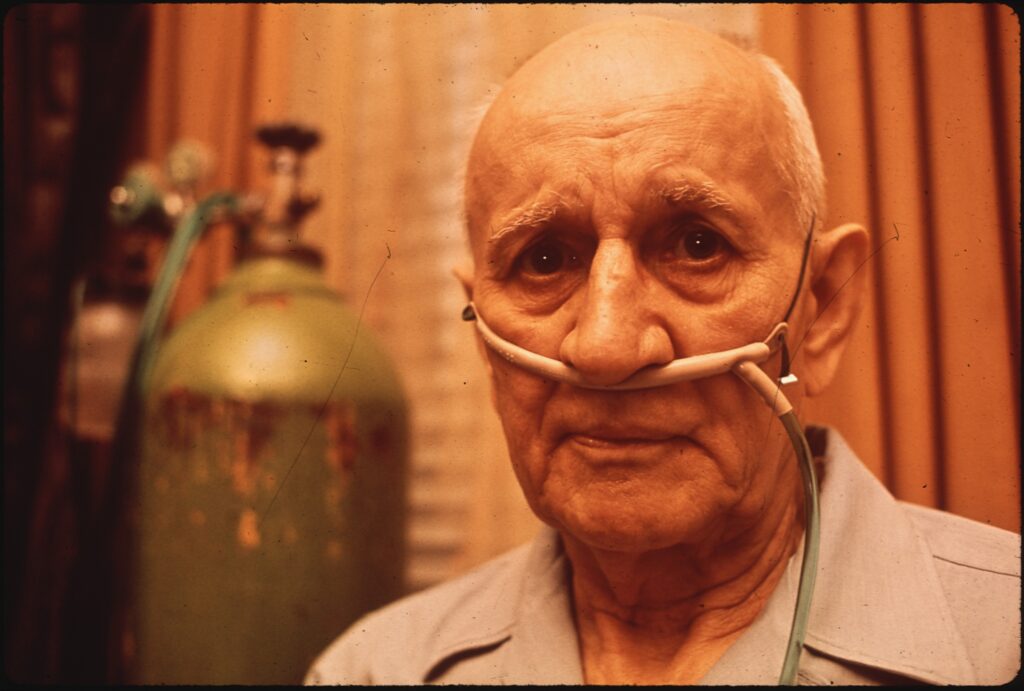
In a recently published article in JAMA Psychiatry Meng-Ting Wang and his colleagues conducted an analysis on a group of patients in Taiwan with chronic obstructive pulmonary disease (COPD) to determine whether the risk of experiencing acute respiratory failure (ARF) is higher if patients with this chronic illness are prescribed antipsychotic medications. Their findings indicate that “the use of antipsychotic drugs was associated with a 1.66-fold increased risk of ARF within 14 days of therapy initiation”. COPD which includes chronic bronchitis and emphysema, is a chronic lung disease that makes it hard to breathe. ARF is a “serious complication” related to COPD which often requires intense care, hospitalization and a high mortality rate (49% of patients die within a year).
Other studies have examined the effect of long-term use of antipsychotics and concluded that they lead to poorer cognitive functioning, have adverse side effects, negative effects on physical health, and lead to changes in brain structure. This group of researchers was interested in examining the incidence of ARF in patients with COPD after short-term exposure to antipsychotics – they examined the occurrence of ARF events within a 14-day period after medication use. Their interest stemmed from reports of 12 patients who experience respiratory complications within hours to 10 days of using antipsychotic drugs. However, a “population based analysis” to determine the safety of prescribing antipsychotics to patients with COPD had not yet been conducted.
The researchers used a case-crossover design in which patients with ARF were compared with themselves during an earlier time period – this “design compared the use of antipsychotics during the period immediately before the ARF event (case period) and during an earlier control period for each patient with ARF”. Cases were drawn from the Taiwan Longitudinal Health Insurance Database January 2000 – December 2011. The “case” period was defined as the development of ARF 1 to 14 days, whereas the “control” period was 75 to 88 days before the ARF events occurred. They examined the use of both, typical and atypical antipsychotics.
After applying their exclusion criteria, they examined 5032 patients from 11,785 total cases of patients with ARF. Of these, “590 patients (11.7%) filled at least one prescription for an antipsychotic medication during the case period compared with 443 patients (8.8%) during the control period”. Statistical analyses revealed that this represents “an overall 66% increase in the risk of ARF during the first 2 weeks of antipsychotic use, independent of cardiogenic, traumatic, and septic factors.” Further, this risk was also linked to the dose prescribed of the medication – with a dose defined as “high” leading to three times greater the risk of developing ARF compared to a “low” dose.
The possible reasons for this observation are discussed as being the link between the action of antipsychotics on dopamine and serotonin receptors and changes in respiratory function. Some of the limitations of this study are confounding factors like the finding that “psychosis can worsen patients’ lung function”, non-determination of the accuracy of ARF diagnoses, the unavailability of some confounding variables like lung function testing results and smoking status in the health database, and the inability to measure actual antipsychotic adherence.
Nevertheless, the researchers “recommend that healthcare professionals be vigilant regarding the signs of ARF among patients with COPD who are receiving antipsychotics, especially during the initial treatment phase.” This is true of typical and atypical antipsychotics and reducing the dose of the medication may be tried but is not a foolproof strategy for eliminating the risk of ARF. Finally, “high doses of antipsychotics should always be avoided whenever possible.” This study is a contribution to the consideration of the risk-benefit analysis of antipsychotic prescription, especially in patients with COPD.
****
Wang, M., Tsai, C., Lin, C., Yeh, C., Wang, Y., & Lin, H. (2017). Association between antipsychotic agents and risk of acute respiratory failure in patients with chronic obstructive pulmonary disease. JAMA Psychiatry. doi:10.1001/jamapsychiatry.2016.3793 (Abstract)















Indeed. The FDA does not approve of the use of antipsychotics on elderly persons with dementia and psychosis. That’s because of a doubling of the rate of death in such people when given antipsychotics in a group of very short studies like the Taiwanese one. It seems entirely arbitrary to limit the non-approval to individuals with dementia and psychosis. The key is the oldness, and the non-approval should be extended to all elderly persons (then to all of humanity).
Something they’re probably too uninterested to have learned is that persons with Dementia with Lewy bodies are at greatly elevated risk for Neuroleptic Malignant Syndrome if made to take an antipsychotic. As much as 35% of old age dementia is Lewy body dementia, but it’s not often diagnosed properly. It can be diagnosed relatively late, because memory impairment is not typically among the first symptoms to become apparent. Delusions and hallucinations often precede it, and those are not always disclosed by the person experiencing them.
Haldol and other neuroleptics have killed countless elderly people, with and without dementia. There are too many stories of someone’s elderly parent being admitted to a nursing home for short term physical therapy or extended recovery from surgery, and leaving on a gurney, killed within days by idiot, improperly educated, callous and brainwashed employees. They really think Haldol is a great drug. Search AllNurses.com for Haldol or haloperidol if you want an eye-opener. It will keep you from setting foot in a hospital or nursing home unless you have some way to keep the murderous control freaks’ drugs out of your body. Stating in writing that you must not be made to take an antipsychotic isn’t reliable. (StudentDoctor.com is another place to listen in on some water-cooler medical chatter.)
Report comment
is it not obvious that giving a tranquilizer to someone with COPD is not sensible?
Report comment
It does make you wonder just who is out of touch with reality.
Report comment