If antidepressant drugs worked to reduce suicide, we should see a decrease in suicide rates when antidepressants began to be widely adopted. This should be true around 1960 when the first-generation drugs emerged and even more pronounced around 1990 when the SSRIs exploded in popularity.
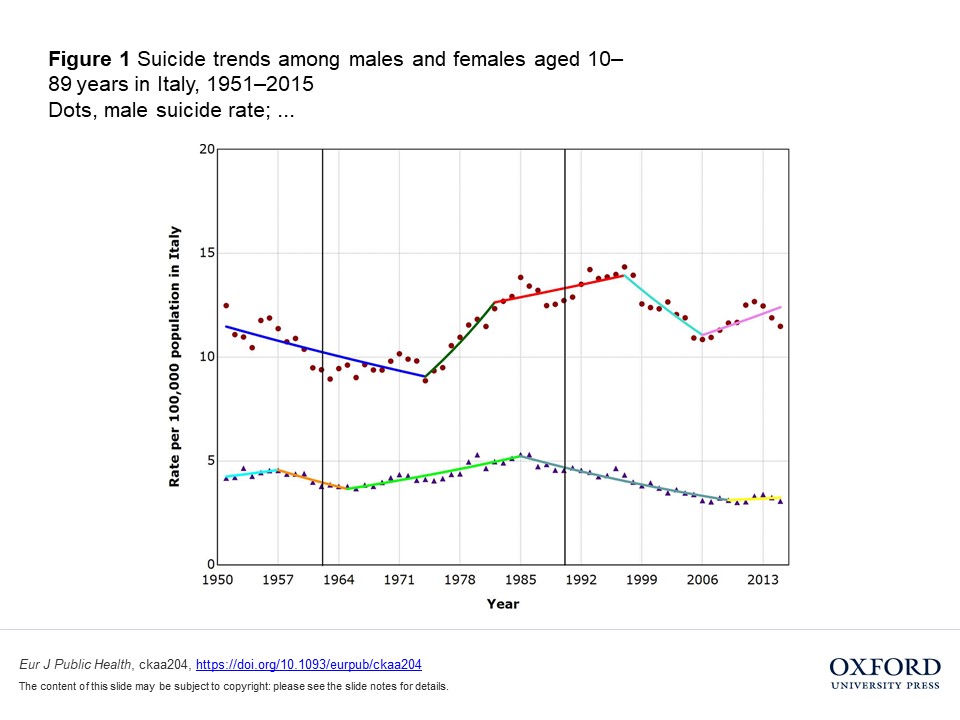
To test this, researchers looked at suicide rates in three countries—Italy, Austria, and Switzerland—over time. They found that there was no association between these time periods and suicide rates. The drugs did not appreciably change suicide rates at all.
“The introduction of antidepressants around 1960 and the sharp increase in prescriptions after 1990 with the introduction of the SSRIs did not coincide with trend changes in suicide rates in Italy, Austria or Switzerland,” the researchers write.

The association between antidepressant drugs and suicidality is controversial. Numerous studies have found that antidepressant drugs actually increase suicidality, especially in children and young adults. However, rarely, some studies have found unclear results, indicating that antidepressants may not have an appreciable effect on suicidality either way in adults (on average).
Some ecological studies have found that antidepressant prescription increases were associated with decreased suicide rates; however, these studies have methodological issues. For instance, they often cover short timeframes (rather than looking at when the drugs actually began to be prescribed widely). This hides situations where the suicide rate was already falling substantially before the drugs began to be used.
Thus, increased prescription of the drugs is statistically associated with decreased suicide—but the trend had already started before the drugs were being used, so they could not be the cause of the decreased suicide rate.
However, proponents of antidepressant use claim that the drugs protect against suicidality. If so, it should be relatively easy to detect this result. Drugs used by tens of millions of people should have a noticeable trend effect right when they became mainstream—if they successfully prevent suicide.
Thus, in their new study, researchers Simone Amendola, Martin Plöderl, and Michael Hengartner analyzed the suicide rates in their respective home countries: Italy, Austria, and Switzerland. They looked at the long-term suicide rates over the decades from the early 1950s to the early 2010s, focusing on both the initial widespread use of MAOIs and TCAs in 1960 and the SSRI boom in 1990. They write:
“Reductions in suicide rates should mostly occur when new antidepressants are first introduced into a population, but there will be much less reduction as use spreads. As a result, assuming antidepressant prescriptions had a clear and sustained suicide-protective effect at the population level, we would expect (i) a decrease in suicide rates around 1960 when the first antidepressants were introduced and (ii) another decrease starting 1990 when the SSRIs were introduced.”
