how to handle the inevitable post drug symptoms that arise.
Report comment
Hi Corinne,
Thanks for this, very clear and informative.
I know very little about this class of drugs but it’s significant the amount of overlap there is with SSRI withdrawal.
Regarding your comment that SSRIs cause brain injury, what is this induced by and how can it be addressed?
I am planning to discontinue citalopram after 7 years of use and I’ve been on one SSRI/SSNRI or another for 16 years now.
I’m extremely concerned about my memory, cognitive difficulties and emotional numbness that may be related to this long term drug use.
Is there hopeful literature or studies compiled on the withdrawal and repair process?
I’m hoping there is. Were you referring to any study/research in particular when you referenced SSRI induced brain injury and if so could you refer me to them.
Thank you!
Report comment
send me an email using the author contact form. I have a bunch of stuff on Google Drive and I can attach those to an email pretty easy
Report comment
Thanks Corinna,
Have looked for contact but can’t locate one.
Report comment
email corinnawest816 at gmail dot com
Report comment
Hi Corinna,
I’m happy to see you in one piece. Thank you for the necessary Article. You explain the situation brilliantly.
I believe most so called “schizophrenics” are people trapped in withdrawal syndrome. When I tried to withdraw from strong “antipsychotic” medication abrubtly, I rebounded fairly quickly and was given a chronic diagnosis.
Eventually I decided to come off the disabling medications first, and taper very slowly from there with weaker medications. Once I was off the most offensive drugs, I allowed myself as much time as I wanted.
I’m not completely sure I understand the mechanics of the dopamine system* – but I have first hand experience of “antipsychotic” withdrawal syndrome and the emotional ‘dysregulation’ you describe.
I found ‘CBT’ and independent community groups helpful as well.
*(I have a vague memory of a study in Western Ireland in 1978 approx involving rats and depot antipsychotic modecate – the drug I rebounded with).
Report comment
Absolutely brilliant. This, especially, I feel is vital information, from the get go:
“Just because there is a biological mechanism doesn’t mean that psychosis is a brain disease. Something causes that mechanism to kick in.”
You are doing the most relevant and authentic research that brings truth and will benefit so many.
Report comment
Hi Alex,
It’s been said for a long time that “antipsychotic” withdrawal causes a type of PTSD syndrome. It’s probably different for different people – but it’s worthwhile knowing about!
I think people aren’t the same as rats – they are more developed and have more authority over their behavior.
It is also possible to compensate for withdrawal syndrome.
Report comment
Interesting, Fiachra, I’d agree with that from my own experience. Although I don’t feel post traumatic stress is a disorder that we’re stuck with forever, I think of it more as guidance to what feels better to us. For me, that is how I heal pts, I look for what feels good to me, rather than that which gives me anxiety and fear. If I have a pts reaction to anything, then it’s not a good fit for me; and if I go in the other direction, I find my gold.
Because of the pts from the medication toxicity, which makes me fear putting any chemicals like that in my body, I no longer take any chemical pharmaceutical or over-the-counter drugs, only natural remedies, which has been really healthful and beneficial for me in every way, so the post traumatic stress from the medication toxicity actually led me in the right direction for myself, and created positive core changes for me.
But that’s just me. I not only respect anyone for how they choose to self-care, I feel people make the appropriate decisions for themselves simply from the virtue of it being their choice. I think everyone experiments with self-care, there are no universal remedies.
What I appreciate here is the self-awareness and trust in her process displayed and exemplified by Corinna. This is pioneering stuff she’s sharing.
Report comment
Hi Alex,
I think “Anti psychotic” withdrawal is probably one of the most important areas of research as regards Recovery – and the article is very easy to understand.
Report comment
I saw the chart on dopamine affinity but was also thinking how lumping all these drugs and discussing anti psychotics together doesn’t seem to be exactly the right way to go about it.
I have taken Seroquel and Zyprexa in the past.
Zyprexa olanzapine is evil, people who write about its effects and withdrawals are always using the word “hell” and others like it. That stuff was a nightmare, its anhedoinia effect a robbery and withdrawal was a trip to hell.
Seroquel is more like pot without the paranoia and anxiety, I took a Seroquel , I am hungry , I need to eat and goto sleep now… You just don’t see the real angry posts online full of words like hell and evil used to describe it.
I guess what I am trying to point out is this scientific stuff and that general term anti psychotic doesn’t describe much the huge difference in the way these completely different drugs actually make you feel. Its not like beer vs wine vs liquor or even apples and oranges.
Report comment
All neuroleptic drugs work on dopamine receptors in “anti-psychotic” doses. But its not only dopamine, these drugs also play with other receptors with varying affinities. For instance, a low dose of Seroquel may give you munchies because of its strong antihistamine H1 effects at that dose. That sedating effect of the drug may also enable more sleep for those people who have not slept properly in a long time. Actually getting some sleep may help with many people who are diagnosed with psychosis. Etc.
