In 2004, the FDA added a black-box warning to SSRI antidepressants on the increased risk of suicide among children taking these drugs. A new study suggests that this warning has increased the proportion of children who begin an antidepressant on a low dose, but the majority are still receiving higher than recommended doses.
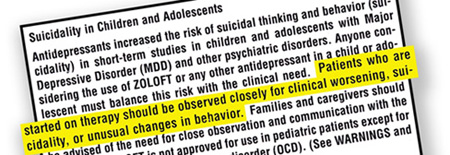
After an FDA funded meta-analysis had found that children taking antidepressants had twice the rate of suicidal ideation and behaviors as those taking a placebo, the FDA advised the children diagnosed with major depressive disorder (MDD) not be given paroxetine (Paxil) and added a warning to all antidepressants. While the initial warning was geared toward children with depression, a year later, in 2005, the FDA expanded the warning to include adolescents and young adults.
Research suggests that, among children and young adults, a higher antidepressant dose is associated with a heightened risk of side-effects, including self-harm, “highlighting the potential importance of initiating therapy with lower doses, especially among children and young adults.”
In 2007, the American Academy of Child and Adolescent Psychiatry (AACAP) issued new guidelines that suggested that children and teenagers with depression begin antidepressant treatments at a low dose. Public health researchers from the University of North Carolina at Chapel Hill, with funding from the NIMH, recently set out to examine whether US prescribers have begun to exert extra caution with SSRIs following the black-box warning and changes to guidelines.
To assess prescriber cautiousness, the researchers looked at data from the LifeLink Health Plan Claims Database, which contains records of diagnoses and prescriptions for US patients on ninety-eight different private health plans. Specifically, they analyzed the SSRI treatment patterns of 51,948 commercially insured children (ages 5-17), 51,653 young adults (ages 18-24), and 395,550 adults as a comparison group (ages 25-64) taking citalopram, fluoxetine, paroxetine, and sertraline between January 2000 and December 2009.
They found that after the addition of the black-box warning the proportion of patients beginning an antidepressant on a low dose increased over time. Before the addition of the warning, 25% of children initiated an SSRI at a low dose. By 2009, the percentage had risen to 40%. However, 60% of children were still beginning an SSRI on a higher than recommended dose.
“The change in prescribing practices surrounding dosing was not universal,” they wrote, “given that by study’s end, the majority of children who initiated SSRIs did not do so with a low dose.”
The researchers also found that 74% of children continued receive refills of the same SSRI after the initial prescription and that approximately 20-25% of children who had initially received a low dose had increased or augmented this dose by the second prescription.
Patients seeing a psychiatrist were slightly more likely to initiate an SSRI at the recommended low dose than those seeing a general practitioner, “which may be a result of differential familiarity with treatment guidelines, the black-box warnings, or SSRIs themselves.” The initial prescription for an SSRI was written by a psychiatrist for only “21% of children, 10% of young adults, and 5% of adults.”
The researchers conclude:
“Given recent findings that the dose of the antidepressant may be associated with an increased risk of self-harm, as well as AACAP guidelines indicating that children and adolescents with depressive disorders should initiate antidepressant treatment with a low dose, our results suggest that prescribing practices surrounding SSRI dosing among children improved following the black-box warnings but still fall short of guidelines.”
*
Bushnell, G. A., Stürmer, T., Swanson, S. A., White, A., Azrael, D., Pate, V., & Miller, M. (2015). Dosing of Selective Serotonin Reuptake Inhibitors Among Children and Adults Before and After the FDA Black-Box Warning. Psychiatric Services. (Abstract)















These toxic drugs, which perform no better than placebo, should not be given to anyone, let alone children. Children on the SSRI’s often experience manic episodes which then get them labeled as bi-polar. How convenient for the drug companies since the kids end up taking nice big drug cocktails. It’s disgusting and yet nothing is done about it.
Report comment
Exactly! Well spoken. Every single word you typed is spot on. 1 million thumbs up!
Report comment
Absolutely 100% correct, Stephen Gilbert.
Liz Sydney
Report comment
What is a reasonable amount of Draino?
Report comment
It’s all very interesting. As a client/consumer/survivor/recipient (whatever we call ourselves this week,) I absolutely can look at my periods of depression and link them to life’s events and my poor response. Sometimes I responded to SSRI’s, sometimes I didn’t. Sometimes I responded to therapy, sometimes I didn’t. Sometimes, I just got over it because there was no other choice but to get on with life. It’s always interesting to me that meds seems go off the chemical imbalance bit, which if it doesn’t exist in relation to mental health concerns, how can the meds that would in fact create a chemical imbalance then correlate to mental health concerns (i.e. the increased suicide rate?) if there is no chemical connection? Not taking away from the idea that no amount of Drano is safe (LOVE that!) but it’s just a curious thing to me.
Report comment
Great comment, and this especially lit up for me:
“I absolutely can look at my periods of depression and link them to life’s events and my poor response.”
Me too. And not just depression, but anything negative happening to me. Somewhere, I began that process, and when I can tag it, I can shift that, and change my experience. Takes a bit of introspection, humility, and ownership.
I can blame, judge, stigmatize, label, and name-call those around me until the cows come home, but that’s not going to shift anything or anyone–that is, no CHANGE will occur, inside or out, without some kind of catastrophe happening to wake people up. From what I understand, that’s how it works. Whereas when we take responsibility for ourselves and our life experience, rather than to project it outward, then we can avoid worse disasters, and start turning that trend around.
When we take responsibility for what life dishes out and do our inner work around that in a self-responsible way, then we find not only the power to move forward, but also to create authentic core change. I just can’t see any other way. Force works in no direction.
