Fixing Genes Won’t Fix Us
From The Boston Globe: Scientists' focus on biology and genetics research downplays the role of socioeconomic factors in causing distress and health problems.
"Science is threatening a new era of...
In Memory of Julie Greene
With deep regret, Mad in America announces another loss in our contributor community. Julie C. Greene, writer and antipsychiatry advocate, lost her battle with kidney disease on November 29 at her home in Beaver Falls, Pennsylvania. Julie had been an MIA blogger since 2014, including several pieces on the dangers of lithium.
Insanity on Trial
The trial of Anders Breivik, who confessed to killing 77 people last summer in Norway, has become a test of the concept of insanity...
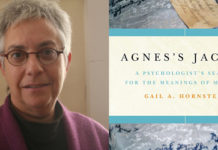
First-Person Accounts of Madness and Global Mental Health: An Interview with Dr. Gail Hornstein
Dr. Gail Hornstein, author of Agnes’s Jacket: A Psychologist’s Search for the Meanings of Madness, discusses the importance of personal narratives and service-user activism in the context of the global mental health movement.
How Come the Word “Antipsychiatry” is so Challenging?
So here we go again; another meeting with another young person who describes how he is in an acute crisis - you may call it - and is diagnosed and prescribed neuroleptics. He is told by the doctor that he suffers from a life-long illness and he will from now on be dependent on his “medication.” As long as people are met this way I see no alternative than showing that there are alternatives. If that means being "antipsychiatry," then I am more than happy to define myself and our work in that way.
Environment is a Primary Factor in Transition to Psychosis
Researchers (including Jim van Os) find, in a three-year cohort study of 1272 people at possible genetic risk of psychosis, that "most transitions (to psychosis)...
Schizophrenia Neurotoxicity Redux
Researchers in Spain and the U.K. find a similar pattern of brain volume changes in a group 76 controls and 109 patients with schizophrenia...
Confessions of a Trespasser
In a recently published commentary in Psychiatric Times, Ronald Pies and Joseph Pierre made this assertion: Only clinicians, with an expertise in assessing the research literature, should be weighing in on the topic of the efficacy of psychiatric drugs. They wrote their commentary shortly after I had published on madinamerica “The Case Against Antipsychotics,” and it was clear they had me in their crosshairs.
Rejecting the “Medications for Schizophrenia” Narrative: A Survivor’s Response to Pies and Whitaker
As a psychiatric survivor who has personally experienced severe psychosis, my criticisms focus on the relative lack of attention to what psychiatric drugs actually are, and on the uncertain, contested nature of the supposed target of these drugs: “schizophrenia.” I will elaborate on each of these points with references, as well as highlighting alternative approaches to helping psychotic people.
Stimulants, But Not Cannabis, Predict Readmission for Psychosis
Prior admissions with stimulant disorder, but not a prior cannabis disorder diagnosis, are a negative prognostic sign in first-episode psychosis according to new research...
The Mind-Expanding Ideas of Andy Clark
In this piece for The New Yorker, Larissa MacFarquhar profiles the philosopher and cognitive scientist Andy Clark, whose work argues that our minds are inseparable...
Hereditary Madness? The Genain Sisters’ Tragic Story
The story of the Genain quadruplets has long been cited as evidence proving something about the supposed hereditary nature of schizophrenia. But who wouldn’t fall apart after surviving a childhood like theirs? The doctors attributed their problems to menstrual difficulties or excessive masturbation — anything except abuse.
NIMH: RAISE Study to Have Immediate Clinical Impact
In a Science Update, the National Institute of Mental Health (NIMH) reports that Medicaid services is already taking steps to implement “coordinated specialty care” (CSC) in response to the RAISE study released last week. “The RAISE initiative has shown that coordinated specialty care for first episode psychosis is better than the standard care offered in community clinics. However, covering the cost of coordinated specialty care can be challenging. When Medicaid agrees to pay for effective treatment programs, patients in need benefit.”
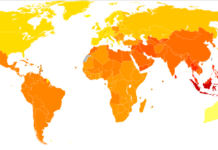
International Study Examines Environmental Factors Associated with Psychosis
Study finds the incidence of “psychosis” to vary by person and place, corresponding to factors such as race, ethnicity, age, and environment.
Remains of Missing 24-Year-Old Dad Found in Coast Guard Boat
From Yahoo! News: Nine months ago, Matt Amsler, a 24-year-old father, mysteriously disappeared after undergoing a bad reaction to antipsychotics. His body has been found...
Markingson Case Supporters: Please Join Our Call-In Campaign
Patient advocates and bioethicists have launched a call-in campaign demanding action on psychiatric research abuse at the University of Minnesota.
American Psychosis
E. Fuller Torrey has a new book. While I was not thrilled to support the Treatment Advocacy Center, I was curious as to what he had to say. Where Torrey has clarity, I contend there is much that we still do not understand. I worry that a perspective that suggests the answers are clear cuts us off from inquiry into alternate approaches.
What is Contributory Injustice in Psychiatry?
An article on contributory injustice describes the clinical and ethical imperative that clinicians listen to service users experiences.
Early Environment Influences Schizophrenia Independent of Genetic Risk
Canadian researchers found that childhood adversity and other environmental factors such as family instability and cannabis use was associated with the development of schizophrenia,...
Existential Therapy Assists Patients Withdrawing From Psychiatric Drugs
Confronting existential anxiety through “Basal Exposure Therapy” shows promising results in people withdrawing from psychotropic drugs.
Psychosis in the General Population
Schizophrenia Bulletin explores "the extended psychosis phenotype," finding that affective dysregulation, psychotic experiences, motivational impairments, and cognitive alterations are distributed throughout the population, and suggestive...
Does DSM-5 Matter? Yes; but not for Psychiatrists
What makes the DSM so pernicious is that it is a cultural document whose influence transcends not only psychiatric practice but also the Western civilization from which it originates. Each revision of the DSM rescripts and reimagines how we make sense of our experiences, reinterprets what thoughts, feelings and behaviors are socially sanctioned, and ultimately what it means to be human.
Relapse in Chronic Schizophrenics following Abrupt Withdrawal of Tranquilizing Medication
Relapse in Chronic Schizophrenics following Abrupt Withdrawal of Tranquilizing Medication. Prien, R. British Journal of Psychiatry, 115 (1968), 679-86.
The critical finding of this NIMH study was that...
More Evidence Antipsychotics Reduce Brain Volume
People diagnosed with schizophrenia experience reductions in brain volume that increase over time, and the amount of those reductions increases in proportion to the...
Mental Health Patient Becomes Best Mental Health Nurse
From ABC Australia: Matthew Ball, a mental health nurse with lived experience of hearing voices, psychiatric diagnosis, and hospitalization, was recently named the Australian College...