Interview by Justin Karter.
This week, MIA Radio presents the fifth in a series of interviews on the topic of the global “mental health” movement.” This series is being developed through a UMASS Boston initiative supported by a grant from the Open Society Foundation. The interviews are being led by UMASS PhD students who also comprise the Mad in America research news team.
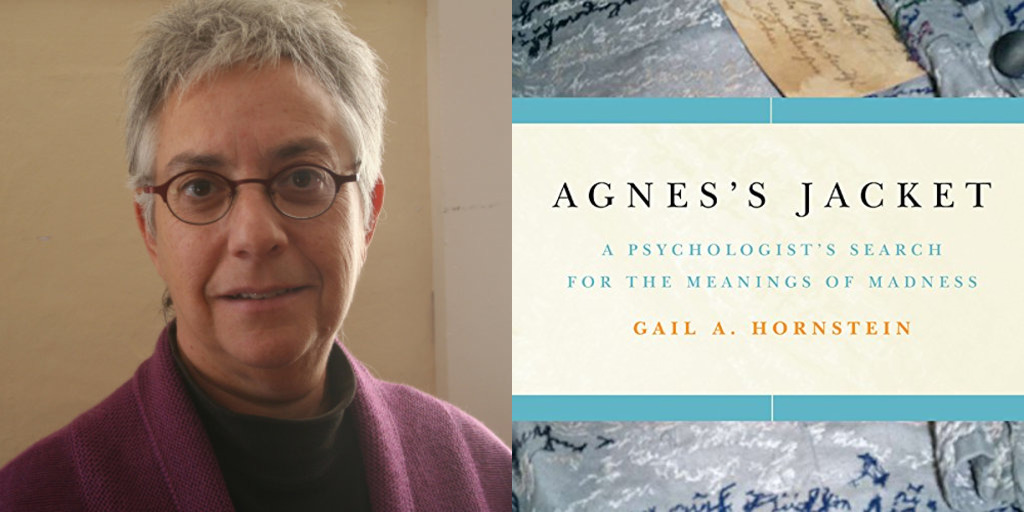
I was fortunate to interview Dr. Gail Hornstein, a Professor of Psychology at Mount Holyoke College in South Hadley, Massachusetts. She is the author of To Redeem One Person is to Redeem the World: The Life of Frieda Fromm-Reichmann and, most recently, Agnes’s Jacket: A Psychologist’s Search for the Meanings of Madness. In her work, she chronicles both the personal narratives of people with lived experience of being treated as “mad,” and also the growing movement of survivor and service-user activism. Her Bibliography of First-Person Narratives of Madness in English (now in its 5th edition) lists more than 1,000 books by people who have written about madness from their own experience; it is used by researchers, clinicians, educators, and peer groups around the world.
She is now director of a major research and training project investigating how hearing voices peer-support groups work, supported by a grant from the Foundation for Excellence in Mental Health Care. This project is training dozens of new hearing voices group facilitators across the US and sponsors research to identify the key mechanisms by which this approach works.
What follows is a transcript of our conversation, edited for clarity.
JK: Thank you for joining us today, Dr. Hornstein.
GH: Thank you, Justin. I’m delighted to be here.
JK: Thanks, to dive right in, in what ways do first-hand personal stories of madness provide a counter-narrative to the dominant discourse in the mental health professions?

GH: I think that using the framing of “counter-narrative” is helpful in that it makes clear that multiple narratives can be offered to explain the anomalous experiences that many people have. The framework provided by psychiatrists, psychologists, and other mental health workers is an important one, and of course, as you say, it shapes the dominant discourse in the United States. However, throughout history, there have always been alternative approaches to understanding the kinds of complicated and often very distressing experiences that are called mental illness or madness, and people who have first-hand experience of psychiatry have provided many of these alternative approaches.
The problem is that because the evidence base for the dominant approach is contested at best and shaky at worst, it is not clear that any one way of explaining these phenomena has a stronger claim to authority than any other approach. And here is where the perspectives of people with first-hand experience become especially important because they often have at least as much evidence to support them as do the perspectives of mental health professionals.
