Psychiatrists don’t utilize blood tests or brain scans to diagnose their patients. Instead, they rely on subjective observations about how their patients seem, and they listen to stories told by them to arrive at a diagnosis. Given our relative ignorance about how the brain functions, how does a psychiatrist know if a particular thought pattern, feeling or behavior is a symptom of mental illness? It’s estimated that the human brain—the most complex object in the known universe—contains about 86 billion neurons that interact in complex ways with one another and with other neurons in the central nervous system, and despite how much we’ve learned in recent years, consciousness remains an enduring mystery. So far no one has been able to cogently explain how the complex patterns of firing neurons give rise to our subjective, conscious awareness of the world.
Given these facts, how does anyone conclusively draw a dividing line between mental wellness and mental illness? What amount, degree, or kind of neurosis, psychosis or distress is normal? How do we know when a person’s behavior or their psychological and emotional state is indicative of psychopathology? What is mental illness? Is it a disease like any other, resulting from a structural or functional disorder of the body? Or is mental illness too often a phrase used to mistakenly pathologize and stigmatize the human condition itself? Isn’t it reasonable to suggest that the phrase scapegoats a person’s biological and psychological makeup as it discounts the role played by the environment the person inhabits?
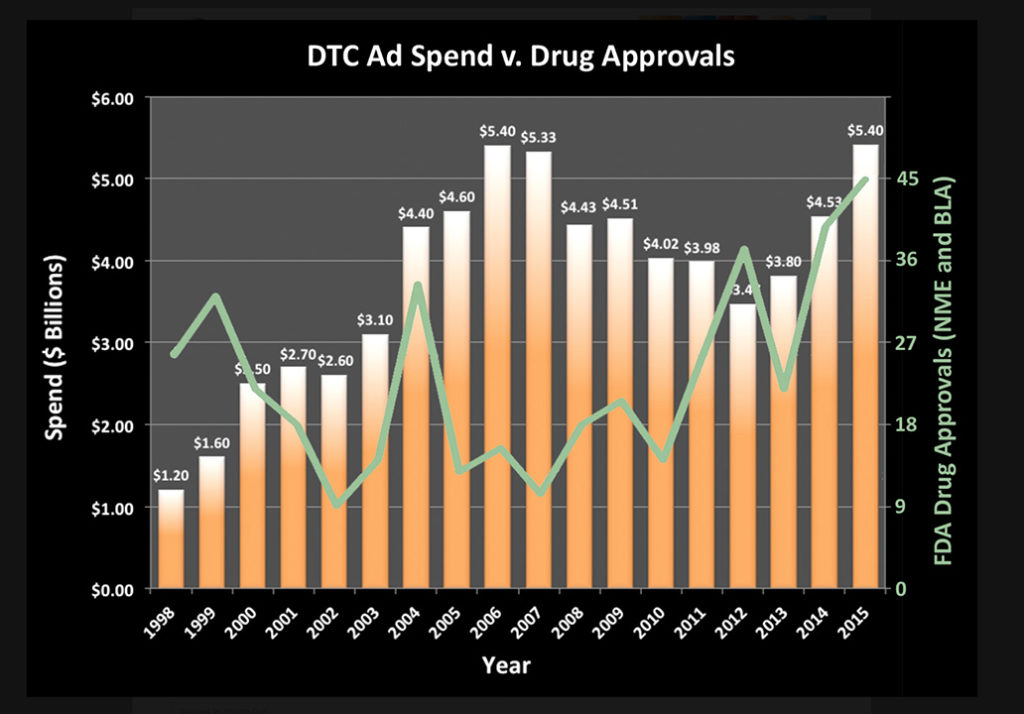
Two influential books that shape humanity’s understanding of what it means to have a mental illness are ones that most people have never heard of let alone ever read. They are the International Classification of Diseases (ICD) and the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (DSM). While cognitive liberty advocates challenge the inclusion of mental disorders within the pages of any catalogue of diseases, the stories told by psychiatrists citing the conditions defined in these nosologies are respected as scientifically-validated medical truths by many millions of people, in large part thanks to billions of direct-to-consumer advertising dollars spent propagating this narrative.
Effective, professional storytelling tactics are employed by for-profit companies marketing potent mind-altering substances to people experiencing anything from a lack of ease in life to paralyzing distress or despair. As a result, hundreds of detailed descriptions of different patterns of thinking, feeling and behaving are considered to scientifically define the bounds of what constitutes mental illness. While attempting to assuage psychic suffering with psychopharmacological treatments may be well-intentioned, evidence abounds that prescribing people these drugs serves to exacerbate their problems in many cases. For an unlucky few, psychiatric medications induce a condition called Neuroleptic Malignant Syndrome, which results in death on rare occasion.
A decade and a half ago, I was treated with a powerful psych med, against my will. Acting alone and empowered by the state, a psychiatrist stripped me of my inalienable rights of liberty and the pursuit of happiness, because he determined that I was in need of emergency psychiatric treatment for a life-threatening mental illness. He relied on information contained within the pages of the DSM to determine the illness ostensibly responsible for my behavior. Understanding how the DSM came to contain the mental disorder descriptions that it does is critical to apprehending why the APA has drawn the line separating mental wellness from illness as they have.
