Utilizing data from the Chicago Follow-up Study, researchers followed 139 initially psychotic patients over 20 years. Published in Psychiatry Research, the study reports that while antipsychotics were beneficial during acute hospitalizations, patients not prescribed antipsychotics had significantly better work functioning than those who were prescribed antipsychotics.
“Negative evidence on the long-term efficacy of antipsychotics have emerged from our own longitudinal studies and the longitudinal studies of Wunderink, of Moilanen, Jääskeläinena and colleagues using data from the Northern Finland Birth Cohort Study, by data from the Danish OPUS trials the study of Lincoln and Jung in Germany, and the studies of Bland in Canada,” the authors write. These longitudinal studies have not shown positive effects for patients with schizophrenia prescribed antipsychotic for prolonged periods. In addition to the results indicating the rarity of periods of complete recovery for patients with schizophrenia prescribed antipsychotics for prolonged intervals, our research has indicated a significantly higher rate of periods of recovery for patients with schizophrenia who have gone off antipsychotics for prolonged intervals.”

Authors of this study draw attention to previous research that has pointed out the lack of evidence on the effectiveness of antipsychotics after 3-years. The present article adds to previous research presented in the Danish OPUS trial which demonstrated improved functioning and higher rates of employment after ten years in patients off antipsychotics.
The authors of this longitudinal study aimed to measure work functioning in patients with schizophrenia on long-term antipsychotic treatment compared to patients with schizophrenia not on antipsychotics controlling for symptom level and premorbid achievements.
Using data from the Chicago Follow-up Study, a study examining functioning, outcome, and recovery in psychotic disorders, 139 patients (psychotic schizophrenia, n= 70; control sample (psychotic mood disordered), n = 69) were followed over a 20-year period. Patients were recruited and initially assessed during an acute phase of hospitalization and followed up at 2 years, 4.5 years, 7.5 years, 10 years, 15 years, and 20 years.
Of the 70 patients classified as having schizophrenia, 58 were followed up at the 20 year period, 30 were assessed at all 6 follow ups (2, 4.5, 7.5, 10, 15, and 20 years), and 32 were assessed at 5 follow-up periods. Two patients were assessed at 4 follow-ups and 6 at less than 4 follow-ups. 25 patients were always prescribed antipsychotics and 15 were not prescribed antipsychotics from the 2-year follow-up onward. These two comparison groups were used in assessing the long-term differences between patients on vs. off antipsychotics.
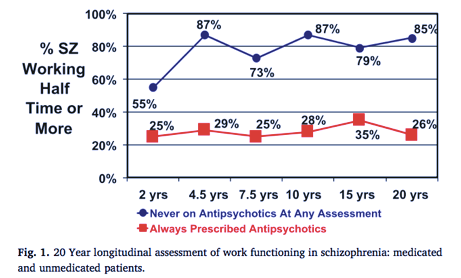
The chart above presents the work functioning of patients continuously prescribed antipsychotics (n= 25) vs those not on antipsychotics over the last 18 years (n=15). As the figure shows, the only time point where there was no significant difference between the on work functioning between the two groups was during the 2-year period.
At each of the remaining time points, the unmedicated group performed significantly better on work functioning (.000 -.016 ). From the 4.5 year assessment on, over 65% of patients not on antipsychotics were working half-time or more.
Moreover, patients continuously prescribed antipsychotics were significantly more likely to have negative symptoms than those not prescribed antipsychotics at 4.5 years and 20-year follow-up and those with negative symptoms were less likely to be working at 4 of the 6 follow up periods.
When controlling for prognosis, patients with poor prognosis not on antipsychotics had better work functioning than those with poor prognosis prescribed antipsychotics. No significant differences were found between the medicated and unmedicated groups with good prognostic potential, which the authors point out may be due to the small number of patients with a good prognosis.
When controlling for premorbid achievements, those with poor premorbid achievements not on antipsychotics had significantly better work functioning than those prescribed antipsychotics with poor premorbid developmental achievement. Among the small number of those with good premorbid achievements, more of those not on antipsychotics were working than those taking the drugs.
When combining all results on symptom and functioning of the 70 patients with schizophrenia across all six follow-ups, results did not support the use of antipsychotics to improve functioning and the odds ratio conducted by the authors demonstrated that those not on antipsychotics were 1.76 times more likely to have adequate work functioning compared to those on antipsychotics.
The results of this study add to the growing literature demonstrating a lack of long-term positive effects of antipsychotics for patients identified as having schizophrenia. The researchers add that in other published papers, they have reported a higher rate of recovery in those off antipsychotics.
Overall, the results of this study make clear that after the 2-year mark (at which the differences are not significant), those off-antipsychotics have better outcomes. The authors write:
“The data indicate that any hypothesis based on the view that antipsychotics facilitate work functioning are extremely doubtful since the results for work functioning were running strongly (at significant levels) in the opposite direction.“
****
Harrow, M., Jobe, T. H., Faull, R. N., & Yang, J. (2017). A 20-Year multi-followup longitudinal study assessing whether antipsychotic medications contribute to work functioning in schizophrenia. Psychiatry Research, 256, 267-274. (Abstract)















Mental Illness Fraud
ME To
[email protected] at 12:32 Today
Dear Karen Buck MP
Severe Mental Illness is supposed to be more disabling than being blind or in a wheelchair.