In other words, it’s not just a question of human rights, although of course, human rights are extremely important here. People ought to have the right to define their own experience, but I am also talking about good science as well as human rights. If a perspective like the biomedical model of mental illness does not have clear scientific evidence to support it, then other perspectives, let’s call them counter-narratives, become especially important because these approaches might have as strong, if not stronger an evidential base.
JK: You are currently directing a national study of the effectiveness of hearing voices peer-support groups. Could you speak to how this approach challenges psychiatric orthodoxy?
GH: Psychiatrists see the experiences that get diagnosed as hallucinations — whether auditory, visual, olfactory, etc.–as resulting from faulty brain processes that in and of themselves have no particular meaning. So if someone says, “I hear a voice that’s telling me that I’m a bad person,” for example, mainstream psychiatrists would pay very little attention, if any, to the actual content of what the voice or voices are saying to the person, but rather would focus mainly on trying to stop these voices from occurring. In most cases, a psychiatrist would prescribe medication to the person or would teach them distraction techniques so that the voices might stop entirely or, if not stop, at least be less dominant in the person’s experience.
It’s very rare for biological psychiatrists to ask patients questions about what the voices are actually saying, what their content is, or what they might mean. Their rationale is that if these experiences are the result of faulty biological brain processes, then it doesn’t really matter what the content is. What you want to do is stop the phenomenon from occurring. And psychiatrists worry that if the person talks about the voices or listens to the voices or pays attention to the voices that they will further retreat into what a psychiatrist would call a delusional world, a world that’s not real. From this perspective, an important part of treatment is getting the person to understand that their voices are not real and therefore they shouldn’t be paying attention to their content. Instead, they should be doing things to try to stop them.
The Hearing Voices approach takes a very different view, assuming that all psychological experiences are meaningful, and although sometimes it is difficult to determine the meaning, it can ultimately be interpreted or deciphered. Our assumption is that there is always meaning to experience and paying attention to voices can often allow us to understand more about why the voices are there in the first place. So one of the things that we have learned over the past 30 years in research and practical application of the Hearing Voices approach is that when people pay attention to their voices and indeed when they try to understand specific aspects of their voices and the contexts in which they are distressing, it’s extremely helpful.
What happens in hearing voices peer-support groups is that people ask one another detailed questions about their voices in an effort to understand how they work, why they’re there, and what their particular meaning might be for that person. They might ask one another questions like: “What do the voices say?” “How many voices are there?” “Have they changed over time?” “Is the voice you hear today the same as the voice you heard six months ago?” “Are there certain situations where they’re most likely to appear?” “How do you feel when they’re there?” “What purpose do you think they serve?” “What tone do they use?” And so on. In other words, questions designed to help the person get a detailed and contextual understanding of an experience that has probably baffled them and perhaps terrified them over a long period but which they have been taught by mental health professionals to ignore or at least try to ignore. And what we find in hearing voices peer-support groups is that perhaps paradoxically from the point of view of the mainstream mental health perspective, when people focus on their voices and try to understand them, they often decrease in intensity and their distressing aspects become less problematic.
For example, people might become aware of positive voices that they hear, and these positive voices can help to reduce the distress of the negative voices. In fact, the existence of positive voices that many people experience is something that doesn’t even make sense from a biomedical point of view. There wouldn’t even be a way of assuming that there could be positive voices from the point of view that says voices ought automatically to be considered symptoms of psychosis. And, of course, we know that in other cultures and in many subcultures in the United States, voices can have a very important positive and meaningful function. Every spiritual tradition in the world has inspiring leaders who had some kind of experience of hearing voices: Jesus, Moses, Mohammed, the prophets – they all had experiences in which an angel or God spoke to them. And of course, we don’t consider these kinds of experiences to be evidence of psychosis.
Even people who are not prophets but rather are more ordinary practitioners of various spiritual traditions often report some kind of auditory connection to a voice or voices that serve as a guide, something that plays a positive role in their life. We wouldn’t even know about the existence of such positive voices if we hadn’t delved into these kinds of experiences in greater complexity, as we do in hearing voices groups.
