In a new study, researchers Jim van Os and Peter Groot found that when trying to discontinue antidepressant use, a process of hyperbolic tapering reduced the likelihood of withdrawal. Withdrawal symptoms were further reduced by slowing down the process and tapering in small daily steps rather than in large decreases every week.
Reached for comment via email, Groot wrote:
“Our research confirms what patients have known and been trying to achieve for decades. That reducing the dose gradually enough and in small steps gives the body enough time to get used to the slowly decreasing dose and prevents complaints due to withdrawal.”
Since a variety of factors can influence antidepressant withdrawal in complex ways, they suggest that the specific, individual process of tapering should be monitored and adjusted in a personalized manner. The authors write:
“The demonstration of multiple demographic, risk, and complex temporal moderators in time series of withdrawal data indicates that antidepressant tapering in clinical practice requires a personalized process of shared decision making over the entire course of the tapering period.”
 Antidepressant withdrawal is common in those trying to get off the drugs and can be severe in up to half of those who experience it. The UK NICE guidelines now acknowledge the potential for severe and long-lasting antidepressant withdrawal. Researchers have proposed that a hyperbolic tapering schedule may help prevent withdrawal or at least reduce the severity of symptoms.
Antidepressant withdrawal is common in those trying to get off the drugs and can be severe in up to half of those who experience it. The UK NICE guidelines now acknowledge the potential for severe and long-lasting antidepressant withdrawal. Researchers have proposed that a hyperbolic tapering schedule may help prevent withdrawal or at least reduce the severity of symptoms.
A hyperbolic taper means that the dose has to become smaller and smaller, particularly near the lowest doses. This is because the drug occupies a large proportion of the brain’s serotonin receptors even at a very low dose (see the dose-occupancy graph below for fluoxetine). As the graph shows, dropping from 40 mg to 20 mg will not make much of a difference in terms of the drug’s effect. However, dropping from 5 mg to 2.5 mg means going from around 65% occupancy to 40% occupancy, a significant shift in the brain’s serotonin system. Going from 2.5 mg to a complete stop is an even sharper drop in serotonin occupancy: dropping from 40% to 0. Thus, as the dose approaches zero, smaller and smaller incremental changes may be necessary to give the brain time to adapt.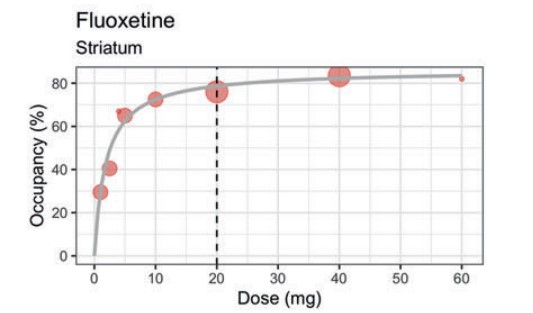
As van Os and Groot explain, “When a psychiatric drug is administered, physiological adaptations occur, and a new homeostatic set-point is established. Abrupt drug discontinuation leads to withdrawal symptoms, with their duration determined by the time needed for the adaptations to resolve. These symptoms may worsen or peak even after the drug is eliminated. Tapering, or step-wise reduction of the drug, causes withdrawal symptoms at each step, but with lesser intensity than abrupt discontinuation as a new, lower homeostatic set-point is established before further dose reductions. Drugs with longer half-lives may lessen withdrawal symptoms by minimizing the difference between the shifting set-point and plasma levels. Also, according to the model, a more gradual step-wise reduction further lowers the risk of withdrawal symptoms.”
Unfortunately, antidepressant pills don’t come in an easily reduced form, which leads patients to try to cut them and break them into small enough doses—which doesn’t lead to very precise dosing. One solution to this issue is tapering strips, which have been used in the Netherlands recently. A patient can order a set of personalized tapering strips from one particular pharmacy in the Netherlands, which contains antidepressant medication packaged in the doses required for hyperbolic tapering.
In previous studies, van Os and Groot found that tapering strips helped users to successfully stop antidepressants by reducing the likelihood and severity of withdrawal. In one study, for example, tapering strips helped 71% of users to successfully discontinue antidepressants, most of whom had unsuccessfully tried to stop using the drugs before.
The new study by van Os and Groot aims to provide a clearer picture of how tapering and withdrawal are linked and what other factors might be involved. The study included 608 participants in the Netherlands who used tapering strips to try to discontinue their use of antidepressants. Most received tapering strips with small daily dose reductions, but 8.6% received strips with larger, weekly decreases. Participants rated their withdrawal symptoms daily. The minimum time of tapering was 28 days (one set of tapering strips), and the maximum was 140 days.
On average, participants noted withdrawal scores between “very little” and “a little,” meaning that tapering seemed generally successful at reducing withdrawal.
Via email, Groot wrote:
“There were quite a few people in our study who reported no complaints at all during their taper. I was surprised about this because I expected more variation in the numbers patients would fill in on the self-monitoring forms that came with the tapering strips.