My GP Surgery keeps playing around with terms like “schizophrenia” to the Point that I am now too frightened to go on to a building site.
(I sent you an email earlier today at 11.15 with the details).
Yours Sincerely
ME
Report comment
Hey Fiachra ever heard of the ‘schizophrenia challenge” it goes like this -‘ patient’ ( client/consumer/victim/inmate) “Hey doc if you think this poison is so great why don’t you take it then, it might help relieve you of a few of the fixed false ideas you’ve been hawking around about me and improve your social skills, maybe even your occupational functioning, why not have a go then it just might help? ”
Doc thinking to self – I can see this is not going to go well.
Well normally this approach is fraught with danger and rarely goes as intended. Sometimes the doc actually takes up the challenge though and within hours of taking just one tablet finds their mind in an awful mess, their occupational and social functioning falling apart and occasional start getting suicidal and wanting to die.
So called ‘Schizophrenia’ the world’s worst insult mascarading as a legitimate disease is as far as I know the only condition where the treatment causes the majority of its (alleged) ‘symptoms’.
Good luck with getting your MP interested, however insisting your afraid to walk onto a building site may not prove very helpful (just saying).
Report comment
Aw, I bet even people without “schizophrenia” show better work functioning off neuroleptic drugs.
Report comment
I bet they do!
Report comment
Is it possible to give a rough guess on the effect of antipsychotics on recovery?
Thank you for publishing the Harrow 20 years follow-up showing better functioning without antipychotics.
Leucht et al has 2009 found (How effective are second-generation antipsychotic drugs? A meta-analysis of placebo-controlled trials) the effect NNT(Number Need to Treat)=6 for short time treatment (1). However this was looking at symptoms on the Positive and Negative Syndrome Scale (PANSS).
Leucht et al 2012 looks at maintenance treatment with antipsychotic drugs published better results but concludes that it is necessary to “clarify the long-term morbidity”.
Bola et al. Cochrane.org 2011 (5) found just 5 studies with real placebo, i. e. RCT. One of them Rappaport et al 1978 found that umedicated patients managed better, e. g. readmission into hospital. NNH turned out to be 2.9 (NNH= number need to harm).
Nancy Sohler et al. gives 2016 this summary: «For many years, this (…)clinicians’ belief in the need for long-term use of antipsychotic medications strong (Lehmann, 1966) that it has been impossible to design a sound observational study to address the question of efficacy or harm … (O)ur study also could not conclusively evaluate whether long-term antipsychotic medication treatment results in better outcomes on average. We believe the pervasive acceptance of this treatment modality has hindered rigorous scientific inquiry that is necessary to ensure evidence-based psychiatric care is being offered.»
So I understand there are nearly no RCT controlled studies (avoiding «cold turkey» problems) answering my question on recovery.
However is it possible to give a very rough guess?
Approx. 60% or so of first-episode patients may recover without the use of antipsychotics.
Naturalistic studies of e. g. Harrow, M. & Jobe, T.H. (2012), Harrow et al 2014 (11), Wunderink (4,7) and Wils et al 2017 show that patients do better without long-time antipsychotic medication.
Jaakko Seikkula et al 2010 (Journal Psychosis Volume 3, 2011 – Issue 3) has reported on long-term outcome of first-episode psychotic patients treated with Open Dialogue Therapy in Western Lapland approx. 80% recovery (6). Showing the benefit of using not much medication supported by psychosocial care. The effect of cognitive therapy (8) and psychotherapy (9) is documented.
Bjornestad, Jone et al. 2017 reported “Antipsychotic treatment: experiences of fully recovered service users”: “(b)etween 8,1 and 20% of service users with FEP achieve clinical recovery (Jaaskelainen et al., 2013)” under the profession’s current protocols.
Now I know this guess is not exact science, but does it seem that approx. 40% of patients subject to regular medication (e. g. in Norway “National guideline for diagnosis, treatment and follow-up of individuals with psychotic disorders”) loose long-term recovery compared to non-medicated patients?
Would this be a fair rough guess of the long-term effect of antipsycotics on recovery?
Patients have a right to know in advance to decide with informed consent the benefit of actual symptom reduction in the beginning at the price of long-term reduction of recovery. Where there is a risk there has to be a choice.
I would appreciate your answer based on your knowledge of studies. Thank you in advance.
Report comment
The only thing more disabling than Severe Mental Illness is supposed to be being paralysed from the neck down.
If people are able to work are they Shizophrenic?
Report comment
Why are you perpetuating the fallacy that there is such a thing as schizophrenia? And why would anyone cooperate with this study instead of telling off the researchers?
Report comment
The researchers are insane and refuse to admit they are insane. Who is to tell them differently? Who has the power?
The next step in the case where someone is wrong , is a higher authority is supposed to judge what is going on, such as the police. But in this world there is no police , there is no higher authority.
Specifically “telling off the researcher” just makes more (false) scientific evidence . When people don’t participate (as can be expected) they remove them from the evidence base.
Report comment