The goal of our specific research project is to understand how exactly hearing voices peer-support groups play such an important and positive role for many people around the world. We know that people find these groups valuable because there are now hundreds of groups all over the world and people often go to great lengths to be able to access a group and to participate in it regularly, but we don’t fully understand precisely what makes these groups so effective. Participation in these groups has helped many people to recover fully from distressing experiences associated with their voices, and our project is focused on being able to identify these specific mechanisms.
JK: Your work with the hearing voices peer-support groups makes clear that the mainstream mental health model is inconsistent and out of sync with the experience of many people who hear voices. To move somewhat more generally to the movement for global mental health, critics have accused the movement of spreading a Western model of mental ill health that is inconsistent with the experiences of people in diverse cultures. What is the role of culture in the experience of madness more generally, and how does including culture in the picture perhaps make this Western mental health model even more problematic?
GH: Well, culture is crucially involved in every aspect of our experience. Indeed, it’s probably a category error to think that we can even separate out some kind of variable called culture and look at it in isolation. There is no aspect of our psychological experience at any moment of our lives that is not shaped by and in response to culture in some respect. So the question is a little bit artificial, but I understand why you’re asking it. And here I think we need to focus specifically on the pathologizing assumptions of Western culture about an experience, for example, like voice hearing, but also many other kinds of experiences that get labeled as mental illness.
As we know, for example, from the important work of Ethan Watters in his book, Crazy Like Us, people in different cultures experience what we might call the same kinds of feelings, perceptions, and thoughts in very different ways. Now again, we can’t be totally certain that they’re exactly the same. There are many methodological issues involved in evaluating private psychological experiences in different cultures. There are problems of translation — what do the words even mean that we’re asking? But still, if we set those problems aside for a moment and just think about overall assumptions about how we understand psychological experience in current biomedical, Western psychiatry – and I emphasize current because this hasn’t always been the case – the assumption is that any distressing experiences that end up getting diagnosed as mental illness come from faulty brain processes and have little to do with the context of someone’s experience and in particular, they have little to do with trauma.
From our experience in the Hearing Voices Network, many, many people identify the causes of their voices, especially their distressing voices, as directly linked to earlier trauma in their lives. The fact that many Western mental health practitioners, but of course not all, ignore trauma makes it very, very difficult to make sense even in our own culture of the kinds of experiences people are having.
But certainly in other cultures where people might understand what is happening to them in terms of, for example, problematic relationships with their families or with their community rather than as some kind of faulty brain process, we see a real disjuncture between the Western biomedical approach and the way people understand their lives on their own. I especially want to emphasize that if we take solely a biological view toward understanding psychological phenomena, we leave out crucial aspects of what makes people’s experience meaningful, especially social, interpersonal, and cultural aspects of their experience and the particularly important role of trauma.
I emphasize that this is the current Western view because prior to the 1970s, and especially from a psychoanalytic point of view, trauma was always considered to be a crucial causal factor in bringing about distressing psychological experiences. And even in the United States prior to the 1960s, the assumption was that people who ended up with a diagnosis of schizophrenia, for example, or any kind of psychotic diagnosis had experienced trauma early in their lives and working through those traumas in adulthood, particularly in psychotherapy, could enable them to fully recover. It is only in the last 30 or 40 years since the biomedical model has become so dominant in the United States, Europe, and the UK, that we have seen such a huge gap between the Western model and other ways of understanding psychological experience.
JK: Thank you. Another criticism of the Movement for Global Mental Health and specifically the Lancet Commission on Global Mental Health has been the failure to include the voices of people with lived experience in the overall project. In your book, “Agnes’s Jacket,” you chronicle the rich history of the psychiatric service user, consumer, and survivor groups developing research and treatments for experiences of madness. In what ways do these personal narratives challenge the global mental health project and how might they be included?
