Last month, Anna Lembke, M.D., Jennifer Papac, M.D., and Keith Humphreys, Ph.D. published a perspective piece in the New England Journal of Medicine detailing the urgent need to address inappropriate prescribing of benzodiazepines.
“Despite the many parallels to the opioid epidemic, there has been little discussion in the media or among clinicians, policymakers, and educators about the problem of overprescribing and overuse of benzodiazepines and Z-drugs, or about the harm attributable to these drugs and their illicit analogues.”
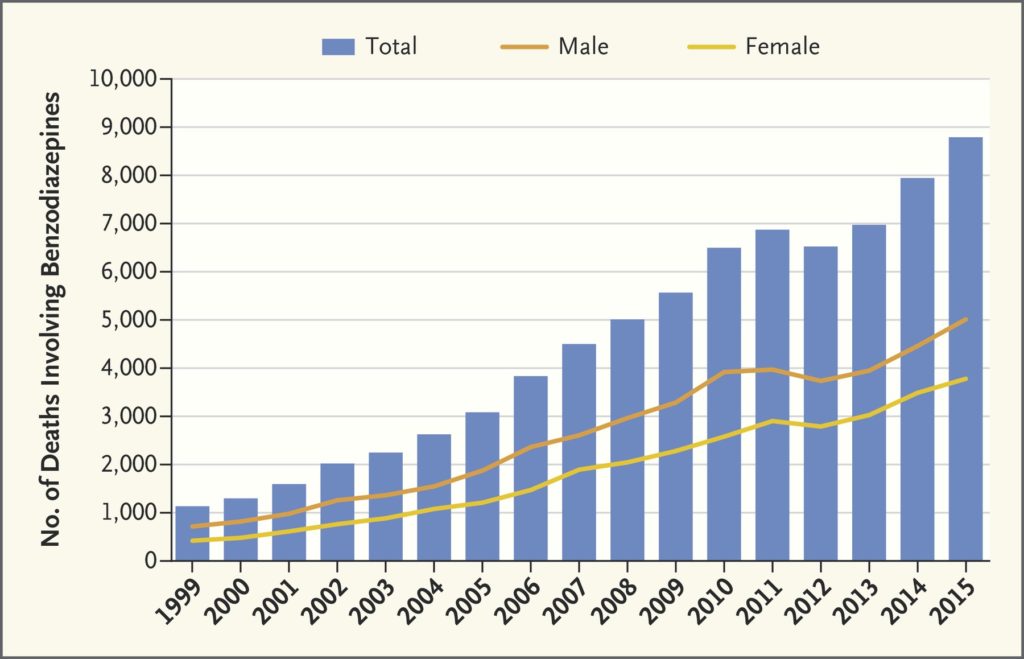
From the National Institute on Drug Abuse.
The use of benzodiazepines, which are controlled substances such as alprazolam, clonazepam, diazepam, and lorazepam, has dramatically increased within the past few decades. Between the years 1993 and 2013, the number of adults who filled a benzodiazepine subscription risen from 8.1 million to 13.5 million– a 67% increase.
Prescriptions correspond to the Food and Drug Administration (FDA) guidelines outlining the approval for benzodiazepines to treat anxiety, insomnia, seizures, and acute alcohol withdrawal. Yet, the drugs are also prescribed off-label for a number of reasons, the authors write, including restless leg syndrome and depression.
Alongside the accelerating number of adults filling benzodiazepine prescriptions, deaths resulting from overdose have risen from 1,135 in 1999 to 8,291 in 2015. The authors note, however, that benzodiazepine overuse, misuse, and addiction go mostly unnoticed.
Part of the reason, they hypothesize, may be because three-quarters of deaths involving benzodiazepines also involved opioids. Yet, rates of co-prescribing benzodiazepines and opioids have nearly doubled since 2001. While the opioid epidemic has appropriately received widespread attention, Lembke, Papac, and Humphreys question why the same attention has not been garnered for similar trends in benzodiazepine use.
“It would be a tragedy if measures to target overprescribing and overuse of opioids diverted people from one class of life-threatening drugs to another. We believe that the growing infrastructure to address the opioid epidemic should be harnessed to respond to dangerous trends in benzodiazepine overuse, misuse, and addiction as well.”
Moreover, new highly potent and deadly versions of benzodiazepines have become available through an illicit market. These are known as “z-drugs,” and they are associated with increased mortality when taken either alone or in conjunction with opioids.
Given the dangers associated with benzodiazepine use, both in isolation and alongside opioids, the authors suggest prescribers become more aware of the risks involved and aspire toward tapering with clients stabilized using opioid-agonist therapy.
“Many prescribers don’t realize that benzodiazepines can be addictive and when taken daily can worsen anxiety, contribute to persistent insomnia, and cause death. Other risks associated with benzodiazepines include cognitive decline, accidental injuries and falls, and increased rates of hospital admission and emergency department visits,” they write.
Furthermore, educators and policymakers can address the misuse and overprescription of benzodiazepines alongside efforts to address the opioid epidemic. More specifically, prescribers can be encouraged to check state prescription drug monitoring program before prescribing. The authors specifically address educators and policymakers as they suggest greater attention and education around the safe prescribing of benzodiazepines and encourage immediate efforts to terminate illegal online pharmacies.