The story behind how the ICD and the DSM came to include certain mental disorder descriptions is a fascinating one. It was 1893 when the International Statistical Institute adopted the International List of Causes of Death. By the end of 1949 the World Health Organization published the sixth edition of the International Classification of Diseases or ICD-6. This version was the first to contain a section for mental disorders. Three years later, in 1952, the American Psychiatric Association’s Committee on Nomenclature and Statistics published the first edition of the DSM. As the APA’s DSM History website page explains, “It contained a glossary of descriptions of the diagnostic categories and was the first official manual of mental disorders to focus on clinical use. The use of the term ‘reaction’ throughout the DSM reflected the influence of Adolf Meyer’s psychobiological view that mental disorders represented reactions of the personality to psychological, social, and biological factors.”
Thirteen years later, in 1965, Sir Aubrey Lewis, a British psychiatrist responsible for the mental disorder section revisions of ICD-8, removed the word “reaction” from the mental disorder names. This seemingly insignificant nominal change represented a seismic shift in defining mental illness. Christopher Lane from Northwestern University, a 2005 Guggenheim Fellow, wrote about this seminal event in Shyness: How Normal Behavior Became a Sickness (Yale, 2007).
“The revisions to ICD-8 were bold, even cavalier, and had lasting consequences. Consulting few outside experts, a situation unimaginable a generation later, the person appointed to update the manual quietly eliminated the term reaction from many diagnostic labels. As a result, diagnoses like schizophrenic reaction, which in DSM-I had referred to sporadic psychiatric incidents, evolved almost overnight into schizophrenia, even if the person’s symptoms were rare or not especially violent. The same was true for terms like paranoid reaction, which the DSM-II task force determined henceforth would be known simply as paranoia. When I asked Robert Spitzer about these revisions, he confirmed my suspicions, ‘ICD-8 was written by one person, [Sir] Aubrey Lewis at the Maudsley [Institute of Psychiatry, London], and he didn’t have the word ‘reaction’ in the eighth edition, so DSM-II didn’t either. ‘No,’ Spitzer added, ‘there was no discussion at all’ on the DSM-II task force about the viability or consequence of adopting these changes. Turning phrases like ‘schizophrenic reaction’ into simple nouns (‘schizophrenia’) may seem insignificant. But as Spitzer concedes, it was a ‘major shift’ in approach, because it altered at a stroke the very meaning of illness for clinicians and patients.”
Robert Spitzer was a Professor of Psychiatry on the research faculty at Columbia University in New York City. In 1974, he became the chair of the APA’s task force responsible for producing DSM-III. Spitzer played a major role in leading a faction of psychiatrists on the task force to significantly revise and augment the number of disorders defined in the DSM-III, swelling the count of conditions contained in the growing catalogue by an eye-popping 46%.
| YEAR | EDITION | # OF DISORDERS | % GROWTH |
| 1952 | DSM-I | 106 | n/a |
| 1968 | DSM-II | 182 | 72% |
| 1980 | DSM-III | 265 | 46% |
https://en.wikipedia.org/wiki/Diagnostic_and_Statistical_Manual_of_Mental_Disorders
It has been a decade since Lane penned his assiduously researched and insightful account about this transformation of the APA’s diagnostic criteria. His explanation of how a small group of psychiatrists privately collaborated in the 1970s to revise the organizing document behind their profession is as amusing as it is unsettling. The incredible but true tale Lane tells about how shyness came to be viewed as an illness is more akin to political farce than erudite debate about how to classify different types of mental disorders, ostensible or otherwise.
Lane gained unprecedented access to the APA’s archives, and found documents detailing disturbing facts about the lack of scientific rigor employed while revising the third edition of this influential document. He frames the battle over this revision of psychiatry’s diagnostic bible as one driven by deeply-rooted internal conflicts within the field. Neuropsychiatrists argued for the radical expansion of the diagnostic criteria into many different disorders with specific symptoms while their Freudian colleagues favored a psychodynamic approach with fewer, and more broadly defined categories that recognized the biological, psychological and environmental factors that coalesce into human distress and despair. While neuropsychiatry clearly won this battle in the pages of DSM-III, Lane’s writing about the inner workings of Spitzer’s task force illuminate how a supposedly scientific process devolved into one guided more by individual personalities, professional agendas and profit potential.
Reflecting on the legacy of Robert Spitzer shortly after his passing in 2015, Lane wrote a blog post about a significant exchange between Spitzer and Isaac Marks, involving the inclusion of Panic Disorder in DSM-III as a stand-alone illness. Marks, “the world-renowned expert on panic, fear and anxiety” was flatly against the inclusion of Panic Disorder as a separate illness. From Lane’s blog post:
“Though committed to treating and understanding panic, Marks was steadfastly opposed to its being represented as a stand-alone disorder. He was similarly opposed to the formal identification of Social Phobia/Social Anxiety Disorder as a separate disorder, not least after seeing his own research on the subject (pointing to a different conclusion) cited as a reason for the change. The evidence that Social Phobia should be separated off had not been overwhelming and little had been published since that implied otherwise. But on both counts, Marks was overruled. ‘The consensus was arranged by leaving out the dissenters,’ he said to me ruefully, after Spitzer had told him in the men’s room at that key Boston conference that he ‘wasn’t going to win. Panic [disorder] is in. That’s it.’ ‘Never mind about the pros and cons intellectually,’ Marks continued, characterizing Spitzer’s apparently cavalier rejection of his expertise and objections. ‘Don’t confuse me with the data. It’s in.’