GH: If we don’t start from people’s lived experience, then we rob ourselves of a huge amount of important information that could enable us to understand distressing experiences more fully. For example, if we don’t pay attention to the contexts in which someone’s distress occurs, it becomes much more difficult to help the person figure out how that distress might be lessened. One of the biggest errors I think of the Western biomedical model is to assume that if someone has, for example, a diagnosis of schizophrenia, that their behavior is disordered at every moment and in every context. In fact, we know that the opposite is true –people’s feelings, experiences, perceptions, thoughts, behaviors, etc. vary a great deal across different contexts and there is crucial information to be gained from understanding those variations and encouraging people to pay attention to them so that they can have a greater degree of autonomy over their own experience.
As I said earlier, this is partly an issue of human rights. The slogan of the disability rights movement, “nothing about us without us,” contains a crucial lesson for all of us to learn. In addition to the human rights aspects of this issue, as I have already noted, we need to have good science, and we don’t have good science if we ignore crucial sources of data. So, for example, one of the things we know from the Hearing Voices Network is that people often fully recover even from very distressing experiences. Even if they have been patients in the mental health system for many years, they can still fully recover. This is not something that the biomedical model assumes to be possible. So if we are exporting to the rest of the world a view that is unduly pessimistic and not based on the actual evidence of what happens in people’s lives, we’re doing everyone a disservice.
There’s an important concept that Dr. Andrew Weil, the natural health practitioner, introduced, which he called “medical hexing,” pointing to examples like a physician saying to a person or to their family, “you’ve got to come to grips with the fact that you’re never going to get better, “ or “You’ve got schizophrenia, and that is a serious and persistent mental illness which you’re going to have for the rest of your life.” Or, “You have bipolar illness, and that’s a cyclical form of disorder, you’re always going to have these cycles, and nothing is going to be able to stop them.” Andrew Weil argues that it is like putting a hex on someone, basically using the self-fulfilling prophecy in its most negative form to say to the person, “there really isn’t any hope for you here.” And not only is that ethically very problematic, but it’s also factually wrong on the basis of what the evidence that the Hearing Voices Network and many other members of the activist and survivor communities around the world have demonstrated.
JK: Thank you. You’ve spoken today about good science and how including personal and first-person experience actually leads to a better and more robust science for mental health research. How does including first-person experience change the way we even think about what constitutes evidence and effectiveness of various interventions and how would incorporating these perspectives transform our current health care systems and policies?
GH: I think this is really the most important question of all. Evidence in science is of paramount importance, and all of us who have been trained in methodology in graduate school have learned that finding evidence for one’s hypotheses is the crucial activity of science. Hypotheses are not always found to be supported. The criteria for what constitutes evidence is a central question in the philosophy of science and ought to be of concern to everyone who is involved in any kind of mental health initiative.
Unfortunately, the widespread use of medication as a treatment for what gets called mental illnesses has led to a very narrow view and a very quantitative view of what constitutes evidence in the first place. So, for example, the notion of a randomized clinical trial makes a certain sense when what you’re trying to do is evaluate a drug treatment or some other finite intervention. For example, if you have two groups in your study, and you give one group a drug and you don’t give the other group the drug and you have a control group and other proper measures of control in the design of your study, it might be possible to conclude something about whether there is evidence for or against the use of that particular medication or intervention. There’s a certain logic to the use of a randomized clinical trial for that kind of treatment. However, it is a very narrow notion of what constitutes evidence. And we know, for example, from psychotherapy research, that psychotherapy has a profound and powerful effect on many, many people’s lives. But it’s very, very difficult to evaluate the effectiveness of psychotherapy using a randomized clinical trial because we would have to take a group of people and randomly assign them to therapists or no therapists to see whether or not there was any effect of the treatment.
And the crucial thing we know about psychotherapy is that it’s the relationship between the therapist and the patient that is or is not likely to enable change. The relationship is an absolutely crucial part in every form of psychotherapy, and both research and clinical testimony bear this out. So we can’t randomly assign people to therapists in order to evaluate psychotherapy. And this is equally a challenge in our study of hearing voices groups. When we get to something like peer support, we, of course, cannot randomly assign people to groups because the nature of human social life is such that we are going to feel more or less comfortable in a given group. We’re going to find the members and the context of a given group more or less helpful or relevant to the particular situation we’re in and so on. So what we need to do is have a notion of evidence that starts from people’s lived experience and which enables them to articulate in their own way, in their own narrative structures, and in their own vocabulary what it is that is helpful or not helpful about a particular kind of intervention.