Report comment
Does Seroquel have anti neurological compounds added to it that block extrapyramidal effects?
Report comment
Take to much and the result is restless legs.
Less is more with Seroquel.
Report comment
Fiachra: “Does Seroquel have anti neurological compounds added to it that block extrapyramidal effects?”
Technically they don’t usually add different compounds to these drugs. The drugs are made of molecules and they have different effects because their molecules “prefer” to bind to different receptors. When there are lots of haloperidol molecules in one’s body, they often tend to go block dopamine receptors and comparatively not so much other receptors. The molecules of other neuroleptic drugs, such as Seroquel, tend to go less likely to block dopamine and often go to other receptors instead. A single Seroquel molecule can go to dopamine, histamine, noradrenaline, serotonin, etc, receptor.
Major reason some of these drugs have less EPS is that they block dopamine more weakly, even at the doses they are used to treat psychosis. So, a dose of 600-800 mg of Seroquel is still likely to give you less dopamine blocking than moderate or high dose of haloperidol. In addition, I think for instance Seroquel (or, quetiapine molecule’s metabolite norquetiapine) binds to anticholinergic M1 receptors, which may prevent or mask some EPS.
Report comment
Thanks Hermes, that’s interesting.
Report comment
Ya nothing like a few days of cant sleep in a row to open the doors of psychosis.
I will never get why they wake up manic/psychotic patients in the hospital who are finally sleeping. Sleep is what is needed to get it to go away. F U and your clever blood pressure excuse to force wake ups real early in the morning. Those rude wake ups early just prolong it.
Report comment
The top picture (which isn’t very clear, sorry, shows this. The dopamine D2 receptor binding constant for seroquel is about 100nM, whereas the D2 receptor binding constant for olanzepine, or zyprexa is 3 nM. So zyprexa is likely a lot closer to Haldol in feel. I know I ate the house down on both drugs and couldn’t take either.
Report comment
All I know is that Zyprexa seriously effed me up.
This chart shows the half life of Zyprexa as 30 hours and Seroquel 7 hours.
http://www.psychweekly.com/userdocs/articleimages/412CMEtable1_big.jpg
Maybe that explains the anhedonia that insidiously crept in and the hellish withdrawals.
This pharmacology is complicated, we need a chart that simply rates them on the evil scale.
Seroquel is a one or two maybe and Zyprexa an eight or nine. Factoring in the withdrawal hell I think those high numbers would be right for Zyprexa even with the other chemical nightmares such a depot injections included on the rating by evil scale.
I got really really sick from that Olanzepine crap. I have heard peoples ‘nightmare’ stories about kicking heroin and they were nothing compared to my Olanzepine withdrawal.
You kicked heroin and were sick for a whole week. Poor baby.
Report comment
Corinna, thank you so much for sharing this information. For clarity…are you saying that the higher the binding constant, the more difficult, problematic, relapse-ridden the withdrawal? Does it follow that Risperidone would be more difficult to withdraw from than Zyprexa?
Report comment
I am saying tighter the binding constant, the more side effects there are. I think the withdrawal syndrome are more difficult for longer half-life drugs p and I think the difficulties depends on how long you were on the drug. I think the return of emotions that have been gone for a long long time is a lot harder than the rebound psychosis. The rebound psychosis you can ride it out without seeing a doctor. But emotions require a skill building process to learn how to tolerate. They are amazingly intense emotions after you haven’t experienced them for years.
Report comment
Thanks, Corinna, I absolutely agree that all patients and families should be told that withdrawal from the antipsychotics is known to cause a withdrawal induced super sensitivity manic psychosis. Neither my family, nor I were forewarned of this by doctors who weaned me off these deplorable drugs.
I also believe people (including the psychiatric industry) need to be reminded that combining antipsychotics with other psych drugs, like antidepressants or benzos, can also cause psychosis via anticholinergic toxidrome.
https://en.m.wikipedia.org/wiki/Toxidrome
The bar graph is, to me, a bit misleading. It basically seems to be pointing out that if a person becomes psychotic, due to an amphetamine, then an antipsychotic can block some of the extra dopamine receptors, thus reduce the initial iatrogenicly created psychosis. And it shows that an antipsychotic will increase dopamine receptors, above the number in the control, when given alone. Thus, an antipsychotic given alone can cause a psychosis in an otherwise heathy individual.
My first “psychosis” was two weeks after being given my first antipsychotic, so this makes sense to me, although all my doctors claimed the antipsychotics could never cause a psychosis.
What’s misleading, to me, is the claim “the psychotic process itself” causes changes in the dopamine receptors. How can odd thoughts, rather than drugs, cause dopamine receptor anomalies? The message the graph should relay is that antipsychotics should not be given, since alone they can cause psychosis. And amphetamines should not be given to people because, they too, can cause psychosis. And antipsychotics do not cure amphetamine induced chemical imbalances, taking a person off the drug that caused the psychosis is the proper solution.