The Boston conference had been paid for by Upjohn Pharmaceuticals, maker of Xanax, a drug that became widely prescribed for Panic Disorder. As the CEO stood up to give his opening remarks, Marks recalled, he admitted quite openly: ‘There are three reasons why Upjohn is here taking an interest in these diagnoses. The first is money. The second is money. And the third is money.’ Despite concern that his research was being misused, to ends he could not support, Marks was, he said, ‘disinvited’ from subsequent discussions. Panic Disorder and Social Phobia/Social Anxiety Disorder weren’t just included in DSM-III, but, as he feared, given such low diagnostic thresholds (including, in 1987, public-speaking anxiety for SAD) that millions of American adults and children became eligible for a diagnosis, with Xanax, Paxil, and other medication among the most frequently prescribed treatments.”
After-the-fact reflections of people involved in the DSM-III task force reinforce the notion that the conditions described by the disorder names within the book are unlike other diseases that plague humankind in obvious and important ways. “There was very little systematic research [involved], and much of the research that existed was really a hodgepodge—scattered, inconsistent, and ambiguous. I think the majority of us recognized that the amount of good, solid science upon which we were making our decisions was pretty modest,” said a consultant on the revision task force. Others involved commented that, “The poverty of thought that went into the decision-making was frightening… In some cases, the people revising DSM-III [were] making a mental illness out of adaptive behavior.” In 1984, four years after DSM-III’s publication, psychiatrist George Valliant warned that the “disadvantages of DSM-III outweigh its advantages,” characterizing the revision as one that “represents a bold series of choices based on guess, taste, prejudice, and hope.”
Presuming that someone has an illness because their behavior is consistent with a disorder description contained in the pages of the DSM requires an audacious leap of faith given how little we understand about the brain, and what we do know about the lack of scientific rigor employed while updating this influential nosology. How the APA explains why people think, feel and behave as they do guides how millions of people frame the problem associated with certain types of human suffering. Please consider adding Lane’s Shyness to your reading list to learn more about how the APA task force responsible for DSM-III transformed the way people think about mental illness. In the meantime, enjoy this interview with Lane where we discuss what led him to write this book a decade ago, and why the story he told and questions he posed are still relevant today.
* * *
What prompted you to write Shyness: How Normal Behavior Became a Sickness a decade ago?
A combination of factors, really, that collided more or less simultaneously. As a university teacher, I kept hearing from students prescribed medication for anxiety and stress who were not at all sure the meds were necessary or, for them, the answer. Several spoke with disbelief about the ease and speed with which they’d been given a prescription—invariably for an SSRI, as this was the mid 2000s. Others worried about side effects and the DSM diagnosis longer-term. When the number of students reached a critical mass, I decided to dig deeper.
What did you find?
In hindsight, having heard of colleagues who never got anywhere with the APA, I was frankly lucky to be given unrestricted access to the DSM-III, -IIIR, and –IV papers. Put some of that down to dogged persistence: I kept bugging Robert Spitzer about the precise whereabouts of the papers, insisting on their importance as a key chapter in the history of American psychiatry. At one point, he implied that everything had been lost when the APA moved from downtown Washington D.C. to Arlington, Va. But eventually he relented, advising the APA that I should have a chance to review the papers. When, on arrival, the organization’s librarian said I could photocopy anything I needed, pointing to a nearby machine, I gathered up all the files I could locate on the Anxiety Disorders, Personality Disorders, depression, diagnostic criteria, minutes, votes, you name it, and, to the surprise of a few colleagues waiting, looked on with attempted casualness as my precious copies stacked up into an enormous pile. I’ll never forget the day the APA consented to their partial publication; everything was so accurate and well-documented in the book that they couldn’t say no.
That’s quite a coup for you, with results they weren’t anticipating. What happened next?
Once the extent of what I’d copied became clear to them, Spitzer himself and other influential figures granted me follow-up interviews, to present their side of the story. As I’d made known at the time, I had records of even individual votes for the approval of major diagnoses, and correspondence among key participants often pointing to vast, even fierce disagreement about diagnostic criteria, how (and whether) to turn into a condition what they thought they were describing, and even whether the syndrome itself existed beyond their sometimes raucous meetings. Occasionally, they would trade insults by diagnosing each other with the condition they were trying to formulate—that was fairly amusing! Yet, with just a few exceptions, the proposed disorder would wind up in the manual, with the loosest criteria imaginable—a consequence, I’d say, of Spitzer’s trying to keep everyone happy and onboard. Knowing that DSM-III was later touted as groundbreaking, scientific, and evidence-based, you’d need only look at the correspondence and the flimsy justification for inclusion to conclude that it was clearly nothing of the sort.
What led you to be curious about how the DSM-III came to be?
