A new study investigating fifteen years of patient records at a Midwestern hospital found that psychiatrists almost always responded to patient complaints about their relationships by prescribing antidepressants, despite the fact that these complaints had little to do with the DSM criteria for depression. The study’s lead author, Jonathan Metzl, a professor of Sociology and Medicine, Health and Society at Vanderbilt, suggests that after the decision in 1974 to remove homosexuality from the DSM, psychiatry continued to enforce forms of socially accepted relationships through the prescription of antidepressants.
 “As it became less acceptable to overtly diagnose homosexuality, it became increasingly acceptable to diagnose threats to female-male relationships as conditions that required psychiatric intervention,” Metzl wrote.
“As it became less acceptable to overtly diagnose homosexuality, it became increasingly acceptable to diagnose threats to female-male relationships as conditions that required psychiatric intervention,” Metzl wrote.
“Doctors increasingly responded by prescribing antidepressants when patients came to the office describing problems with heterosexual love and its discontents.”
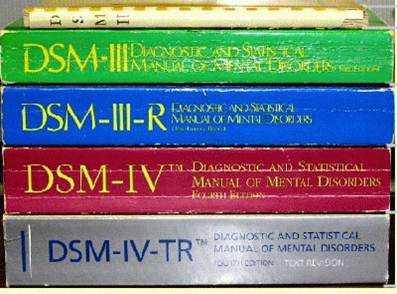
Metzl and his colleagues, Sara McClelland, and Erin Bergner, together representing perspectives from psychiatry, psychology, and sociology, begin their paper by examining “the heterosexualizing of sanity.” While mental health was traditionally associated with normative heterosexual relationships, in the late twentieth century two major trends impacted this history: The removal of homosexuality from the DSM and the rhetoric of gender roles inherent in the marketing of psychiatric drugs.
The researchers ask: “Did the removal of homosexuality from the DSM unintentionally fortify normative assumptions about ‘proper’ gender roles in the interactions between mental symptoms, women, and men?”
“In many ways, the 1974 decision was a major step forward,” Metzl wrote. “But as we show, implicit gender still functioned in the exam room, and our analysis suggests that psychiatry still has work to do in that regard.”
The researchers systematically analyzed and coded patient charts and psychiatric notes of 45 adult patients. These patients were drawn from a much larger sample of nearly 2,500 charts from a 15-year span at a large Midwestern hospital system.
“In the charts we analyzed, the pressures of attaining or maintaining heterosexual relationships functioned as common modes for describing depressive symptoms,” Metzl wrote.
The content analysis revealed that psychiatrists and physicians often decided to include the details of a patient’s heterosexual relationships and “the majority of women’s charts identified a patients’ marital status as a matter of course and then qualified this status through reference to a male partner.” Relatively few charts listed women’s work or employment history while employment status was routinely included in the records of male patients.
When patient charts “consistently connected women’s symptoms with unfulfilled relationship or gender roles,” the researchers found, these “formulations frequently led to prescriptions for SSRI antidepressants.”
“Our analysis suggests that outpatient psychiatric charts from the year 2000 linked concerns about depressive illness to seemingly extra-clinical tensions regarding heteronormativity and its discontents,” the study authors conclude.
“In an aggregate sense, evolving connections between the heteronormal and the psychiatric normal suggest the possibility that the rhetoric of psychiatry and psychopharmacology performed some of the same regulatory functions as once did the DSM, coding particular gender performances, races, or object choices as mentally healthy while relegating others to the realm of disease.”
****
Metzl, J.M., McClelland, S.I. and Bergner, E., 2016. Conflations of Marital Status and Sanity: Implicit Heterosexist Bias in Psychiatric Diagnosis in Physician-Dictated Charts at a Midwestern Medical Center. The Yale journal of biology and medicine, 89(2), p.247. (Abstract)















after the decision in 1974 to remove homosexuality from the DSM, psychiatry continued to enforce socially accepted forms of relationships through the prescription of antidepressants.
This perfectly shows that psychiatry is all about social control and has nothing to do with science.
Report comment
Hocus Pocus Diagnosis where the focus is on the label, and Not on the facts of the individual’s experiential life, the hypnotizing, mesmerizing effect, objectifying the person to be controlled and managed by harmful synthetic chemicals, pharmaceuticals and ECT, electric current through the brain, with No Cumlative Healing Effect, making them instruments, tools of torture, used by pontificating psychiatrists provided by pharmaceutical companies for their pockets at the expense of suffering individuals. Allopathic medicine is eugenics. Then, medical records are documentation for the day of reckoning when correctly understood. The Nazi Doctors – Medical Killing and the Psychology of Genocide by Robert Jay Lifton Operation PaperClip brought Nazis to the US after WWII. Project MK ULTRA Mind Control Techniques CIA Program youtube.com A documentary about the CIA and Psychiatry. Pharmacy < Pharmakeia < Sorcery, Drugs, Enchantment. That Old Black Magic , literally.
