The following article is based on hundreds of cases seen in the layperson psychiatric drug withdrawal community. But, don’t take my word for it. You can find hundreds of these stories on online forums such as Surviving Antidepressants, Benzo Buddies, or dozens of Facebook groups such as Cymbalta Hurts Worse, EFFEXOR (Venlafaxine) Tapering, Discontinuation Syndrome and Protracted W/D, or Lexapro: Support, Withdrawal, Recovery. Psychiatry has the opportunity to learn from our online communities to better care for the many people who wish to stop taking psychiatric drugs.
We are conditioned to believe that the medical system has all the answers to our mental and physical health concerns. But for people taking psychiatric drugs and who want to come off, traditional systems may unnecessarily harm them further. Patients who are prescribed antidepressants, antipsychotics, benzodiazepines, mood stabilizers, and/or z-drugs often seek help from detox facilities and hospitals with psychiatric wards when their regular providers aren’t knowledgeable enough to assist. But these places are not qualified to help people who want to deprescribe.
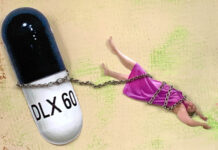
Like the thousands of formerly trusting consumers in the online forums, the pattern seen in online communities goes a little something like this: A person goes through something hard—a bad job, a divorce, the death of a loved one, a trauma, an inability to sleep, or an inability to handle major stress happening in their lives. They make an appointment with their family doctor or, less often, a psychiatrist. The doctor prescribes something for the symptoms, usually an antidepressant or anti-anxiety drug. In the following months, many will start to feel side effects that may mimic mental or physical illnesses. Their doctor will fail to recognize the symptoms as possibly being caused by the drugs they previously prescribed. When the patient reports these new or worsening symptoms, the prescriber will either raise the dose of the current medication, switch the patient to a different medication (in the same class of drugs or in another class), or add more medications (prescription cascade).
 Many months will pass. The patient’s medication dosages have been increased, they have been put on or taken off multiple medications, and they may suddenly find themselves on three to 10 drugs at the same time. Antipsychotics are often used for sleep (an off-label use) if benzos or z-drugs aren’t being prescribed.
Many months will pass. The patient’s medication dosages have been increased, they have been put on or taken off multiple medications, and they may suddenly find themselves on three to 10 drugs at the same time. Antipsychotics are often used for sleep (an off-label use) if benzos or z-drugs aren’t being prescribed.
At some point, the patient feels awful and doesn’t know what’s happening to them. They may have symptoms that are so severe that they feel like they are “dying” or that their nervous systems are “completely fried.” They don’t know if the adverse effects are due to their original condition, from the cocktail of medications they are now taking, or from some new, emerging “illness.”
This is when their healthcare utilization often increases. Patients will often go on a wild goose chase searching for the cause of their awful symptoms. The patient is subjected to MRIs, CAT scans of their brain or other areas of their bodies, blood tests, and visits to multiple specialists like rheumatologists and neurologists. All the while, the patient continues taking the drug(s) that have been causing their problems.
Eventually, the patient gives up the wild goose chase of seeing doctors, of trying new meds and stopping others, and subjecting themselves to more and more testing. They feel scared and hopeless, but their intuition or just how terrible they feel will tell them that they need to get off the cocktail of medication they are on, ASAP. After anything medically serious has been ruled out, the patient may finally realize that the medication they are prescribed is not working and/or is making them feel worse.
The Detox Problem
Detox facilities are not trained to deprescribe psychiatric drugs. Through the years, patients have figured out that hyperbolic tapering may be the best method to reduce the severity and length of withdrawal symptoms and to ensure the best chance at a successful taper. This process can take months, and in some cases, years, for a patient in a polypharmacy situation. Hyperbolic tapering is not appropriate for residential detox programs where twelve step programs, addiction language, and fast detoxes are standard of care. Insurance companies would not pay for the length of stay or appropriate support needed for a patient coming off psychiatric drugs slowly. Successful tapers are best done on an outpatient basis where the patient is in control of the rate and method of taper with support from a knowledgeable prescriber. Peer support from others who have gone through the process is also needed (and available online 24/7; see the forums listed at the top of this article).