I’d already written quite extensively about the history of psychiatry, psychoanalysis, and medicine since the nineteenth century, and had followed developments such as the 1973 decision to remove homosexuality from the manual. Though it seems incredible to say so today, at the time that decision was quite controversial and fiercely contested by conservative psychiatrists such as Charles Socarides, who were apoplectic about the move.
And what about Spitzer’s role in that development?
Spitzer himself was quite canny in navigating the turmoil and turning himself into the hero of the hour—he was given stewardship of DSM-III as a reward. Part of his compromise with the conservatives, though, was to float “ego-dystonic homosexuality,” which over time became Gender Identity Disorder. So it’s not as if he was depathologizing homosexuality entirely, as some like to think—we know this from his later research flirtation with Reparative Therapy, for which he subsequently apologized. To my mind, there was still a major lesson to learn from his seemingly insatiable appetite for adding more and more disorders to DSM-III and –IIIR. During meetings, he would tap out their criteria on an old manual typewriter while his colleagues sometimes shouted over each other to nail down their precise characteristics. Students joked at the time that he never met a disorder he didn’t like.
How important was your Guggenheim fellowship in the process of researching and writing the book?
Besides my doggedness, the fellowship was a key reason Spitzer and the APA relented in granting me access to the papers. Since the Guggenheim Foundation was funding much of my research and clearly favored transparency, the onus was on Spitzer to avoid seeming as if he was thwarting discovery. He also cared greatly about his legacy and wanted very much to be seen as having rescued the DSM from imprecision and mediocrity. The historical record is not nearly so flattering—his decisions, frequently determining the number and phrasing of criteria, often come across as questionable and arbitrary.
People find hope and even peace, not to mention community, in part, by subscribing to the biomedical narrative of mental illness propagated by the APA in the DSM and by the manufacturers of psychiatric drugs in their ads. You don’t question that people suffer. You do write about a concern about the impoverishment of the human experience due to the medicalizing and treatment of normal emotions and behaviors. Should people experiencing a normal degree of distress or despair in life who are lucky enough to feel better as a result of taking psych meds consider not taking them out of a concern for the diminishment of the human experience?
That’s a great question—and to this day a somewhat fraught subject for debate. Back in 1972, the Cornell psychiatrist Gerald Klerman took issue with what he called “pharmacological Calvinism,” which he characterized as the position: “If a [pharmaceutical] drug makes you feel good it must be bad.” You can detect a fair amount of defensiveness in his approach but, even so, I wouldn’t recognize myself in any such characterization.
So, what for you are better questions to ask?
Not just: Are the meds truly necessary? But: How are they functioning therapeutically? Is the influence strictly pharmacological or does it pale beside the fascinating, often astonishing strength of placebo? And does the possibly minor drug benefit outweigh the very real risk of harm, over not just one lifespan, but generations. From there, the questions for me balloon to an even-larger scale: Is the widespread prescribing of meds for relatively mild conditions changing us culturally and cognitively? Is it altering our tolerance for pain and influencing my students’ attention spans? Where do we draw the line over so-called “enhancement”? How do we differ cognitively and culturally from nations with tighter controls on prescribing? And are U.S. definitions of mental illness and health influencing those of other countries, to the point of exporting models of illness and setting a kind of planetary standard for mental health? You think back to the DSM-III correspondence as the yardstick for supposedly watertight scientific terms and then find articles with titles such as “Social Phobia in Saudis” that underscore that the decisions had truly global consequences. Just as well we’ve been able to document them carefully and decide for ourselves about their underlying validity.
What’s inherently wrong, if anything, with naming as many kinds of behavioral problems a person can have as possible, so that highly trained medical professionals are in a better position to help more people contend with more problems in highly convenient ways, like taking a pill?
The struggle to name something precisely is clearly a medical necessity, for physicians and patients alike, and one spanning centuries not just recent decades. But to answer your question better, just consider the example you cited earlier of Sir Aubrey Lewis, editor of ICD-8 (the basis for DSM-II), single-handedly deleting the word “reaction” from diagnoses such as “paranoid reaction” and “schizophrenic reaction.” In both cases, the term “reaction” indicates that the situation is dynamic, possibly short-lived, and tied to context or particular stressors (environmental, income-related, doubtless exacerbated by job-loss, homelessness, and so on). With the renaming of those conditions as “paranoia” and “schizophrenia,” all sense of reaction is lost at the stroke of a pen, it becomes much easier to imply that the conditions are innate and potentially lifelong; their recurrence will also seem closer to relapse than the repetition of a particular stressor. And with the rise of the term “disorder”—e.g., “depressive disorder,” “social anxiety disorder,” even “passive-aggressive personality disorder”—the not-so-hidden implication is that the root of the problem is biological/genetic rather than social/environmental. In short, how we describe something—especially in psychiatry—is profoundly deterministic.
What about the broader consequences of errors over naming?
While there’s a fundamental need in medicine to name phenomena accurately, to minimize errors and misdiagnoses, psychiatry (despite many of its best intentions and well-publicized fantasies) is not an exact science. It’s often profoundly inexact in its grouping and characterization of traits, propensities, behaviors, and persons—profoundly normalizing at the same time, too, as definitions of pathologies and norms go hand-in-glove. And psychiatry has tended consistently to loosen its diagnostic criteria over time, lowering the threshold for illnesses and making it far easier to receive a diagnosis for one. In the book, to take just one example, I look at the implications of the shifting terminology from “anxiety neurosis” to “social phobia” and then to “social anxiety disorder” and how, though psychiatrists think these all add up to the same condition, they in fact reference and target quite different behaviors.