Today I am not so surprised anymore. This is because five months ago I decided to taper the venlafaxine I have used since 2004 for the second time. I decided to taper from the 75 mg I was using to 0 mg over a period of 20 weeks with the help of five consecutive tapering strips.
When I started, I intended to carefully fill in my self-monitoring forms every day. But I quickly noticed that I found it hard to do this. Day after day, I took my daily dose without really thinking about this, and time and time again, I forgot to fill in my daily number on the self-monitoring form. Because there was no need for me to do this. Whether I filled it on each separate day at the same time or retrospectively after a week or after two weeks really did not matter. Because the number I needed to fill in was always the same, it was always 1 because I had no complaints, which I could in any way attribute to withdrawal.
This five-month tapering from 75 to 0 mg in daily steps was clearly different from my eight-week taper from 150 mg to 0 mg in weekly steps about 10 years ago.
A week from now, I will be at 0 mg, and then things start getting interesting for me. Will I remain stable or not? If I remain stable, I will conclude that perhaps I have been using venlafaxine for almost 20 years for not very good reasons.”
In their study, van Os and Groot found that, on average, those who tapered faster had worse withdrawal. Therefore, the researchers write that guidelines should allow people to craft personalized tapering schedules that can last much longer than 28 days to reduce withdrawal.
Van Os and Groot also note that other risk factors appeared to influence the possibility and severity of withdrawal, including female sex, younger age, previous withdrawal experiences, long-term antidepressant use, and fear of withdrawal. They write that the presence of these risk factors further necessitates a personalized and monitored antidepressant discontinuation process.
They note that the study was observational, so causality cannot be inferred. They add that patients who had already chosen to use tapering strips and who are all in the Netherlands may not be representative of all patients who wish to discontinue using antidepressants.
****
van Os, J., & Groot, P. C. (2023). Outcomes of hyperbolic tapering of antidepressants. Therapeutic Advances in Psychopharmacology. Published online May 9, 2023. https://doi.org/10.1177/20451253231171518 (Link)















If l’m not mistaken, Mark Horowvitz suggests that the same tapering method be used for the withdrawal of Haldol.
Report comment
He does and so do we. That is the reason tapering strips have been developed and are available not only for antidepressants, but also for antipsychotics, benzo’s, opioid pain killers like oxycodon and tramadol, and some other medications like e.g. lithium. See http://www.taperingstrip.com
Report comment
Thank you for this incredibly important research! The world needs to have access to this article. This is a gift to the psychiatric drug withdrawal community. Many thanks to Mr. Groot for the courage to share about his lived experience. That makes him the ideal person to do this research.
Report comment
It is taking me 6 years to taper off 60 mgs of Cymbalta. I have been counting microbeads to taper. I started at 220 beads. I did 5% drops every 2 weeks until I got to 50 beads, then I started to drop one bead every 2 weeks. When I got to 9 beads I started to get withdrawals. I slowed down to dropping one bead a month. It helped reduce the withdrawal symptom I was having but it was still present. At 4 beads I began to hold each bead drop for 4 months. My withdrawal symptom is gone so it seems holding for 4 months is working.
I am terrified of getting PAWS. In 2019 I went off the 60 mgs in 8 months and got severe akathisia 6 weeks after being completely off Cymbalta. I was extraordinarily lucky my brain accepted reinstatement of 30 mgs. It took 3 months to stabilize and I’ve been tapering off the 30 mgs since then.
I’m down to 3 microbeads now, holding each bead drop for 4 months so I should be finished in about a year.
In total it is taking me 6 years to safely taper off 60 mgs and avoid PAWS.
When I was a moderator 2 years ago for a Cymbalta taper group with 30,000 people, I read multiple posts a day and it seemed there was no rhyme or reason to the severity of withdrawals people experienced.
People who had been on the drug for months could get just as severe withdrawals as people who had been on the drug for years.
To note, now 2 years later there are 36,000 people in the group.
Report comment
Its definitely true that a taper has to be hyperbolic. But I think a more realistic time frame is between 5 to 10 years of tapering. I am fortunate that I was taught basic math and science in school, because I can make my own reduced dosage capsules. But here’s the thing you need to understand: Physical withdrawal symptoms are only the tip of the iceberg. The physical withdrawal symptoms give you the advance warning that you are tapering too fast. The physical withdrawal symptoms usually lead to mental symptoms. We humans can tolerate a certain level of withdrawal symptoms. But if we exceed that tolerable level, the taper will fail and we will develop full fledged withdrawal psychosis, necessitating going back on the drugs. We should set a minimum taper rate, and a maximum rate. In most cases, its better to err on the side of taking longer to taper rather than risk a failed taper that could lead to being set back by several years. We just have to guestimate at the proper rate because there is very little science.
Report comment
I need more information about tapering my Haldol. I was on 4MG of it that’s two tablets at 1.5MG and two tablets of 500microgram. So that’s 4 tablets in total. I decided to use a pill cutter to cut one 500microgram tablet into quarters. I threw away one quarter and ate all the other tablets.
My aim is to try to reduce by a quarter every one to two months. I’ve been on Haldol since Feb 2023 and think it will take me a year to come off totally.
Report comment