“We believe national efforts to reduce overprescribing of opioids and to educate the medical and lay communities about their risks should be expanded to target benzodiazepines. Educators and policymakers could address the overprescribing and overuse of benzodiazepines in tandem with current efforts to curb the opioid epidemic.”
****
Lembke, A., Papac, J., & Humphreys, K. (2018). Our Other Prescription Drug Problem. New England Journal of Medicine, 378(8), 693-695. (Full Text)















“Psychiatrists Warn Policymakers Benzodiazepine Overuse Could Lead to Next Epidemic.” Maybe the psychiatrists should stop force drugging people with this class of drugs then?
I had lorazepam, plus 13 other drugs, medically unnecessarily forced upon me, against my will, by this now FBI convicted doctor and his not yet arrested psychopathic psychiatric partner in crime at Advocate “Good” Samaritan hospital.
https://www.justice.gov/usao-ndil/pr/oak-brook-doctor-convicted-kickback-scheme-sacred-heart-hospital
The psychiatrists who are medically unnecessarily force drugging people (to cover up prior iatrogenesis and medical evidence of child abuse) with these drugs, for profit, are the problem. $30,000 was defrauded from my private health insurance company for that medically unneeded medical poisoning.
These lunatic doctors think it’s clever to “snow” people, in the hopes of making the patients unable to breath, so they may perform unneeded tracheotomies on people for profit – which is what that doctor was eventually found to be doing to many patients. Although he was only arrested for Medicare/Medicaid fraud.
Who are the psychos? The psychiatrists and doctors who are medically unnecessarily force drugging people with these drugs. The psychiatrists are the problem, not the heroes.
Although, I will agree the doctors are also insane people who believe the opioids are “safe pain killers.” I had no idea doctors were so staggeringly stupid and ungodly unethical.
Report comment
which are safer benzos or anti-psychotics like abilify
Report comment
If by safer you mean less addictive Abilify is kind of safe. I took it for 7 years and tapered off in 8 weeks with only a few bad headaches.
Report comment
But of course, long-term users are more likely to develop diabetes or heart disease.
Report comment
Got off it just in time! Border line diabetes and heart arrhythmia. Both are better after 18 months. Losing 35 pounds helped.
Report comment
Abilify gave me the worst akathisia. I couldn’t sit still.
Report comment
benzo, as no such thing as psychotic molecule.
Report comment
abilify or valium…which is worse
Report comment
That question is kind of like the game, “Would you rather?” Would you rather have one finger cut off or have to sleep every day in a dumpster for 20 years? Guess what, I wouldn’t want to do either!
Report comment
Are there any positive life changes you could make LittleTurtle? Volunteer, take up a hobby, join a walking group?
Report comment
Legalise all drugs which are currently prescription-only in select places and remove doctors and psychiatry as middle-men, except only as voluntary consultants (if the person wants to use them at all) to give information in exchange for payment (and not as labellers and behavioural-record maintainers).
The community can learn for itself how to use these drugs or taper off of them.
If someone partakes in an “epidemic” type of misuse, it’s on their own heads. There is no need for “well-intentioned policy makers” to butt in.
Report comment
“Many prescribers don’t realize that benzodiazepines can be addictive…”
I wish people would stop using that word “addictive” or “addiction.” It puts the onus on the patient rather than where it should be. Iatrogenic dependence is the phrase that needs to be used. There are very few who take benzos who are addicts. They’ve instead duly taken their pills as prescribed by the doctor. Ativan and Xanax have such a very short half-life, however, that the patient is left with even more anxiety due to the GABA having been hijacked by the benzos in order to enable the calming effect, which in turn causes glutamate to begin to run rampant. This causes tolerance withdrawal. The patient must either up their dosage or switch to a longer-lasting benzo (Valium is preferably better over Klonopin).
I wish I had known all this, but I didn’t start researching until I had terrible vertigo while out walking. No one told me anything about benzos except my sister. When I told her about taking Ativan, she said, “I hope you don’t get addicted.” But I wasn’t worried because I wasn’t “one of those people.” A lesson learned the very hard way…
I’m so glad that there are more and more articles about benzos. At four years out, I don’t know how long I have to go to be rid of the terrible CNS damage. Thank you for this, Zenobia!!
Report comment
Thank you Zenobia for this article. I post some articles on my Facebook but find that my friends don’t really respond. It’s only when you’ve been personally involved that you realize how horrible Benzos are. I believe klonopin made my daughter suicidal and she killed herself after taking herself off of it. No doctors helped her taper. In one hospital they took her from 3 mg to .5 in 6 days. So much progress needs to be made in the medical world to get the word out about short term use for benzos and for tapering protocols.
Report comment
I just dont understand this experience. I have ALWAYS found it difficult to get prescriptions for klonopin or Xanax, without being looked at as a drug abuser by the person prescribing it. In my experience, they all know of their potential for abuse and addiction.
?? Since when did psychiatry suffer this long term memory loss?
Report comment