Thanks for your insights.
Report comment
Hi Someone Else,
You’re right about the “antipsychotics”, they made me a lot worse too. I was happy to refuse them at the start, but once I was taking them I then couldn’t go without them.
I’m not against drugs for the sake of it, but if they worked then people would make solid recovery (and they don’t).
My own chemical treatment was very unsucessful.
Report comment
Someone else, you are right on both counts, both antipsychotics and amphetamines cause psychosis.
But to add some nuance to your “never” statement , the amphetamines are simply one of 30 animal models for so called schizophrenia. Possibly in higher doses that used for adhd? I mean, to provide performance enhancements for higher curiosity kids who get bored in schools and get adhd labels. And the chart shows that antipsychotics relieve a high level of “psychosis” while causing a lower level of it.
Report comment
Stahl, an influential figure in psychopharmacology, tries to draw a line between “conventional” neuroleptics and “atypical” neuroleptics in his book Stahl’s Essential Psychopharmacology. You can read the chapter about conventional neuroleptics here: http://stahlonline.cambridge.org/essential_4th_chapter.jsf?page=chapter5_summary.htm&name=Chapter%205&title=Summary. It details how high D2 blocking in conventional neuroleptics can lead to all these adverse effects. Haloperidol is a strong D2 blocker. Other conventional drugs, such as chlorpromazine or perphenazine, not so much. Instead of telling about the lower D2 blocking ability of these other conventional drugs, he just adds the side effects of these specific drugs to the side effect list of conventional drugs in chapter “Other pharmacologic properties of conventional antipsychotic drugs”. For instance:
“Still other pharmacologic actions are associated with the conventional antipsychotic drugs. These include generally undesired blockade of histamine H1 receptors (Figure 5-9) causing weight gain and drowsiness, as well as blockade of α1-adrenergic receptors causing cardiovascular side effects such as orthostatic hypotension and drowsiness.”
Nowhere he mentions that for instance Seroquel has very strong effect on those same specific receptors, in very low doses. Etc.
Report comment
Interesting path but one often traveled it seems. Pin a base on the mental map as to where the spirit is at peace. Take it all into the imagination. Guide the spirit back here often because it is from this base that the spirit will seek to understand what a crazy world the ego seeks. No drugs required!
Report comment
Corinna, I went cold turkey off both antipsychotics at once. I was on three for a few years along with a few other drugs. I stopped 3mgs of Risperdone and 20 mgs of Abilify. I didn’t know anything about withdrawal. Sometimes I wonder if the withdrawal is made worse by the placebo effect. No, I’m not saying “it’s all in your head,” but if you tell people “it’s gonna suck,” then surely, it’ll suck worse. I had no clue. I got put into an ER on a hold and they were such inattentive they completely forgot to give me my pills. Finally, I was scared I’d have a seizure from stopping the anticonvulsants, so I thought I better speak up and remind them. They gave me a “PRN” of Lamictal. Um, huh? Well, I was out. I decided the heck with the Risperdal and Abilify. I was fine.
However, a long time ago, a very long time ago, when I took an overdose the doc said, “I think you don’t need meds after all,” and he didn’t put me back on. I had racing thoughts from Thorazine withdrawal. But he thought I was “psychotic” and “needed” the drug. Oddly, I wasn’t psychotic, and never was. I never understood why they were so worried about “symptoms coming back” when there were no symptoms to begin with, none that required a “cocktail” of seven pills. Oddly, I knew that all along, in the back of my head.
Report comment
Im on a small dose lexapro and ativsn about a month ago i went to eye hospital due to photophobia caused by the drugs im on.
They give me a drug called tropicamide ophthalmic which i was unaware of at the time was an anti-cholinergic drug. I became very disorientated for a few days and started to experience terror and PTSD symptoms….racing mind every morning and i have these vivid night terrors , and severe OCD symptoms- should this still be happening a month later.
Report comment
I spent six years being “experimented” on by being given every drug possible. Ativan, Depakote, lithium, haldol (found out that I’m allergic to it), trazadone, zyprexa, xanax, seroquel, abilify, risperidone, geodon, klonazapine, and many more. I experienced psychosis, anxiety, thoughts of suicide, depression, eye problems, tremor, weight gain, and more while on these drugs and trying to withdraw. I ended up in the hospital while reducing zyprexa. My experience, like others, was pure hell. Don’t take risperidone either. Depakote made me feel like a robot without emotions. Ativan was toughest to withdraw from. It took me six year to get to where I am. I am the point of just taking one atypical antipsychotic, and I always knew I never needed any drugs. Now I am on Latuda at 20 mg and going to be tapering off slowly as possible. And I am determined that I won’t ever have to do this ever again. I would rather die than ever have to take any mental health drugs. Once I am off Latuda (Lurasidone), I am not looking back.
Report comment