Report comment
how can the meds that would in fact create a chemical imbalance then correlate to mental health concerns (i.e. the increased suicide rate?) if there is no chemical connection?
If I get the question you’re asking in other words, if awful feelings aren’t caused by chemical imbalances why do psychiatrically-induced chemical imbalances cause awful feelings?
One answer is that psychiatric drugs don’t “create imbalances” necessarily, they just fuck you up period, like any poison. Again, what is the “right balance” of Drano vs. no Drano?
Report comment
Agreed that they can and do harm. But not period…I think I’m curious about the cause and effect. Drano would, I imagine, lead to multi organ failure…clearly poison. It would not inspire the individual to end their life like these drugs do. Just thinking out loud here. No stock in Prozac 🙂
Report comment
What a terrible, insidious thing that it became normal, and normalized, to drug children. Nothing short of evil. Drugged children can’t learn how to think, or feel, or cope with any of the events of life when they’ve lived years with their brains on drugs. And these pills are a gateway to any other sort of future substance misuse (or even, it’s being suggested, bipolar illness). A moral crime that began with the pharma companies but that many adults are complicit in: Teachers, school administrators, psychologists, psychiatrists, foster caregivers (as we read about frequently now), and let’s not let PARENTS off the hook. Somebody says ‘yes’ to the prescription, buys it, and shoves it at the child day after day. Shame.
There’s my angry diatribe for the day.
Cheers, all.
Liz Sydney
ourviolentchild.wordpress.com
Report comment
I absolutely agree. And I’m one of the many who had the strange effects of an antidepressant / antidepressant discontinuation syndrome symptoms misdiagnosed as “bipolar.” So, absolutely, this is happening. It’s tragic we’re stigmatizing and drugging children, though. Realistically, only the lowest form of life on the planet would attack the weakest members of society. That’s just sick and wrong.
But when you try to educate teachers about the problems, they get defensive because they’re being put into horrible situations. I’ve met parents who think it’s a good thing to give their kids drugs that help them study. I so worry about these children. I know another parent who couldn’t handle her rambunctious child, so drugs her. I tried to educate her, and she says hopes to get her kid off the drugs some day, but the drugs do apparently calm some children down, but at what long run cost? You have lunch with a pastor, who heads up the largest child drugging organization in your town, give him Whitaker’s book. And this is his bread and butter, so he doesn’t want to see it end. It’s just heartbreaking.
Report comment
I think children under 21 shouldn’t be prescribed any antidepressants; we shouldn’t be in a hurry with drugs!! There will be a lot of difficult situations in life, and if they become accustomed to drugs in so early age what will be next? Moreover, there are a lot of ways to treat depression except antidepressants: http://bit.ly/21IqeXJ
Report comment
The life threatening toxicities of SSRI’s share the basic common denominator of AKATHISIA. This is apparently poorly understood by prescribers, Tragically, AKATHISIA is vulnerable to mis-diagnosis as a first episode psychosis. This is “managed” with further SSRI /s and “anti-psychotic/s, increasing the serotonin toxicity and causing extra-pyramidal and other brain, as well as systemic injury.
The truly bizarre and unique behavioural, personalty and physical changes should make a clinical diagnosis relatively straightforward.
A prescription drug history: —-> introduction of SSRI, change in dose of, change of SSRI, or cessation of SSRI, resulting very rapidly in “pseudo-psychotic” behaviour and extreme, overwhelming AGITATION will provide the basis of a safer and more effective approach to this vital differential diagnosis.
Report comment
TRM123
Akathesia misdiagnosis:
‘Pre psychotic episode’ was how my Adverse Reaction and last hospitalization was described (many years ago in Ireland). After that I cut the meds right down and got better.
2 years later my Consultant Psychiatrist was praising my recovery and wanted to know how it had come about. So I told him the truth, that it was as a result of stopping the disabling medication that had also triggered my suicidal hospitalizations.
The next time I saw my Psychiatrist he told me he was going to Canada on a Sabbatical. He went to Ontario
http://www.ncbi.nlm.nih.gov/pubmed/3406048
Report comment
Cool, you got one to quit (or at least take a break from) disabling people, excellent job, Fiachra.
Report comment
Thanks Someone Else,
It might have been coincidence.
Years later I complained about my *experience to the Irish Medical Council and they provided me with details of my former Psychiatrists juniors, who were no longer registered. So I presumed my former psychiatrist to be retired (he wasn’t though, he was on an Irish Medical Council Committee).
Eventually I discovered he was still registered, and I chased up a complaint.
Irish Medical Council Staff were prepared to admit they knew my former Psychiatrist personally, but they claimed they didn’t recognise his name (he’s got 4 first names and a shortened version as well).
My complaint went nowhere. He was let off the hook by his colleagues. But I believe he is now actually genuinely ‘retired’.
*Manufacturers’ Warnings In Clinical States: Severe adverse reactions requiring immediate medical attention may occur and are difficult to predict. Therefore, the evaluation of tolerance and response, and establishment of adequate maintenance therapy, require careful stabilization of each patient under continuous, close medical observation and supervision.
http://ps.psychiatryonline.org/doi/abs/10.1176/ps.49.10.1361-b#/doi/abs/10.1176/ps.49.10.1361-b
(Extra pyramidal equals akathisia)
Report comment
Thank you for your response to Akathisia Misdiagnosis Fiachra
Re Extra pyramidal equals akathisia, — agreed.
I should have specifically referred to the grotesque features of iatrogenic tardive dyskinesia which may rapidly follow the failure to recognise, diagnose and adequately manage acute SSRI induced Akathisia.
Psychiatry means “never having to say you’re sorry”.
Report comment
Yep!
Report comment
Hooray, Fiachra! Simple, direct truth-speaking in action. We want more of that 🙂
Report comment
Thanks Alex.
Report comment