However, the researchers found that the suicide rate did not change at these time-points. For instance, in Italy and Switzerland, the suicide rate was already decreasing substantially since 1950, while a sharp increase in the suicide rate occurred in the late 1960s and early 1970s. For Austria, the suicide rate was relatively stable in the 1950s (neither increasing nor decreasing), but again increased substantially in the mid-1970s.
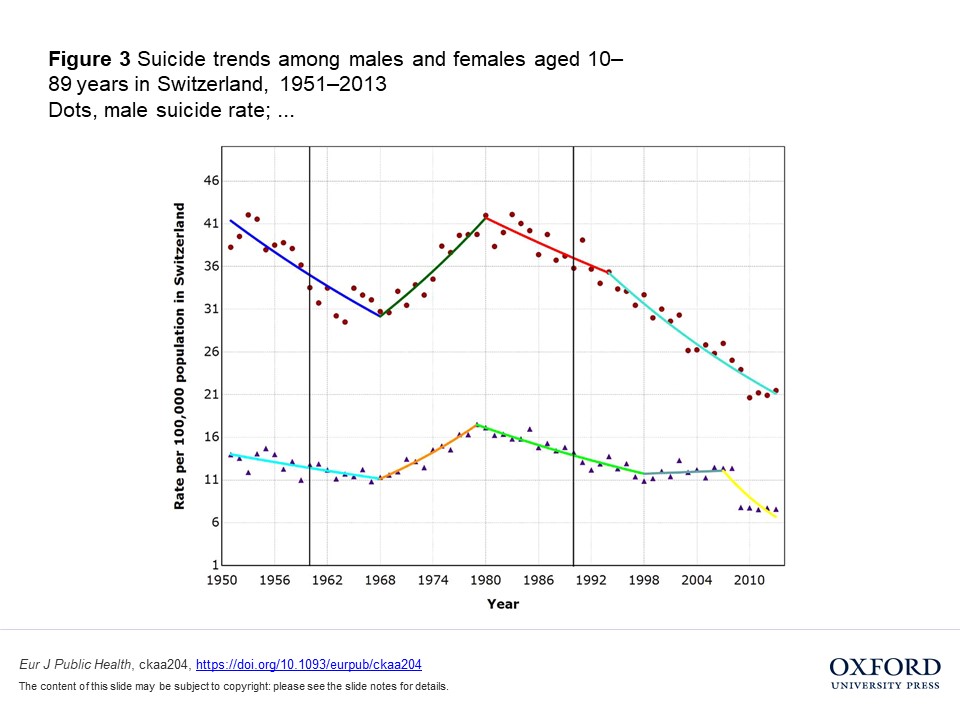
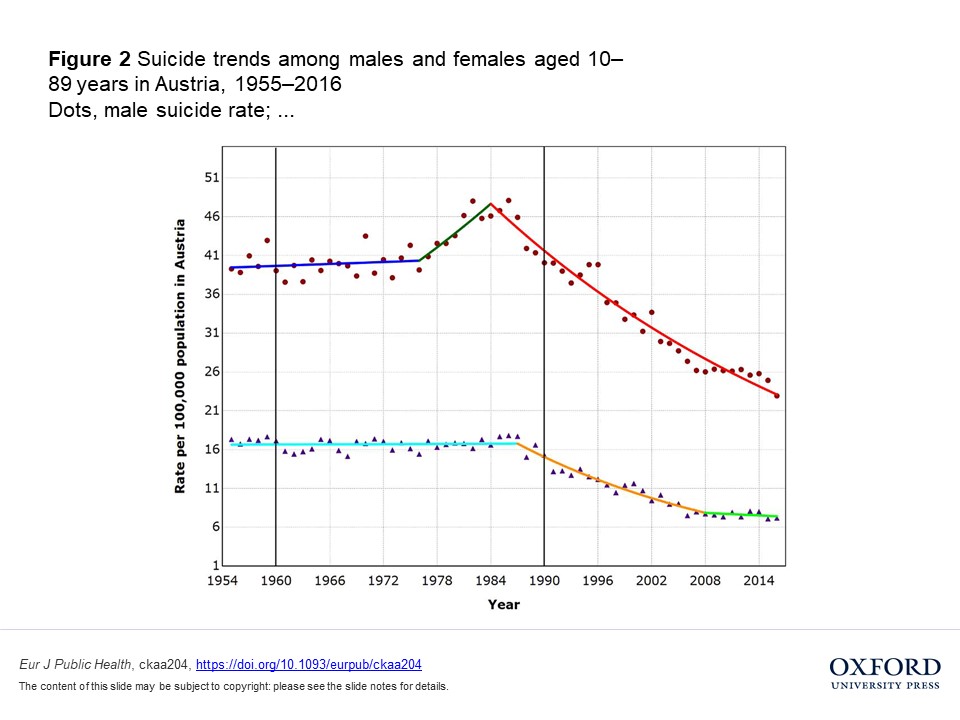 Similarly, the popularization of SSRIs was not associated with changes in suicide rates. In Switzerland, the suicide rate declined steeply from 1980 onward, before the new drugs took hold. In Austria, the same decline happened in the early 1980s—again, long before the big boom of 1990.
