A new study, published in Frontiers in Psychiatry, discusses an ongoing controversy in Australia following an FDA black box warning cautioning that the use of antidepressants may cause an increase in suicidal thoughts and behaviors in persons under 18 years with a diagnosis of depression or other disorders. The study authors also review data on antidepressant prescription and suicide and self-harm trends to assess whether different perspectives on the safety of these drugs are supported by real-world evidence.
The article suggests that prominent researchers and psychiatrists have systematically put forth a narrative that antidepressants are safe and reduce the risk of suicide in youth with no supporting evidence to back these claims while neglecting compelling evidence that the opposite may be true.
The researchers, led by Martin Whitely, a mental health patient’s rights advocate and researcher at Curtin University in Australia, explain that major psychiatric institutions have mostly declined to acknowledge this issue:
“Several prominent Australian mental health advocacy organizations and influential Australian psychiatrists disputed the antidepressant-youth suicidality nexus, and claimed that the use of antidepressants, on balance, reduced the risk of youth suicide.”
 There is increasing evidence showing that taking antidepressants increases the risk of suicidal thoughts and behaviors in persons under 18 years of age. However, professional and public opinion continues to minimize risks and make unsubstantiated claims regarding the drug’s safety profile.
There is increasing evidence showing that taking antidepressants increases the risk of suicidal thoughts and behaviors in persons under 18 years of age. However, professional and public opinion continues to minimize risks and make unsubstantiated claims regarding the drug’s safety profile.
According to the authors, several agencies—both governmental and independent—and individuals have issued reports and public statements that ignored vital evidence supporting the antidepressant-suicidality nexus. Opinion leaders, such as researchers and psychiatrists, have also played a key role in minimizing the risks and insisting that antidepressants reduce suicidality.
“Australia’s peak body on suicide prevention made unreferenced claims, misrepresented the findings of Gould et al.’s review, ignored key findings of the Cochrane review, and minimized the importance of the FDA and TGA suicidality warnings,” the researchers write.
Key opinion leaders in the country—who often received funding from the pharmaceutical industry—have incorrectly quoted research to support claims that antidepressants are safe and reduce suicide risk. The study authors show that the studies used to support such claims were either much more cautious in their conclusions than opinion leaders suggested, or were simply not appropriately quoted.
In one case, due to a discrepancy between the abstract and full-text of the article, “the abstracts did not report the significantly higher rate of suicidal ideation/attempt with fluoxetine compared with placebo.”
Additionally, most antidepressants (90.4%) are prescribed by General Practitioners (GPs) in Australia. The authors suggest that GPs often repeat prescriptions initiated by psychiatrists. A radio interview quoted by the authors showed that some senior GPs might be working with outdated evidence about antidepressants that have long been proved inaccurate. Government bodies have also downplayed the risks of antidepressant use in youth, potentially contributing to a lack of public and consumer awareness.
The study reviewed and analyzed national data on antidepressant use, suicide, and self-harm trends against the backdrop of the debate and controversy around safety and risks associated with this class of drugs.
In Australia, the second-highest per-capita consumer of antidepressants among developed countries, 101,174 persons between the ages of 0 and 18 years were dispensed antidepressants from July 2017 to June 2018. The number of young Australians receiving a prescription for antidepressants decreased significantly after the FDA warning was issued. However, authors suggest that a subsequent increase in antidepressant dispensing and suicide rates supported by the data may have been influenced by advice that directly contradicted the FDA warnings.
In the past 10 to 15 years, there has been a worrying upward trend in both antidepressant prescription and suicide and self-harm rates in youth. “279 Australians aged under 25 died by suicide in 2009, and 458 in 2018,” the authors write.
Between the years of 2006 and 2016, there has been a 98% increase in intentional annual poisonings, with antidepressants prescribed to children and adolescents often being the means of self-harm.
The researchers show that there is a consistent pattern of association between increasing antidepressant dispensing and higher suicide rates:
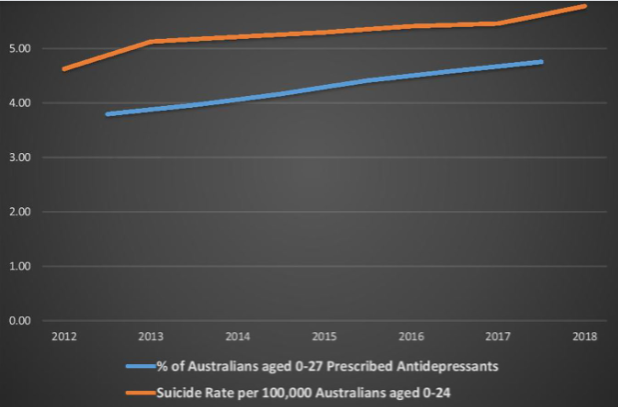 The authors caution readers in the interpretation of the data. Many factors contribute to complex phenomena like suicide and self-harm, and correlation does not mean causation. However, despite the data, key opinion leaders and government agencies continue to play an essential role in shaping the narrative regarding the risk and safety of antidepressants in youth.