Oftentimes, detox facilities reassure patients that they are “the most knowledgeable in the field” or “specialists in benzo withdrawal.” Because training in deprescribing psychiatric drugs is so poor, most facilities approach it like opioid or alcohol detox where patients are given “supportive medication” (like clonidine, valium, or beta blockers) and rather roughly torn off their drugs, without much regard for withdrawal symptoms. The patient might do okay for the first few days, until eventually, all hell breaks loose. Many will suffer the severe central nervous system destabilization (heart palpitations, sensory hypersensitivity, suicidal thoughts or akathisia) and may have to sign out of the facility against medical advice (AMA). This means they will not receive any prescriptions for medications they were given while at the facility. In many cases, these patients receive large hospital bills and leave with more prescriptions than what they were admitted on.
The Psych Ward Problem
Patients coping with a polypharmacy situation who turn to their psychiatrists, general practitioners, therapists, or hospital emergency wards may be in trouble, too. Whether the patient is suicidal or their doctor suggests psychiatric wards as a good place to “stabilize,” doctors there often take patients off drugs abruptly and/or will start new medications, increasing their polypharmacy problem. For example, a person may be taken off one of their antidepressants and a new one started. A medication for sleep may be replaced by an antipsychotic (whether or not the person is psychotic—usually they are not), or an anti-anxiety medication will be stopped and replaced with an antidepressant or a mood stabilizer. Sometimes, new diagnoses are given as well. Then, the patient is released within a few days and sent home after the doctor believes the patient to be stable.
Usually, a few days is not enough time to know whether a person is truly “stable,” as evidenced by the prevailing guidance that it can take 4-6 weeks for a drug to start “working.” But, this is one of the reasons doctors say they have “never seen people have a hard time coming off.” They aren’t asking the right questions while patients are inpatient, there is no follow-up from psych wards back to the community, and psychiatric drug withdrawal symptoms are misdiagnosed as “relapse” or a new illness when they are seen. Further, the mental health industry does not track patients long-term to see whether their interventions are truly helpful or not. Once discharged, patients are back home left to deal with their polypharmacy nightmares all on their own and they will often turn to our online communities for help. Patients find support forums usually from a simple Google search like “benzo withdrawal” or “fluoxetine withdrawal.”
In the online communities, patients find out that their strange physical and mental symptoms may be due to the medications they are taking and will see them spelled out in full detail, by other patients in the same situation as themselves. They are offered ways to cope with their symptoms, they find hope, and an exit plan off the drugs. They see success stories of patients healing and restoring their health, usually without the support of any medical professionals.
The Solution
Psychiatry is at risk of losing any credibility they have left by continuing to ignore the gaps in support for people who choose to deprescribe because of iatrogenic harm or otherwise. Perhaps some prescribers are not aware of their patients’ paths through the medical system, or detox and psych wards. A vast majority of practitioners have no knowledge or training about psychiatric drug withdrawal and protracted withdrawal syndromes. Patients are too afraid to go back to the providers who have caused them harm, are gaslighted when they do, and are afraid to talk about it for fear of losing their prescriptions they need to taper safely at their own speed. Are these the outcomes that psychiatry wants? With no movement towards safe deprescribing happening at any level of the mental health industry, the knowledge about how to taper successfully, and how to cope with severe symptoms, lies in the layperson withdrawal community.
Is abandoning responsibility to the layperson withdrawal community the best strategy? This strategy does allow patients to keep control of their tapers, at their own speeds, using the collective wisdom passed on from patients before them. They cope with the severe symptoms quietly in their own ways, in the safety of their homes without the threat of further hospitalization or forced medication. This prevents further polypharmacy by psych wards and abrupt cessation in detox facilities. But, abandoning the responsibility for deprescribing to the layperson withdrawal community allows the harm to continue in an echo chamber. Every day, the online support forums are seeing more patients coming for assistance in withdrawing from psychiatric drugs. In 2021, the Facebook groups reported a 5.24% growth in members joining drug-specific groups in search of sound advice for deprescribing. Lexapro, Seroquel, and Lithium withdrawal support groups saw a 10-15% increase in new members.
The American Psychiatric Association has long ignored deprescribing as a legitimate intervention when patients are not doing well on their current medications. There must be more continuing medical education (CME) training that includes differential diagnosis of adverse drug effects versus psychiatric disorders, prevention and deprescribing of harmful polypharmacy, safer prescribing and deprescribing practices, shared decision making, informed consent, and patient-directed hyperbolic tapers. Outpatient deprescribing clinics must be funded and research conducted. Medical school curricula must contain best practices (as learned from our communities) for safe deprescribing. These paradigm changes are long overdue.