Finally, in psychiatry you often find an attempt at retrospective ratification, with articles supporting a DSM diagnosis carrying titles such as “Did Samson Have Antisocial Personality Disorder?” and studies of phobias asserting, without skipping a beat: “Hippocrates saw people with many different phobias over the years, ranging from agoraphobia and social phobia to animal phobias and other fears still common today.” Consider the historical flattening involved in such a sentence! The effort makes it possible to weave past incidents into recent discoveries and newly revised theories, to make them all seem seamless and mutually affirming.
Many popular mental health advocates actively promote the APA’s biomedical diagnostic narrative of mental illness. They often speak or write with certainty about suffering from a disease of the brain as a result of being diagnosed with a mental disorder by a psychiatrist. I’ve found it difficult to open up conversations that challenge the veracity of claims implied by this biomedical narrative. Any suggestions?
Those kinds of conversations can be really challenging, especially with the scale of financial backing for the biomedical approach, pretty much at the expense of all others. Human nature being what it is, it probably wouldn’t work to ask your interlocutor: “Did you know that some DSM disorders now liberally bestowed on hundreds of thousands of us stemmed from a single advocate touting their need for inclusion on the basis of just one patient they had personally treated …?,” and only reported as such anecdotally, with a record that cannot be verified. Perhaps the advocates were in fact referring to themselves—it’s impossible to say or rule out. At the same time, I do think that once-popular metaphors such as the “broken brain” and a “chemical balance” have been debunked quite effectively—you don’t hear much of them these days, even in pharma ads, which are the last to change. Many biomedical advocates have become far more circumspect, and that’s both appropriate and potentially useful. Even recent news that the gene-editing program CRISPR has led to the multiplication of all kinds of mutations could slow the stampede toward the biomedical, though I doubt even that could halt its progress entirely.
Four years ago, Dr. Thomas Insel, Director of the National Institute of Mental Health marked a seismic shift in the course of mental health care history when he announced that the NIMH would no longer fund research oriented solely on DSM categories. You called it a “humiliating blow to the APA” and noted that, “the manual’s authority won’t end overnight, but, given the implication of the NIMH’s decision, it also can’t and won’t stay as it has.” I’ve engaged with a number of different popular mental health advocates on social media who have no idea that this event ever occurred. You note that little is likely to change unless the APA and the amounts of money being pumped into pharma direct-to-consumer advertising change. In light of the continued rise in DTC pharma advertising, how do you foresee the authority of the DSM, as measured by the prevalence of the use/acceptance of its disorder names, changing in the years to come?
That’s a great question and goes to the heart of a big issue. Insel was to a large extent faulting the APA leadership for being insufficiently biomedical. He argued, just days before DSM-5 was released—obviously frustrated by its tepid reforms but also I think in a bold pre-emptive gesture—that DSM descriptors suffered from a “lack of validity” because they were fuzzy about etiology in a way the NIMH apparently was not. According to NIMH criteria, “mental disorders are biological disorders involving brain circuits that implicate specific domains of cognition, emotion, or behavior.” When seen in that way—despite all the hype, vast sums of money, and false hope surrounding biomarkers for mental disorders—the NIMH was clearly trying to narrow the gap between itself and the APA, to force the latter to embrace biological psychiatry even more conclusively than it already had. To that end, future editions of the DSM could—if the APA wanted or needed renewed NIMH support—become even more one-sided in their adherence to biomarkers, clearly a worrying scenario.
So, was DSM-5 worse in this respect than earlier editions?
DSM-5 stopped short of including many of the worst proposals that had circulated widely beforehand, such as Attenuated Psychosis Syndrome and Mixed Anxiety Depression, partly because of well-targeted pushback, but also, I think, because the APA—hitting a limit internally over consensus—opted to double-down on the framework and associated problems of DSM-IV. I’m not ignoring that Disruptive Mood Dysregulation, Binge-Eating, Hoarding, and Somatic Symptom Disorder were all included for the first time, with Internet Addiction added to the Appendix. But they were added in a climate of intense skepticism, including at long last from the mainstream media, and it would seem the APA stopped well short of where it wanted and hoped to be. That skepticism is in future likely to be as fierce and well-organized as it was over DSM-5, so the days when the APA could approve dozens of poorly defined disorders at more or less the drop of a hat appear to be over.
Do you think the Research Domain Criteria for diagnosis holds any promise for helping people in need, or do you think its biomedical orientation is systematically the wrong way to address certain kinds of human suffering?
I’m not willing to rule out that, decades hence, biomarkers might hold limited diagnostic value for people in need, just as I’m not willing to downplay the role and influence of the brain in discussion of psychiatric treatment. Still, as Stanford’s John Ioannidis made clear in 2011, in his devastating exposé of the overselling of biomarkers, many well-regarded studies have consistently overstated links between biomarkers and psychiatric disorders, including by selectively reporting only positive findings and exaggerating associations between illnesses and the genes said to influence and cause them. Having written quite a bit about the ethics and falsehoods of “early detection” in psychiatry, including that such an emphasis has medicalized childhood and even infancy, with all kinds of knock-on dangers from powerful medications influencing unformed brains, I am firmly in the camp that the risks greatly outweigh the advantages and are, because of their scale and effect, unacceptable as a result.