The authors caution readers in the interpretation of the data. Many factors contribute to complex phenomena like suicide and self-harm, and correlation does not mean causation. However, despite the data, key opinion leaders and government agencies continue to play an essential role in shaping the narrative regarding the risk and safety of antidepressants in youth.
“Given that Professors McGorry and Hickie continue to be so influential, as evidenced by their prominent role in the post-election suicide roundtable, their continued advocacy of antidepressant use as a means of reducing suicide is significant.”
This study focuses on a neglected area of research: how expert opinion and public discourse may shape prescribing trends and risk awareness. Along with presenting the data on youth suicide and self-harm, the study contextualizes the findings, articulating the forces and powers at stake and showing that scientific evidence can be misinterpreted or only partially presented in public discourse with consequences to public policy and clinical practice.
The authors end on a sobering note:
“There is clear evidence that more young Australians are taking antidepressants, and more young Australians are killing themselves and self-harming, often by intentionally overdosing on the very substances that are supposed to help them.”
****
Whitely, M., Raven, M., & Jureidini, J. (2020). Antidepressant Prescribing and Suicide/Self-Harm by Young Australians: Regulatory Warnings, Contradictory Advice, and Long-Term Trends. Frontiers in Psychiatry, 11, 478 (Link)















Thanks Dr Ana,
I wonder if the GP prescribers know anything about AKATHISIA?
Report comment
I don’t know about akathisia, but I do know that GP’s most likely know squat about dysperceptions, so they don’t ask. They also don’t know about quantitative testing before “diagnosing”, so they wind up giving antidepressants to individuals who, unknown to them,. are showing early signs of the schizophrenia syndrome, the precise group whose individuals are most likely to lose their marbles when medicated with these drugs.
This is also likely to happen to shrinks with the same diagnostic problem difficulties, only they’re better at coming up with excuses than the GP’s.
Report comment
It’s truly shameful that the psychiatrists are still lying about the common adverse effects of the antidepressants, and other psych drugs. It’s appalling that grown adults are systemically force neurotoxic poisoning children en mass. And the death toll is egregious: “8 million people die each year due to mental illness.”
https://www.nimh.nih.gov/about/directors/thomas-insel/blog/2015/mortality-and-mental-disorders.shtml
As pointed out by the same head of NIMH that confessed that all the DSM “mental illnesses” were “invalid.”
https://www.nimh.nih.gov/about/directors/thomas-insel/blog/2013/transforming-diagnosis.shtml
Which, of course, means this is 8 million deaths every year, based upon neurotoxic poisonings, not due to the “invalid” “mental illnesses.” Make our modern day psychiatric holocaust end.
Report comment
You’ll be even more indignant when you realize these shrinks willfully remain ignorant of the basics of nutritional psychiatry, because the practitioner’s mind is closed to anything outside of what he learned in school or company-sponsored seminars.
Report comment
“Antidepressants” increase suicides in people of all ages. This study (which was on a mad in America post) found the drugs increase suicide by 250%. This means “antidepressant” use causes more suicide then depression.
https://www.karger.com/Article/FullText/501215
Report comment
“prominent researchers and psychiatrists have systematically put forth a narrative that antidepressants are safe and reduce the risk of suicide in youth”
Here’s a close look at a classic example: https://www.madinamerica.com/2015/08/do-we-need-to-medicate-more-children-a-response-to-the-call-to-remove-black-box-warnings/
Report comment
Good job Ana, we need to continue bringing these studies under the publics attention.
Patients should sign informed consents in which they are explicitly warned for the dangerous side effects.
The black box warning should be thoroughly explained: “you are sad now, you miss your husband who died, I can prescribe you medication that will blunt your emotions, but there is a risk you will kill your self or your children, or your depression gets worse, or you develop extreme restlessness, delusions, extreme fears, and movements that might not disappear when we discontinue the medication, but if that is what you want to do, please sign here.” How many people would sign up?????
Report comment