This article is excellent, summarizing the same pattern from many personal stories I have read from Mad In America. Thank you Angie. Also I watched the documentary Medicating Normal; it was awesome!
Report comment
Thank you for reading and for your support!
Report comment
I wonder if psychiatry is even anything at this point. It is only being held up by misguidance, misinformation, the lack of comprehensive societal awareness, and money.
All people need is a place to detox of the psychiatric drugs, but money does not flow that way.
Report comment
How the behavior of the psychiatric community — from the lack of informed consent to the gaslighting and abandoning of patients, accompanied by a range of more tools of harm (ECT, forced “treatment”, personality disorder diagnoses, charges of patient non-compliance and the like) is not treated as criminal behavior is beyond me.
This article sums it up very well — the systemic abuse and abandonment of people they were paid to help. I hope more people get access to this information before the mental health system destroys more lives like it did mine and so many others.
I went through this hell of becoming sick from prescribed drugs and seeking help — often paying out of pocket — only to eventually accept that I was on my own with the damage. I wouldn’t wish it on anyone.
Report comment
Thank you for synopsizing this appalling psychiatric betrayal of their clients, Angie. Thank God for the internet, and all the wonderful psych survivors who are helping people wean off the psychiatric neurotoxins as well.
Report comment
This is an outstanding resource that has been needed by the withdrawal community for ages!
I and hundreds of my withdrawal community colleagues who founded and admin nearly every class psychotropic drug group or forum are repeatedly asked this question by our respective group memberships.
Are detox, rehab, recovery centers, psych wards etc helpful, safe and efficacious for psychotropic withdrawal?
Over the course of nearly a decade and hundreds of thousands of withdrawing consumers, we see mostly harmful outcomes from these facilities. Sometimes the very worst happens within a couple days once someone leaves them..
We will be sharing this valuable resource in our groups. Thank you so much for writing it!
Report comment
A well-thought, learner-friendly tool. You have anticipated the readers’ need for frames of reference. This would be a great seminar for first responders, anyone who is interested in people who take psychiatric medications, med-students doing rotations, parents, everybody.
When one of my daughters was not so long ago in a mania, following stress and onset of an inflammatory condition, the police officers were calm, thoughtful and kind as they sought connection with her frame of mind. She chose to go with them cheerfully and calmly to the psych ward. As the gathering of officers left the scene, I responded to a question about medication compliance with my recently gained information that a person in the throes of mania will metabolize their lithium faster and the level will fall. The officer expressed thoughtful appreciation for that info re: lithium; my point being that I have found the police officers to be compassionate and wanting to learn more about the details of medication and the needs of patients. I have seen that when the first responders are given knowledge of the needs of patients , they respond well and do their best. I would like for your keen insights to be made available to first responders in our area….BTW, I would also like to lift your summary paragraph and use it to introduce your article when I repost it.
Report comment
Perhaps, I was unclear. I think that first responders need the type of information that you detailed in order to understand better what is happening to patients.
Report comment
May I digress and suggest some things that would be far better than the drugs? Physically induced inflammation plus stress-induced inflammation (whatever source of inflammation) equals onset of hypomania which usually escalates, in our lived experience. Our understanding is that lithium does have anti-inflammatory properties. However, I have not seen any research that evaluates a holistic and anti-inflammatory response to mania, using lab tests if necessary and the best definition of Differential Diagnosis. We have seen that lithium by itself is rarely used to disrupt mania because it takes too long, i.e, several weeks. To hasten stabilization, the trial and error use of antipsychotic is used and if you are one of The Unlucky Ones then you can be left in a state of akathisia for weeks while the doctor “proves” the drug to see if it is therapeutic at the highest level; this sounds like and looked like covert and cruel research to me. This orchestrated failure of trials of one or more antipsychotics may be followed by coercion for ECT. ]Therefore, to reduce harm, why not be kind and try something natural other than chancy and torturous antipsychotic drug trials and ECT? ] In 2003 and again more recently a study reported that a solution of amino acids valine, isoleucine and leucine resolved mania, but that the beverage had an unpleasant taste, so why not use capsules? Why not use kindness, nutritious food, anti-inflammatory therapies , amino acids and whatever natural or safer things are indicated by a Differential Investigation and Diagnosis? Our culture has vast wealth for whatever PLEASES us. When we take pleasure in kindness it will be more lucrative than Disney.