What we need in a broader sense are ways of assessing the effectiveness of an intervention using a broader set of methodological tools. This includes, for example, qualitative research, but not only that. It also includes the kinds of measures that people themselves think are important as a way to assess what has helped them or not. We can’t just use a measure, for example, like the number of days in the hospital, which might or might not bear any relation to how the person is experiencing their improvement or lack thereof. In other words, we need to really challenge, on scientific grounds as well as on political grounds and human rights grounds the narrowing of the definition of what constitutes evidence and how we can tell whether or not a given approach is effective.
JK: Thank you very much and thank you for all the incredibly important work you’re doing, and I look forward to seeing the results of your study.
GH: Thank you so much. It’s great to be part of it. If people want to learn more about my work, there’s lots on my website, www.gailhornstein.com.




One of the things I detest most about mental health, inc. is how it dehumanizes people, like lab rats. This does harm in so many ways and is rather vampiristic.
To mental health, inc. clinician/authors: Write about your own mad lives and inner voices, and stop co-opting your clients’ lives and voices for your own personal, professional, and FINANCIAL gain. That is everything which is wrong with the mh academic culture. Please STOP.
Study yourselves. That’s how truth comes to light. Not by projecting onto others.
Report comment
Looks like you have it covered.
Report comment
well you are referring I think to elitism and its effects. However did you even read the transcript? This movement is about activism FROM the inside out. So it is a good thing. From the article itself (which I actually read) “The slogan of the disability rights movement, “nothing about us without us,” contains a crucial lesson for all of us to learn.”
That being the theme of the article, it pretty much negates your attack on mental health professionals.
This is a good thing. Power to the people always!
Report comment
Covering up trauma, particularly child abuse, has been for a century, and still is, the primary societal function of the “mental health professions.”
https://www.indybay.org/newsitems/2019/01/23/18820633.php?fbclid=IwAR2-cgZPcEvbz7yFqMuUwneIuaqGleGiOzackY4N2sPeVXolwmEga5iKxdo
https://www.madinamerica.com/2016/04/heal-for-life/
And the need to misdiagnose all child abuse survivors was intentionally built into the DSM. Today, no “mental health” worker may ever bill any insurance company for ever helping any child abuse survivor ever, unless they misdiagnose them with one of the other billable, but “invalid,” DSM disorders.
https://www.psychologytoday.com/us/blog/your-child-does-not-have-bipolar-disorder/201402/dsm-5-and-child-neglect-and-abuse-1
This is why over 90% of those labeled as “borderline” are misdiagnosed child abuse survivors and over 80% of those labeled as “depressed,” “anxious,” “bipolar,” and “schizophrenia” are misdiagnosed child abuse survivors today. The “mental health” industry has historically always been, and still is today, by design, a child abuse covering up system.
Report comment
Perhaps but it should NOT be. They SHOULD be healers, that’s why we go to them. Criticism of the field is necessary but it doesn’t mean they all engage in this- therapists particularly in my personal experience, are overfocused on childhood experiences to the detriment of current functioning and cognitive or neurological issues which could be easily treated at least temporarily to assist our personal functioning. But the field of psychiatry is a mess considering how greedy they are, paid $400/hour plus pharma rep perks just to undertreat, overmedicate and disrespect our humanity!!
Report comment
Sure, the mainstream of psychiatry is only NOW figuring out that “borderline personality disorder” is pretty much a form of PTSD resulting from childhood trauma. But because it was a female-oriented disorder they were reluctant to read the symptoms correctly- easier to diagnose with a personality disorder! They’re “crazy”! They’re only NOW offering a “new” form of PTSD- “C-PTSD”- to those suffering from long-term, chronic traumas; where in the past only war vets could get PTSD..that evolved into war vets and accident and rape/crime victims who got PTSD. Now they’re recognizing that others get it, that similar symptoms arise from repeated traumas which are lower level in intensity (slaps, verbal abuse etc) but consistent over long periods.