Similarly, the popularization of SSRIs was not associated with changes in suicide rates. In Switzerland, the suicide rate declined steeply from 1980 onward, before the new drugs took hold. In Austria, the same decline happened in the early 1980s—again, long before the big boom of 1990.
In Italy, the suicide rate changed drastically—but not around the time-points in question. It actually increased for men while decreasing for women, beginning in the early 1980s, nowhere near the 1990 time-point. A sharp decrease in suicides by men happened around 1998, and then another sharp increase in 2006. These changes appear unrelated to the big prescription boom around 1990.
The researchers write:
“Given that the decline in suicide rates beginning around 1980 in most countries (the putative effect) preceded the rise in antidepressant prescriptions after 1990 (the putative cause), logic dictates that antidepressant prescription cannot be the cause of the declining suicide rates during that period.”
****
Amendola, S., Plöderl, M., & Hengartner, M. P. (2020). Did the introduction and increased prescribing of antidepressants lead to changes in long-term trends of suicide rates? European Journal of Public Health, ckaa204. Published on 25 November 2020. https://doi.org/10.1093/eurpub/ckaa204 (Link)














Suicide never happened in indigenous societies.
However on reservations it is now a major concern.
Must be the genetics that predispose us to depression, or the genetics to be more, or less, “resilient”.
I doubt very much that “anti-depressants” would help. Since they are not dealing with “depression”, but rather the fallout of oppression.
Perhaps the drugmakers can create an “anti-oppression” drug for those who hold power over others.
Report comment
I don’t know about oppression inducing suicides, but I do know that incompetent prescribing does. Most shrinks don’t inquire about unusual perceptual events when diagnosing depressed patients, so they miss depressed individuals who are simultaneously experiencing a number of perceptual distortions, mistakenly prescribing antidepressants for them and making the distorted perceptions worse.
Report comment
Are you trying to be ironic when you talk about genetics? Deconstructing one scientistic fallacy by introducing another doesn’t make much sense.
(Anyway the problem is not simply one group holding power over another, it’s the abuse of that power that makes it a problem.)
Report comment
yes truth, I was being snarky
Report comment
ok np, in retrospect i’m not even sure myself if my argument about the abuse of power being the issue rather than simply holding power over others is 100% accurate (but i would dispute the notion that suicide, or at least highly self-destructive behavior, did not exist in so-called indigenous societies).
Report comment
Thank you, Peter, for honestly reporting on the lies of the big Pharma deluded “mental health professionals.”
Report comment
Sounds about right, when Thomas Insel stepped down as the head of the NIMH in 2015 he admitted that despite spending around twenty billion dollars on brain research during the thirteen years he was in charge they did not improve one measured outcome in mental health in any significant way.
Report comment
Yet they continue to pitch that these are “lifesaving drugs.”
Report comment
They are industry saving drugs.
Report comment
Exactly!
Report comment
A small number of people do seem to benefit from them although the reason may be psychological rather than biochemical; in general it’s like Mark Twain said, don’t count on someone to tell the truth if their ability to earn an income depends on the truth not getting out.
Report comment
We conclude that antidepressant drugs generally appear to reduce suicidal ideation in depressed adults
Antidepressants and Suicide Risk: A Comprehensive Overview
Maurizio Pompili,1,2,* Gianluca Serafini,1 Marco Innamorati,1 Elisa Ambrosi,1 Gloria Giordano,1 Paolo Girardi,1 Roberto Tatarelli,1 and David Lester3
Report comment
I think it would be helpful for everyone if people would make a concerted effort to listen to those who have ADHD and are wearing “a new pair glasses” that make all the difference. I have never seen one person who has come through battling ADHD interviewed by an impartial journalist or anyone else. Not one time. We have something to say and we are ignored. Experts and pundits voice their opinions everywhere even as we are left out in the cold. No one says to us, “Tell us what happened to you. Tell us your story. What was it like having to deal with this misunderstood, damnable disorder all your life? What is it like now that you can pay attention? How does it feel?” We can shed light on the topic and people might learn a thing or three from us. What would it hurt to give us a voice?
