In a new study in JAMA Psychiatry, researchers found that children born to mothers who used SSRIs during pregnancy had reduced brain volume in multiple areas. Most brain volume reductions were still there at the follow-up when the kids were 15 years old. The researchers write that the affected areas of the brain are theorized to be involved in emotion regulation.
“The results of this cohort study suggest that prenatal SSRI exposure may be associated with altered developmental trajectories of brain regions involved in emotional regulation in offspring,” the researchers write.
The researchers were led by Dogukan Koc at Erasmus University Rotterdam, the Netherlands. This was part of Generation R, a population-based study in Rotterdam. The study included 3,198 mothers with a delivery date between April 1, 2002, and January 31, 2006, and the children were followed with three brain scans over time, the last of which occurred when they were 15.
 To account for factors such as the effect of underlying maternal depression and when, specifically, the mothers used antidepressants, the researchers split the cohort into five groups. There were 41 with SSRI use during pregnancy, 77 who only used SSRIs before pregnancy, 257 who did not use SSRIs but had depressive symptoms during pregnancy, 74 who had depressive symptoms only after giving birth, and 2,749 controls who had neither depressive symptoms nor SSRI use.
To account for factors such as the effect of underlying maternal depression and when, specifically, the mothers used antidepressants, the researchers split the cohort into five groups. There were 41 with SSRI use during pregnancy, 77 who only used SSRIs before pregnancy, 257 who did not use SSRIs but had depressive symptoms during pregnancy, 74 who had depressive symptoms only after giving birth, and 2,749 controls who had neither depressive symptoms nor SSRI use.
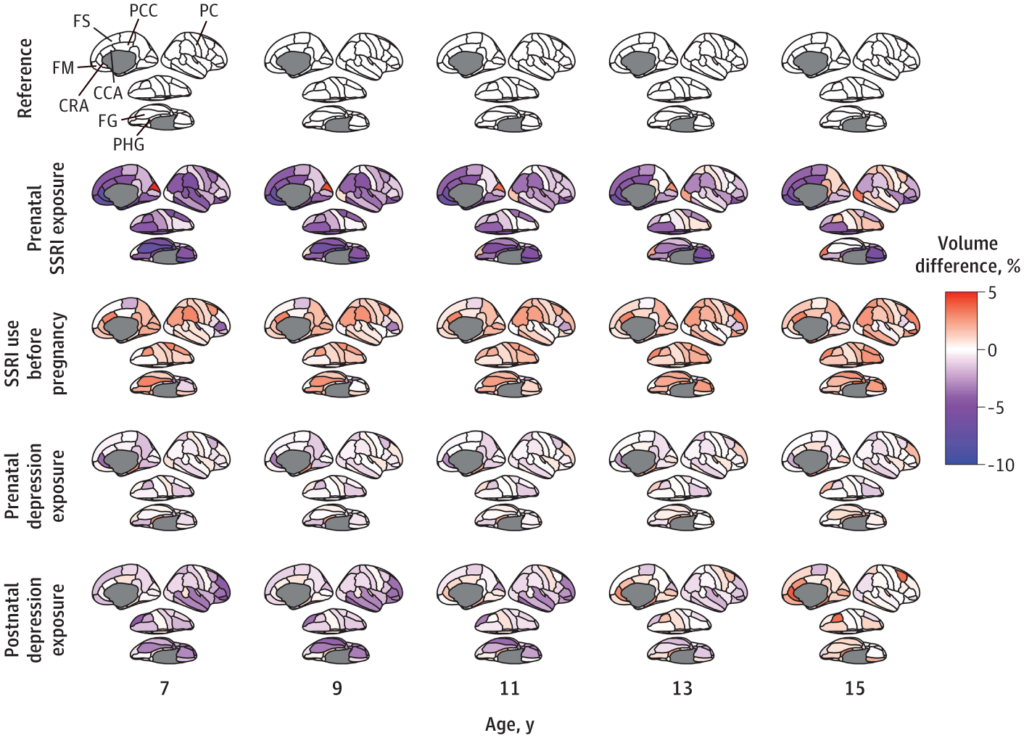
According to the researchers, there was a “persistent association between prenatal SSRI exposure and less cortical volumes across the 10-year follow-up period, including in the superior frontal cortex, medial orbitofrontal cortex, parahippocampal gyrus, rostral anterior cingulate cortex, and posterior cingulate.”
They add, “Prenatal SSRI exposure was consistently associated with lower volume, ranging from 5% to 10% in the frontal, cingulate, and temporal cortex across ages.”
So, could this be explained by the mother’s depression? No, write the researchers. For mothers who were depressed but did not take SSRIs, the children were almost no different from the healthy controls. Prenatal depression was associated with a smaller volume in one area, the rostral anterior cingulate gyrus. Similarly, postnatal depression was associated with a smaller volume in one area, the fusiform gyrus.
Those differences in one area each should be compared to the large, brain-wide reduction in volume in numerous areas experienced by kids whose mothers took SSRIs. Moreover, even in the fusiform gyrus, kids whose mothers took SSRIs had larger reductions in volume than kids whose mothers had depression but didn’t take SSRIs.
The good news is that some of these brain volume reductions appeared to have a catch-up effect: for instance, amygdala volumes had increased by age 15, so kids who were exposed to SSRIs were not any different from controls.
Unfortunately, many of the brain volume differences didn’t catch up. Moreover, it’s unclear what effect these volume differences throughout all of childhood would have on a kid’s development, even if it catches up by their late teenage years.