Candidly, it also needs saying that biological psychiatry consistently underestimates the social and economic consequences of “early detection,” including the very real risks of stigma, lifelong medical dependency, self-fulfilling prophecies, and false positives driving the sort of dangerous levels of overmedication we’ve seen in ADHD diagnoses and with the consistent lowering of age thresholds for Bipolar Disorder.
Tens of thousands of newly diagnosed sufferers of Social Anxiety Disorder who have been handed a psych med prescription for the first time in their life are assembled in front of you. You have two minutes to tell them whatever you want. What would you say?
There’d be a lot to pack in in just two minutes! First, I’d assure them that social anxiety is widespread—that people commonly list fear of public speaking above even fear of death, which really tells us something. And, in essence, that the APA took those common fears and foibles (dislike of eating alone in restaurants, concern about hand-trembling while writing checks, even avoidance of public restrooms) and turned them into what would become, by the year 2000, according to the Harvard Review of Psychiatry, “the third-most-common psychiatric disorder, behind only major depressive disorder and alcohol dependence.” Just three years into the nineties, Psychology Today was calling Social Phobia “the disorder of the decade.”
I would remind them there’s almost a 50% chance a person will think of him- or herself as shy—a percentage that holds across a large number of countries and cultures, leading to widespread confusion between shyness and social anxiety, and that the latter has a long and well-established history—described in ancient Greece, discussed in the Renaissance, and analyzed by Victorians such as Darwin, who wondered, among other things, whether animals could experience embarrassment. Yet Social Anxiety Disorder (aka Social Phobia) dates to just 1980, when Robert Spitzer and a small group of carefully screened, like-minded colleagues decided, largely on the basis of just one article whose author vociferously opposed their move (and still does), to list it as a stand-alone mental illness. They did so, Spitzer told me, partly because they wanted alternatives to the existing term “anxiety neurosis,” which they thought too psychoanalytic and insufficiently focused on the brain. He added, in an aside, that they might have responded that the ICD continued to list the earlier term, in ways that would have challenged the APA’s apparent lock on nomenclature.
What about the pharmaceutical consequences of such changes?
Since the people in your example “have been handed a psych med prescription,” likely in this case for Paxil, given the diagnosis, I would find it necessary to add, without fear-mongering, that GlaxoSmithKline considered shelving the drug before subjecting it to a multimillion-dollar marketing campaign (post-DSM-III approval), because its trial results were so spotty; that they then hid from the FDA much of the associated negative data, including that as many as one-in-five patients had experienced serious, widespread side effects and withdrawal symptoms prior to FDA approval in 1999. And that the drug maker was subsequently required in 2004 to add a black box warning to Paxil indicating an “increased suicidality risk in children, adolescents, and young adults with major depressive or other psychiatric disorders,” as well as from an increasingly well-documented withdrawal syndrome that leaves many feeling worse than before they began treatment. All this for symptoms so routine and widespread they include fear of eating alone in restaurants! If nothing else, the data associated with the most-common pharmaceutical treatment for Social Anxiety Disorder put the condition’s routine concerns and common symptoms into stark relief.














To the Social Identity Disorder sufferers given benzos, I’d say- if you’re really worried, buy some magnesium oxide tablets and pay for them by selling your prescription drugs. You’ll not only be more likely to feel better, but you’ll have enough money left over to treat yourself to dinner at a good restaurant, and maybe have enough to even take a date to dinner.
Report comment
Great article, thanks! And “At the same time, I do think that once-popular metaphors such as the “broken brain” and a “chemical balance” have been debunked quite effectively—you don’t hear much of them these days, even in pharma ads, which are the last to change.” – see the Royal Australian and New Zealand College of Psychiatry’s website for the general public “Your Health in Mind” information on medication, which very clearly continues perpetrating these falsehoods – “How do medications treat mental illness? Medications work by rebalancing the chemicals in the brain. Different types of medication act on different chemical pathways.” I have directly emailed the president of RANZCP about this factual error and iatrogenesis of the falsehood (and shown them Lacasse and Leo 2015 paper – Antidepressants and the Chemical Imbalance Theory of Depression: A Reflection and Update on the Discourse.) But of course no response. So it continues… https://www.yourhealthinmind.org/treatments-medication/medication
Report comment
I agree, this myth is still firmly embedded in the public mind and continues to be propagated by many practitioners, whether out of ignorance or malfeasance or whatever. It appears on many websites across the internet. The tide does appear to be turning, but we’re a long way from having general agreement that this idea is mythological.