Report comment
You are absolutely welcome to tell your story here. We value all voices of anyone who has been through the system and want to hear how things look to you. At the same time, it’s very important to remember that others have had different experiences than you have had, and that you owe them the same level of respect that you are asking. Different people have different experiences, and hearing that one or two or ten or a hundred people feel their lives are turned around by by stimulants doesn’t alter that one or two or ten, or a hundred people share having experienced harm or confusion with the same approach. It also doesn’t alter the statistics and scientific studies about the overall results of stimulant treatment on the whole group of people diagnosed with “ADHD.” You may learn a thing or three from them as well, and it might help you not take it personally when other people’s description of their experience is quite divergent from your own.
I hope that makes sense to you.
BTW, I HAVE seen objective interviews of people diagnosed with ADHD and treated with stimulants or some other approach, and have spoken personally to a large number of such kids. I can assure you that there is a very wide range of responses, some of which reflect your own, some of which are more lukewarm, and some of which reflect feelings of resentment and betrayal. For instance, I worked with a ten-year-old foster kid who was put on stimulants while in foster care, and I asked her how she felt about it a year and a half or so after she was put on the drugs. She said, “Well, I guess it did help me focus better… but on the other hand, maybe I was just going through a lot of stuff at that time.” I would ask you to reflect on why she might not have been as enthusiastic about stimulants as you are. Food for thought.
Report comment
You pointed out that you interviewed kids and how their reaction to stimulants might surprise me. I know people respond differently. Not my point. Your interviews were not broadcast or transmitted on major media outlets or written down word for word and published in TIME or NEWSWEEK or the NYTs. The Big Media has never reported the breakthrough accounts so common among us.
As far as the Media is concerned, we don’t exist and that is a tragic, deliberate and an unfair miscategorization of adults and kids with ADHD. Deception through silence.
You continue to make the point that not everyone has the same outcome. I am aware of that. My point is that we do not hear about the success stories. My point is, the Big Media doesn’t run genuine human interest stories regarding the nearly miraculous results many of us experience. That is my point. No one in the Big Media wants to hear from us. We’ve been to hell and remained there a long time. We came through it and to me that is something worth reporting on.
Report comment
I completely disagree with you. My experience is that the “success stories” are the only thing you ever hear in the media, and that those who have problems with this approach are silenced. Sure, there is the odd “horror story” that is sensational enough to make the news, but the idea that “ADHD” is a “neurodevelopmental disorder” that affects millions of children and can be specifically diagnosed (usually implied that “brain scans” or a response to stimulants are diagnostic) is almost never, ever questioned in the mainstream media. There are plenty of “celebrity stories” (Ty Pennington, Simone Biles, Michael Phelps, Justin Timberlake, Jim Carey, Howie Mandel) where the message is “Stimulant treatment saved my life.” I can’t think of one celebrity who has come out saying, “I tried this stuff but it really didn’t work for me” or “They tried to say my kid had ADHD but he moved to a new school and things went much better.” You’re welcome to prove me wrong by getting me some of these stories about how stimulants don’t work or made things worse or weren’t needed because X was really the problem, but that’s not what I see in the media at all. Seriously, I can’t think of a single story off the top of my head where such a story is told. I’m open to hearing evidence to the contrary.
But my point was not about Big Media, it is about each of us being willing to accept it when other people have different experiences and don’t agree with our own viewpoint. My initial impression left me wondering if you’d be open to hearing things that don’t fit with your own narrative experience. But I could be wrong. Everyone’s entitled to their opinion here, and we all have to respect each others’ views, even when they disagree with us, as long as it is done civilly and with respect for the diversity of experience that exists in the field.
Report comment
Thanks for your input. We see things differently. Best wishes.
Report comment
In other words, you know of no such stories you can share. Your are unwilling to support your claim with data, yet expect others to accept your claim or else they are “not hearing your voice?”
This is not a matter of viewpoint. Either the media is slanted toward success stories or it is not. I’ve given a long list of examples of that slant. You claim I am wrong. Where’s your data?
Report comment