Report comment
Admission to a psychiatric ward is reported to delay diagnosis of treatable medical conditions.
The mute roommate of my daughter who stepped close to my face and opened her mouth for me to see her black teeth and putrid green periodontal disease is a memory that raises the question as to how long it took for her to get the antibiotics and periodontal care that would have been prerequisite for mental health. I did report that condition to the nurse who walked into the room.
Report comment
It just occurred to me that the psychiatric end of Pharma has a lot to do with the 1%. Recently, We have seen Pharma shifting to new and provocative products, perhaps because the truth about psych meds is spreading virulently.
Report comment
Thank you, Angie, for your thoughtful and well-written essay. Yes, you get to the heart of the matter when you say that the psychiatric community has long ignored deprescribing as a strategy—-it’s mind boggling how doctors never seem to consider that maybe the drugs are causing harm rather than helping people. Yes, we need psychiatry to get on board with deprescribing and with more responsible tapering, but I am so grateful all of the online forums exist and that you are out there working to guide people through the process of getting off psych drugs. Kudos to you for your work!
Report comment
Hey Angie, Ellen here. Great article! I’m so glad to see you and your expertise here. Yes, we’ve learned a lot doing it ourselves. Now, if we can crack the Big Pharma wall between lived experience and practitioners, maybe we can get some compassionate support in the process.
Report comment
This is an important article. All too many people go to so called detox facilities and hospitals only to end up damaged and sometimes killed by the treatment. In a worst case scenario, one that I have seen a number of times, the people are hospitalized for a week or two during which time medications are rapidly tapered and stopped. Then the person is discharged the day after stopping the drugs, just as the worst problems from stopping the drugs are about to begin. I testified in a malpractice case about a woman in a hospital who rapidly stopped a benzodiazepine over about a week and then was sent home the day after her last dose. About 4 days later, while in the most intense part of her withdrawal, she made a near fatal suicide attempt (doctor won).
Most of the time a hospital based treatment just switches one drug for another. Most doctors don’t even know about prescription drug withdrawal and therefore assume that they know everything about it.
The flip side of this is that there are non-physicians who also don’t know much about withdrawal peddling unproven and ineffective withdrawal strategies. When things go wrong… they are sent to a (often clueless) psychiatrist.
If psychiatrists were educated about side effects and withdrawal effects, and gave patients informed consent, then most people would say ‘no thank you.’
I hope that this article is read by lots of people who might be considering going to a detox/rehab, as it will save them from a lot of misery.
Report comment
Thank you for this article. This is exactly what my husband is going through right now. Of his entire “cocktail,” his family and I think Olanzapine is the worst one and would like to wean him off. Can you recommend a reliable resource for us to consult? Thank you so much!
Report comment
Stuart Shipko says, “If psychiatrists were educated about side effects and withdrawal effects, and gave patients informed consent, then most people would say ‘no thank you’.
Unfortunately, this isn’t reality. Most psychiatrists have little knowledge or interest in side effects, and even less knowledge or interest in withdrawal effects. And whatever psychiatrists know about informed consent means nothing to them because side/withdrawal effects aren’t realities THEY have to deal with. Denial is the name of the game in psychiatry, so how can anyone trust psychiatrists, most of whom have neither brains nor scruples?
All they do is make more misery out of the iatrogenic mess they’ve already created (which they call ‘psychiatry’) with more evermore “diagnoses”, evermore “treatments”, and evermore “drugs”.
Keep psychiatrists out of it.
Report comment
And what does it mean to practice “good medicine”? It means having a current and extensive knowledge of side and withdrawal effects and how to deal with them, and a deep respect for and abiding adherence to providing informed consent to each and every patient. I think most m.d.’s make a good effort to do this. But not most psychiatrists, which explains the burgeoning cascade of iatrogenic illness that sure enough is becoming the new reality for too many people. So what does that say about psychiatry???
Report comment
This is such a great article, It outlines my own personal experience with medications in a linear way and frames it so well. I wish I had learned more about safe withdrawal and proper tapering before I went off many of my medications, I have had a lot of issues related to tapering at the “recommended” intervals and did not find the online communities in time. I just wanted them out of my body. I am grateful for your thoughtful examination of this topic and I think its extremely important to bring the topic of safer withdrawal and deprescribing into the consciousness of the medical community.
Report comment