Report comment
Hocus Pocus Diagnosis
Precisely!
Psychiatrists aren’t called “shrinks” for nothing.
They shrink the world view to fit their very narrow definition of what it means to be human by diagnosing anything THEY (collectively) decide is not “desirable” even if it is within the gamut of being fully human. All they have to do is vote it into the DSM.
…and once the behaviour/belief/not “normal” cluster of traits is in the DSM it can be medicated, by force, and the person to whom the diagnosis has been stuck can do absolutely nothing about it.
They can be locked up, shackled, injected, have severe and life threatening seizures induced via ECT administered by “doctors”, and denied every human right imaginable just because psychiatrists want to increase their own power, position and earnings.
None of the treatments have been shown to be either efficacious or safe.
None of the “diseases” have been shown to exist.
Being female and “misbehaving” or complaining of not being totally fulfilled (ie not being happy with limited opportunities, abuse, or subservience or not being horny on demand regardless of partner’s behaviour) almost guarantees being questioned on your sexuality and diagnosed and heavily medicated.
Psychiatry is purely about social control and enforcing their view of what is “normal” pretty much on the basis of what can earn them and/or big pharma money and what delivers maximum power and control into their hands.
The control is applied to race, gender, behaviour, thoughts, actions…or anything else they see fit, or unfit.
Report comment
This seems to explain why 25% of middle aged women are currently on antidepressants – any woman not 100% satisfied with their marital relationship gets prescribed an antidepressant – which, of course, is absurd. It is also sexist that men’s professions are listed, but women’s are not. Especially since neglecting to list the women’s professions leads doctors to falsely proclaim productive citizens are “unemployed,” thus worthy of attempting to murder with psych drugs. Definitely, our country is moving in the wrong direction. Thanks, of course in part, to the psychiatric industry.
Report comment
You know if they named drugs by their most common effect SSRIs might be named Sexual Activity Desire Removers.
Doctor: I see you are having problems with your love life let me prescribe you some SSRIs … Sexual Activity Desire Removers.
I think SSRIs helped the increase the divorce rate cause sex is part of the glue that holds couples together and SSRIs screw it up for many people.
Report comment
This is doubly idiotic! First off, they are identifying RELATIONSHIP problems and then prescribing a PHYSIOLOGICAL intervention to “help” – do they really think that taking a drug will improve your relationships? Second, they ignore the obvious fact that having a challenging relationship situation would LEAD to depressed or anxious feelings NATURALLY. This totally belies their claim that they only treat “endogenous depression” or “clinical depression” with drugs – they’ve got a hammer, so everything that comes their way is a nail.
This is not even mentioning the sexist assumptions under which these “diagnoses” and “treatment” plans are made.
The message is clear: if you have relationship problems of any sort, or even if you aren’t in a relationship, stay away from psychiatrists. Or perhaps more generally: if you’re alive and human, stay away from psychiatrists. “Quackery” doesn’t even begin to describe the venal stupidity behind this kind of “treatment.” These people are either evil or dumb, or probably both.
—- Steve
Report comment
Steve,
Several years ago, I worked with someone who was the victim of domestic violence. She was diagnosed as having bipolar disorder. (: but hadn’t filled the med prescriptions.
I successfully discouraged her from filling the prescriptions but to be honest, I don’t know if she remained drug free or not.
I know I sound like a broken record but it isn’t just psychiatrists who are prescribing psych meds for relationship issues. Many people end up on AD withdrawal boards because that PCP in which they described these issues to ends up giving then an SSRI.
So while your advice to stay away from psychiatrists is excellent, you also need to add be wary of drug happy PCPs.
Report comment
True enough – PCPs are actually doing the lion’s share of prescribing of both “antidepressants” and stimulants for “ADHD.” (I decided it’s time to start putting quotes around “antidepressants” to indicate “so-called antidepressants,” since it’s becoming clear that they are at best active placebos for most and something much more sinister for some.)
When I did a brief and painful stint doing involuntary hospitalization evaluations in Vancouver, WA, I discovered an inordinate number of women with obvious trauma histories diagnosed as “bipolar” because they had “mood swings” that were very obviously related to their history of (or ongoing current) traumatization. It really opened my eyes completely to how easy it is to blame the victim for having the “wrong reaction” to their traumatic experiences, or worse yet, to simply ignore that such trauma exist or have an impact on someone’s “mental health.” That was part of my impetus to get out of the field and get into advocacy – I couldn’t support a system who wanted to drug a person’s trauma history out of view. It really is quite revolting, but it’s sadly very common.
— Steve
Report comment