Report comment
I would hesitate on this subject before agreeing, if I could agree. Bio-medical psychiatry is as firmly entrenched as it has ever been. “Broken brain” and “chemical imbalance” may be falling by the wayside, but attributing disorders to genetic causation is only growing stronger, and now, with bogus “bio-markers”, you have an ingenious method of increasing drugs sales. Much of this creation of the DSM has been about reinforcing the status of the psychiatrist as a medical professional, and in that matter it has been highly effective. Seeing as the role of the psychiatrist is contingent upon seeing many common problems people face in life as medical conditions, I don’t see a way around exposing the mythology that that profession has developed around itself as a justification for its existence. I can’t say that there is nobody who is critical of psychiatry for having arisen in the first place. Regardless, people are going to come to that profession’s defense on the basis of perceived need rather than legitimate science, making one question whether that perceived need is enough to justify the entire endeavor, and thus, the pretentious masquerade.
Report comment
The “chemical imbalance” hoax is alive and well. The business of “broken brain” deception is booming. (See, for example: https://brokenbrain.com/trailer/) The myth of mental illness continues to thrive. Other justifications, such as the supposedly genetic origins of so-called mental illness, are also growing. These are all reasons why the dragon of psychiatry must be slain, and the myth of mental illness laid to rest.
Report comment
I’m afraid I don’t see the tide turning, at least not for the next decade. Because of the marketing of the chemical imbalance theory as fact, and because it has been insidiously linked to the destigmatization of mental health, I think most people assume support of the chemical imbalance theory is a social justice issue. Any questioning of psychiatry’s claims has been labeled pillshaming. In their rush to not discriminate against people taking psych drugs, my friends have inadvertently become highly discriminatory toward those of us who have been harmed the drugs and wish to speak out.
Report comment
I read an article saying that promoting the notion of the “broken brain” wasn’t decreasing stigma against psychiatric patients after all.
What’s noteworthy is the site where this was published. NAMI.org. The article is almost 10 years old.
Disgusting. 😛
Report comment
Yes I don’t think these myths have been debunked in the public’s mind at all.
Report comment
Evil will always defeat good–because good is stupid. ~Mel Brooks’s Space Balls
People love the idea that pills are the answer to all their personal problems. This lets them abdicate all responsibility for bad life choices. They don’t have to do squat to improve themselves when the friendly neighborhood dealer in a lab coat can hand out fists of happy pills.
This also lets them bum around watching TV and going to “clubhouses” where they can be treated like kids with really low IQs instead of working. No financial responsibilities!
Some folks like the system because they enjoy a lifelong adolescence!
Report comment
The myths are alive and well. The functions they serve are too valuable to allow a lack of scientific support to usher them away. Better to dismiss the lack of scientific support or pretend it doesn’t exist.
Rob, I couldn’t help myself from spending some time on the RANZCP’s Your Health in Mind website. Here are some things I learned in addition to the quote you posted stating that psychiatric drugs “work by rebalancing the chemicals in the brain.” The quotes below struck me as the most egregious contradictions between the flattering picture painted in the website and scientific/clinical reality. I offer them below without commentary:
1. Psychiatrists provide fully informed consent (https://www.yourhealthinmind.org/psychiatry-explained/whats-a-psychiatrist). For example, they “will only suggest treatments that are proven to be safe and effective.” For treatments they choose, they will explain: “why they recommend this treatment…how it works…what the side-effects are…any risks of the treatment…how much it costs. It’s up to you whether you agree to have the treatment.”
2. “In people with ADHD, there are differences in the parts of the brain that control our ability to plan, organise and focus” (https://www.yourhealthinmind.org/mental-illnesses-disorders/adhd-in-adults)/
3. “We know that bipolar disorder changes how the brain works, and this causes symptoms of mental illness.” (https://www.yourhealthinmind.org/mental-illnesses-disorders/bipolar-disorder)
4. “Newer antidepressant medications work by altering the amounts of natural chemicals in your brain, such as serotonin or noradrenaline.” (https://www.yourhealthinmind.org/treatments-and-medication/antidepressant-medication)
5. “ECT is safe, painless and very effective in treating depression” (https://www.yourhealthinmind.org/treatments-medication/ect). “It’s safe and there are few side effects…The risks are similar to any minor medical procedure given under general anaesthetic.” Adrian, an ECT patient, is quoted: “I’ve had severe depression for 16 years. Any short term memories I lose to get rid of that never-ending, crushing feeling of hopelessness and sadness are worth it, in my opinion.”
6. Regarding psychiatric hospitals (https://www.yourhealthinmind.org/treatments-medication/psychiatric-hospitals): “Sometimes a mental illness can become so severe that the person with the illness may not even realise they are unwell. If someone is so sick they don’t understand they need treatment, and if not having the treatment would put them (or others) in danger, the law allows that person to be treated involuntarily. This means they can be kept in hospital (if necessary) and treated, even though they say they don’t agree to it. To make sure this only happens when it’s absolutely necessary, the law requires that doctors present a case for this in front of a tribunal (or, in New Zealand, a judge)…Seclusion and restraint are a last resort where all other options to keep people safe have been tried or considered. Both should be very rare. The RANZCP’s position is that the use of seclusion and restraint should be reduced and where possible removed entirely.”
Report comment
Klerman’s accusation seems off. “If a drug makes you feel good it must be bad.” Most shrinks work on the opposite premise. “The worse a drug makes you feel the better it is for you.” No doubt it builds character. 😀
Psychiatry is Calvinism for Atheists. I’m not referring to asceticism.