Previous Research
Studies have consistently found antidepressant use in pregnancy to be associated with myriad risks to neonatal health, including neonatal withdrawal syndrome, preterm birth, congenital disabilities, developmental problems, cardiopulmonary problems, and even death.
In one study, researchers found a sixfold increase in neonatal withdrawal syndrome when mothers took antidepressants. In another study, researchers found that 30% of babies born to mothers who used antidepressants experienced neonatal withdrawal syndrome. None of the babies whose mothers did not use antidepressants had this complication. And yet another study found that over half (56%) of babies exposed to SSRIs had this problem.
Researchers have argued that antidepressants should be discontinued in pregnancy because of this risk, which includes symptoms of hypoglycemia, tremors, hypotonia, hypertonia, tachycardia, rapid breathing, and respiratory distress in babies born to mothers who use antidepressants.
Studies have also accounted for preexisting factors like depression severity by comparing women who continued using antidepressants during pregnancy with women who had the same indication and did use antidepressants initially—but stopped after becoming pregnant. That study found that those who continued to use antidepressants increased the risk of neonatal health complications in their newborns, including preterm birth, low birth weight, and hospitalizations.
Other research has found that antidepressant use during pregnancy alters brain development in the fetus. These findings have appeared in top journals, too: A study in JAMA Psychiatry found that antidepressant use during pregnancy increased the risk of infants with speech disorders, while a study in the American Journal of Psychiatry found that antidepressant use during pregnancy increased the risk of impaired neurological functioning in infants.
****
Koc, D., Tiemeier, H., Stricker, B. H., Muetzel, R. L., Hillegers, M., & El Marroun, H. (2023). Prenatal antidepressant exposure and offspring brain morphologic trajectory. JAMA Psychiatry. Published online August 30, 2023. doi:10.1001/jamapsychiatry.2023.3161 (Link)















What if you find out being pregnant and face a choice: either you stop your SSRI medication which leads to serious withdrawal symptoms (which could continue throughout the preganacy and afterwards, when you have small baby to take care of) or you choose to continue taking medicine to keep your mental health stable – during the time period you are living through a big life changing experience.
Even if you decide to try to have a baby and would start withdrawal early on, it can take longer time than expected. Many women might want to “stop medication after becoming pregnant” but withdrawal might have so serious consequences to their health (and ability to take care of the newborn) that it is not possible.
When prescribing SSRI medication to women – and men in their reproductive years, all these possible consequences should be explained and carefully considered whether the medication is the correct support or not.
Report comment
Not to mention the possible damage to the fetus of continuing SSRIs. There are fairly consistent correlations with birth defects, as well as with “ADHD” behavior later in life, if I remember my research correctly.
Report comment
Well, I think with the usual brain morphometry of MRI or fMRI there is the issue of the difusseness of function allocation in the human brain.
There is a correlation of location with function, but depending on the size of the area imputed a function may or may not correspond to a given function. It varies across ages and between individuals.
The old Broca areas/regions do not always sharply fall in their classicaly described way. They are denominated plastic, but that’s not really explanatory. So the functional relevance, acknowledging its significant anatomical impact, might not correlate that well with a specific tendency, a specific effect.
It might diffuse into maybe related functions, but not everytime the same. The anatomical impact might manifest in different perhaps subtle ways.
Contentious, even prejudicious, but it does point to a stronger need for informed consent even in partners of people who use SSRIs because of the risk of unexpected or unwanted pregnancies.
Grave, but “males” have rights too. It seems to have consequences or risks for planning a life together when pregnancy is not only a choice, but, sad to say, a risk. And what about the kid’s rights? Yikes!.
And it opens to me the speculation of what happens when minors are exposed at the different critical stages of brain developement that end at around 20-25yrs of age, as classicaly described. Aware that the brain keeps developing late into a hopefully long life.
Precisely because of plasticity, the brain areas associated with piano playing, math, multilinguicity or chess grow in masters and probably aficionados!, AFIK. So it keeps developing.
Report comment
There is virtually zero informed consent. How does it possibly make any sense that inutero exposure to powerful psychotropics is safe when pregnant women are told to avoid even coffee or a glass of wine? Women are recklessly coerced and fear-mongered to stay on SSRI in pregnancy.
Personally, I very thoughtfully and intentionally sought a responsible AD taper well ahead of trying to conceive. I had been on an AD for approximately one year at the time. I was told it would be irresponsible of me to not stay on an antidepressant while pregnant, “in case” I developed post partum depression. Mind you, I *never* had any mood issues. I was prescribed an anti-antidepressant solely because I was chronically fatigued.
The provider scared me into compliance, do the “best” for your baby. So, I stayed on AD for both my pregnancies. My first child, I experienced vasa previa which necessitated a six week early planned cesarean section. My second child, was born neutropenic and later diagnosed with autism. There is evidence in the literature that both may be linked to inutero SSRI exposure.
My second pregnancy was a twin pregnancy. The twin succumbed to cystic hygroma in utero.
Additionally, both my children were born highly dysregulated-difficult to soothe, tremors, feeding and sleep problems. This is consistent with a withdrawal syndrome. They continued to experience significant sensory integration issues through childhood.
I fully regret allowing myself to be pressured into something that intuitively felt wrong. I was not at all a high risk, not even a small risk. I was never depressed. My children were iatrogenically injured. The collateral damage to children is absolutely unacceptable.
Report comment
So if a woman finds out she is pregnant, she would need to cold turkey off the SSRI immediately. There wouldn’t be time for a taper. What an awful trap to be caught in.
Report comment
How can anyone assume that SSRIs are safe for infants in utero when alcohol and cigarettes clearly are not?
Report comment