This reluctance of Psychiatry to see common sense and its slowness to progress reduces its validity as a medical science more than a patient could ever reduce their validity as an important actor with a voice on the field of health. Basic human rights are basic human rights.
Report comment
I don’t see the problem as encapsulated by the term biomedical model entirely. I once tried to talk to the head of the psychology department at UVA about speaking before classes there, and got nowhere. The survivor voice, the patient experience, was seen as anecdotal besides all the “evidence” these “researchers” were gathering, and therefore something not worthy of consideration (i.e. “unscientific”). Okay, the torture goes on pretending that it is something else. When you’ve been rendered “voiceless”, that is, you’ve got “no seat at the table”, what then? What calls itself “science”, in this case, wants to make sure you have “no seat at the table”. I guess democracy is very threatening to some people.
Report comment
Truth certainly is very threatening to some people! All you said, Frank, yep, exactly. YOUR voice is the one that mattered in that scenario. This industry runs on co-opted voices (and lives!). We take them back, they’ve got no fuel, or foundation, or reason to be. Spread the word…
Report comment
Pretty soon the social networks will be shutting down anti-psychiatry information just like they announced last week they were doing with anti-vaccine info. Try to google that now and see what you get.
Report comment
I am pretty disgusted by the movement to silence ANY discussion of vaccine science that doesn’t totally support that every vaccine ever invented is safe and necessary. I got temporarily tossed off another site for mentioning that the flu vaccine is not generally very effective against the flu, and should probably not be a priority for anyone who isn’t in a high-risk group. I provided a link to scientific research on the point I raised. But I was accused of posting “antivax propaganda.” Pretty authoritarian, and ironic, as people accusing others of being antiscientific are denying anyone else the right to post scientific information and to discuss its implications. I complained to the moderators, to no effect. Disgusting.
Report comment
“I got temporarily tossed off another site for mentioning that the flu vaccine is not generally very effective against the flu, and should probably not be a priority for anyone who isn’t in a high-risk group. ”
And in the real world, people consider this common knowledge! Censorship is scary, indeed!
Report comment
Good thing you didn’t say anything about mega ascorbate and flu prevention. Someone would be filling out the commitment papers in a flash.
Report comment
“he survivor voice, the patient experience, was seen as anecdotal besides all the “evidence” these “researchers” were gathering, and therefore something not worthy of consideration (i.e. “unscientific”). ”
Bingo- meanwhile this “evidence” is largely comprised of BigPharma-funded studies to validate meds’ efficacy so more $$$ for them all. But the patient’s own reality and needs are placed second if at all, and even If you can GET quality insurance to begin with. Industry greed is stealing our country.
Report comment
What a great interview! I am amazed and saddened by the fact that we still haven’t been able to document how HVN groups reduce hospitalization. Keep up the great work Gail!
Report comment
An important consideration was entirely left out of this article. I want to bring this to the attention of any journalist or researcher on lived experience.
Real peer functions have been largely coopted by the biomedical model. This is done in the form of certifications with exams, and by the very expensive trainings needed to pass them. Also by the sources of funds to pay professional peers.
What kind of peer support comes from someone controlled by the psychiatric medical establishment?
Report comment
You point out some valid points. The certification required of anyone wanting to be a peer worker in the state where I live is so oriented towards lots of paperwork and hours worked under a supervisor (who aren’t people with lived experience) and educational hours galore that it’s ridiculous. A social worker that I know looked at all the requirements and said that the peer certification required more than what social workers were required to submit for their certification. And then in the end they stick you with a nice hefty fee to pay for your certification.
One of the sole reasons that any certification was created at all was so that any work done by a peer could be billed for Medicare funds. And billing for Medicare funds demands that you must chart and write notes. This goes against all peer standards since if you get to write about people you have power over them. If you can enter notes in their charts you have power over them. Peers are supposed to form mutual relationships with people so that both parties can learn from one another. If you have the power of the pen you are above those you’re writing about and there is no mutual relationship. Of course, the relationship is not totally mutual because one has keys and a badge that the people being “treated” don’t have. You get to go home at the end of your shift, the people on the units are held against their wills.
Report comment