Instead of a sovereign God who forces us to be good or evil, we have sovereign genes and neurological conditions. No room for free will in either case.
Report comment
I had a different take on the Gerald Klerman claim in that I tend to agree that that’s the way psychiatrists see it. I found neuroleptics made me feel terrible, and it wasn’t that they were saying taking this substance was going to make me get any better. The claim was that a person with a certain diagnosis would have to take these drugs for life, and they were drugs that made me in particular feel terrible.
I was also at one time given a so-called anti-depressant, and I didn’t think it did a thing for me. My doctor at the time said that my body had to adjust to taking the drug with time. Perhaps he thought of it as a happy pill. I felt I wasn’t depressed. I decided not to take the anti-depressant, and I think that was a wise choice. Had I not done so, not only do they have their own set of adverse effects, there would be withdrawal effects to consider if I’d ever tried to come off of them after continued use either with help or entirely on my own.
Report comment
Another great book to read on the topic of the development of the DSM is Gary Greenberg’s “The Book of Woe.” Francesco’s article is a great introduction to this book. The DSM is perhaps psychiatry’s most pernicious sleight of hand. I highly recommend Greenberg’s book for anyone who is seeking to understand the truth about psychiatry: https://psychiatricsurvivors.wordpress.com/2014/04/24/the-book-of-woe/
Report comment
Slaying_the_Dragon, is John Hancock your other non de plume? I notice you share his political ideologies.
Report comment
12 months ago my life was changed while an inpatient at at psych hospital. I was prescribed a combination of medications referred to as “California Rocket Fuel”. These medications changed my life as dramatically as a sightless person being able to see for the first time. In addition, I was also given Prozasin which stopped my nightly PTSD nightmares. Because of these medications, I have been able to work with therapists (currently an AWESOME art therapist). But before the medications I was unable to function to the point of planning on taking my own life. I am no longer hopeless, but rather hopeful. This is due to my family, medications and therapists. But I could never have moved forward without the medications as I was hopeless.
Report comment
You can’t see the paradox in your writing can you? If you are not sick you can not seek help(so you must be sick), you can not get attention you want ( who is paying?) Nightmares come from the unconscious mind , not a medical-physical illness, nightmare come froma fear or a guilty conscious that needs to be confronted, not drugged away.
Report comment
I’m happy that you have found your way out of hopelessness, and I support the right of people to find what works for them to be well – including psych drugs. My issue with the system we have to help suffering people stems from the fact that a person has to be diagnosed with a disease to access certain kinds of help.
It seems reasonable or normal to me that some people are troubled sometimes, after the fact, by traumatic events that they’ve experienced. It’s not easy being a human being, and I don’t think that a system that requires someone to take on the “sick role” in order to access help in dealing with the human condition is optimal.
Report comment
With PTSD, I would wake up screaming aloud almost every night for years. Reliving the horror every night, screaming so loud in my head while asleep trying to wake myself up and escape the horror. This reduces REM sleep, and the nightly fight was also physically tough. With the Prazosin I was able to begin talking with a therapist. At first this brought back the nightly screaming, so my dose was raised by my doctor. As I previously mentioned, I now see an AWESOME art therapist. I have painted pictures of the horror of my past. I am working to beat the horror. I am confronting the horror with my therapist(s). By painting the horror, and discussing my fear and guilt with my therapist, I am finally gaining power over the horror.
But without the Prazosin (used off-label non/FDA approved for PTSD), I could not physically do battle with the horror by painting it.
Report comment
You may be interested in Dr. Joanna Moncrieff’s distinction between a disease-centered versus drug-centered model for understanding the function of psychiatric drugs. The former is basically the chemical imbalance theory- that there is some biochemical deficiency which causes the emotional state, and that the psych drugs correct this, the same way insulin helps a type 1 diabetic. The latter acknowledges that there are many causes of distress, and not all are of biological origin. In this case psych drugs have a drug effect, like alcohol or marijuana, and that might helpful or harmful depending on the particular situation.
The former is a pretty uncritical view, and leads to exponential use of these drugs and an ingnoranc of their dangers. The latter is more truthful and leads to a much more careful use of psych drugs, and a greater awareness of their potential for harm.
In a drug-centered model, it doesn’t mean drugs can never provide any benefit ever for someone with PTSD. It just means greater awareness of what they’re actually doing.
Report comment
You have me thinking… and reading. The VA published a 2017 study that stated a 49% efficacy for Prozasin with PTSD nightmares.
And today, the NYT had an article: “Do Antidepressants Work?”
“The take-home message from these two studies was that the effectiveness of antidepressants had been overstated, and that the benefit might be limited to far fewer patients than were actually using the drugs.”
Report comment
PTSD is caused by emotional trauma. Not genetic inferiority or being an evolutionary throwback–the key premise to psychiatry (a field of eugenics.)
I’m glad you found these drugs helpful. They have some short term benefits as emotional pain killers. I felt better when I first took Stelazine in small amounts of 3 mg twice a day. If I had been told the truth–this will take the edge off your overwhelming anxiety–and taken off after say a month when my social issues had resolved it would have been a good thing not a bad. Like morphine for a broken leg.
Report comment
support of people rights
Report comment